

Christiana Rebello Hilgert1,2; Alvaro Haverroth Hilgert2; Alexandre Nakao Odashiro3,4; Patricia Rusa Pereira Odashiro1,5; Augusto Paranhos Jr.1
DOI: 10.5935/0004-2749.20180062
ABSTRACT
Purpose: To determine the effects of bevacizumab and mitomycin C alone and in combination on intraocular pressure and the scarring process after modified glaucoma filtration surgery in rabbits.
Methods: The rabbits underwent modified glaucoma filtration surgery and were allocated into three groups to receive intraoperative treatment with subconjunctival bevacizumab (group A), mitomycin C and subconjunctival bevacizumab (group B), or mitomycin C (group C). Intraocular pressure was measured immediately preoperatively and on postoperative days 8, 14, 17, 21, 26, and 30. The scarring process was assessed 30 days after surgery by tissue section using hematoxylin and eosin, Masson’s trichrome, and picrosirius. Expression of vascular endothelial growth factor (VEGF) was assessed by immunohistochemical analyses. All analyses were performed by a masked observer.
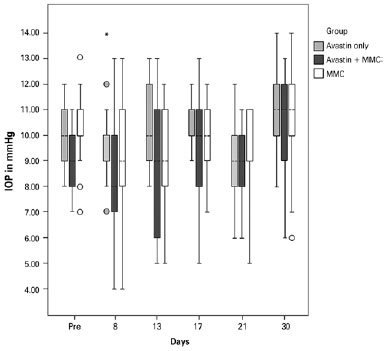
Results: Animals in group A had higher intraocular pressure than those in groups B and C (p<0.01). Intraocular pressure did not differ significantly between groups B and C. The amount of fibrosis was similar with all stains used: group A had the highest level of fibrosis compared with groups B and C (p>0.05). There was less VEGF expression in group A than in groups B and C (p<0.01). Groups B and C did not differ in VEGF expression.
Conclusion: Mean intraocular pressure and fibrosis were lower in animals receiving bevacizumab in combination with mitomycin C but did not differ from values in animals receiving mitomycin C alone. Inhibition of VEGF was greater when bevacizumab was used alone than when bevacizumab was combined with mitomycin C.
Keywords: Bevacizumab; IOP; Glaucoma/surgery; Filtering surgery; Intraoperative period; Wound healing; Rabbits
RESUMO
Objetivo: Determinar os efeitos do bevacizumab, combinados ou não à mitomicina C (MMC), na pressão intraocular e processo cicatricial pós-cirurgia filtrante anti-glaucomatosa modificada em coelhos.
Métodos: Os coelhos foram submetidos à cirurgia filtrante anti-glaucomatosa modificada e alocados em três grupos de acordo com o tratamento instituído - Grupo A: bevacizumab subconjuntival; Grupo B: bevacizumab subconjuntival e à mitomicina C ; Grupo C: à mitomicina C. A pressão intraocular foi aferida no período pré-operatório imediato e nos dias 8, 14, 17, 21, 26 e 30. O processo cicatricial foi avaliado no trigésimo dia de pós-operatório por meio de análise histopatológica utilizando-se hematoxilina eosina, tricrômio de Masson e picrosirius. A expressão do fator de crescimento do Endotélio Vascular (VEGF) foi avaliada por meio de análise imuno-histoquímica. Todas as análises foram feitas por um observador mascarado.
Resultados: O Grupo A apresentou maior pressão intraocular que os grupos B e C (p<0.01). Não foram encontradas alterações significativas entre os grupos B e C. A quantidade de fibrose encontrada nos grupos foi similar com os 3 corantes utilizados: o Grupo A apresentou maior nível de fibrose em relação aos grupos B e C (p>0,05). Houve menor expressão de Fator de Crescimento do Endotélio Vascular no Grupo A em relação aos grupos B e C (p<0,01). Não houve diferença estatisticamente significante na expressão de Fator de Crescimento do Endotélio Vascular entre os grupos B e C.
Conclusão: O bevacizumab associado à MMC apresentou pressões intraoculares mais baixas e menos fibrose, mas estes não foram estatisticamente significantes quando comparados ao uso da mitomicina C isolada. Uma maior inibição do fator de crescimento do endotélio vascular foi encontrada quando o bevacizumab foi usado isoladamente, em detrimento do seu uso associado à mitomicina C.
Descritores: Bevacizumab; Mitomicina; Glaucoma/cirurgia; Cirurgia filtrante; Período intraoperatório; Cicatrização; Coelhos
INTRODUCTION
Trabeculectomy is considered the gold standard surgical technique to enhance aqueous humor outflow through a filtering bleb, thus lowering intraocular pressure (IOP) in glaucoma. However, its success depends on wound healing modulation, which can be variable among patients. If postoperative conjunctival scarring is excessive, the created fistula tends to close and IOP rises again, leading to surgery failure(1).
Many factors favor excessive conjunctival fibrosis and surgery failure. Among others, subclinical inflammation of the ocular surface due to topical hypotensive medication routinely used by patients with glaucoma has been related to an increased number of conjunctival inflammatory cells, mediators, and fibroblasts at the surgery site in trabeculectomy(2).
Excessive fibrosis is responsible for surgery failure in most cases(3,4). Antimetabolites such as 5-fluorouracil (5-FU) and mitomycin C (MMC) are widely used in glaucoma surgery to avoid excessive scarring and are associated with postoperative complications, such as transient hypotony or even sight-threatening conditions such as endophthalmitis(5-8).
In spite of these complications, MMC is still considered the gold standard as adjunctive therapy in glaucoma filtration surgery (GFS), in part due to its ease of application and powerful antiproliferative effect and its superiority over 5-FU in achieving long-term lowering of IOP(9,10).
The need for safer trabeculectomy has led to some modifications of the initial technique and even the use