

Aluisio Rosa Gameiro Filho1; Rafael Godoy2; Angela Rees1; Simona Degli Esposti1
DOI: 10.5935/0004-2749.2023-0064
Dear Editor,
Coronavirus disease 2019 (COVID-19) is caused by severe acute respiratory coronavirus 2 (SARS-CoV-2). Since the outbreak of this disease, several reports of associated ophthalmological manifestations have been published. They usually occur up to two weeks after the beginning of systemic symptoms; however, in 2.26% of cases, the eye can be the site of initial COVID-19 manifestation(1). Even though disorders of the ocular surface, such as conjunctivitis, keratitis, and episcleritis are the commonest findings in these patients, there are some reports of retinal involvement, mostly vaso-occlusive events. We report two cases of paracentral acute middle maculopathy (PAMM) associated with COVID-19.
Case 1
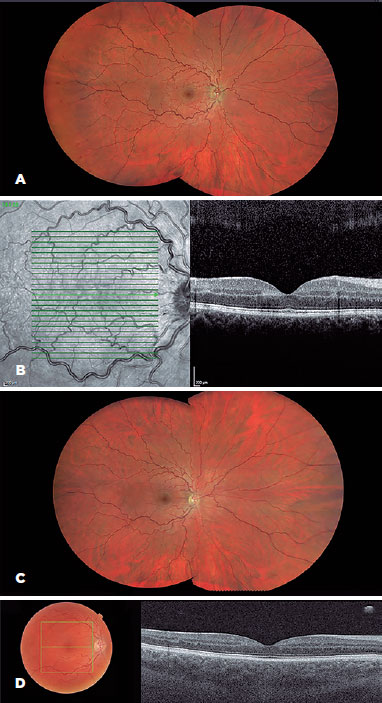
A 36-year-old man attended accident and emergency (A&E) complaining of painless visual reduction in his right eye associated with mild headaches, which had started 1 week before. Five days before, he had been diagnosed with COVID-19. He had received 3 doses of COVID-19 vaccine, with the last dose 2 months before the onset of symptoms. His past medical and family histories were unremarkable. The best corrected visual acuity was 20/80 in the right eye (OD) and 20/20 in the left eye (OS). His intraocular pressure (IOP) and biomicroscopy were normal. Fundoscopy showed increased tortuosity and dilatation of all branches of the retina central vein with some hemorrhages in the temporal areas, suggesting branch retinal vein occlusion (BRVO) in the OD. Fluorescein angiography revealed a delay in arteriovenous time, and optical coherence tomography (OCT) showed a hyper-reflective band in the inner nuclear layer (INL), suggestive of PAMM. After 1 month of observation, his visual acuity returned to 20/20 in both eyes. Blood test results showed normal levels of homocysteine and were negative for thrombophilia. The OCT findings also returned to normal (Figure 1).
Case 2
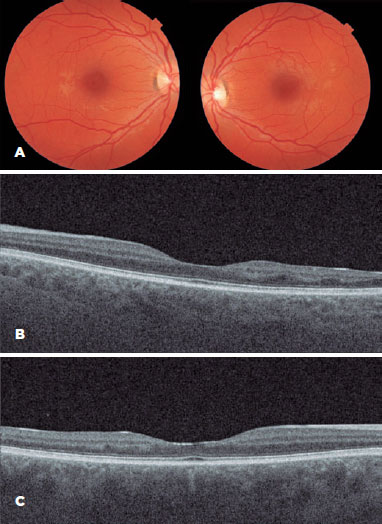
A 30-year-old female patient attended A&E complaining of floaters and scotoma in both eyes. She had recently been diagnosed with COVID-19 and was still breathless and weak on minimal exertion. Her visual acuity was 20/15 and 20/20 in OD and OS, respectively. Biomicroscopy and fundus examination were normal, and the patient was referred for a neuro-ophthalmological examination. OCT was performed, revealing PAMM in both eyes. Two years later, the patient has bilateral retinal INL thinning compatible with late PAMM (Figure 2).
COVID-19 is associated with a state of hyper-inflammation and hypercoagulability, causing thrombotic complications in several organs and tissues. First described by Sarraf in 2013, PAMM is a spectral-domain OCT (SD-OCT) finding characterized by band-like lesions visible at the level of the INL. It is considered the acute phase of ischemia in the intermediate and deep capillary process(2). It usually affects patients about 50-60 years old, with no gender predilection. This condition was previously associated with COVID-19 infection(3) and patients who received COVID-19 vaccination(4). COVID-19 is thought to cause vascular degeneration in the eye through several mechanisms: by direct viral entry into retinal cells via angiotensin-converting enzyme (ACE-2) receptors causing endothelial cell damage and thromboinflammation. When the virus-ACE2 receptor connection is established, the outer part of the receptor is released, leading to a downregulation of the receptor, causing a dysregulation in the renin-angiotensin system, affecting vascular constriction, proliferation, and the inflammatory status of the vascular tree(5); also, by downregulation of endothelial nitric oxide synthase, and abnormal vascular endothelial growth factor expression, inducing a cytokine storm(5); by inducing a deregulation of the autonomic system which controls choroidal blood flow(3); and through coagulation disorders, which can be detected by increased D-dimer levels(4).
The ophthalmologist should be aware of the association of COVID and COVID-19 vaccination, with retinal vaso-occlusive conditions, particularly in young patients with no risk factors for thromboembolic and vascular events.
REFERENCES
1. Aggarwal K, Agarwal A, Jaiswal N, Dahiya N, Ahuja A, Mahajan S, et al. Ocular surface manifestations of coronavirus disease 2019 (COVID‑19): A systematic review and meta‑analysis. PLoS One [Internet] 2020[cited 2022 Jul 27];15:e0241661. Available from: Ocular surface manifestations of coronavirus disease 2019 (COVID-19): A systematic review and meta-analysis | PLOS ONE
2. Sarraf D, Rahimy E, Fawzi AA, Sohn E, Barbazetto I, Zacks DN, et al. Paracentral acute middle maculopathy: a new variant of acute macular neuroretinopathy associated with retinal capillary ischemia. JAMA Ophthalmol. 2013;131(10):1275-87. Comment in: Eye (Lond). 2016;30(5):643-4.
3. Azar G, Bonnin S, Vasseur V, Faure C, Salviat F, Clermont CV, et al. Did the COVID-19 pandemic increase the incidence of acute macular neuroretinopathy? J Clin Med [Internet]. 2021[cited 2022 Oct 15];10(21):5038. Available from: Did the COVID-19 Pandemic Increase the Incidence of Acute Macular Neuroretinopathy? - PMC (nih.gov)
4. Padhly SK, DCruz R, Kelgaonkar A. Paracentral acute middle maculopathy following SARS-CoV2 infection: the D-dimer hypothesis. BMJ Case Rep [Internet]. 2021 [cited 2023 Jan 30];14(3):e242043. Available from: Paracentral acute middle maculopathy following SARS-CoV-2 infection: the D-dimer hypothesis - PMC (nih.gov)
5. Ozsaygılı C, Bayram N, Ozdemir H. Cilioretinal artery occlusion with paracentral acute middle maculopathy associated with COVID-19. Indian J Ophthalmol [Internet]. 2021[cited 2022 Nov 21];69(7):1956-9. Comment in: Indian J Ophthalmol. 2021;69(10):2908. Available from: Cilioretinal artery occlusion with paracentral acute middle maculopathy associated with COVID-19 - PMC (nih.gov)
Submitted for publication:
April 3, 2023.
Accepted for publication:
May 3, 2023.
Funding: This study received no specific financial support.
Disclosure of potential conflicts of interest: None of the authors have any potential conflicts of interest to disclose.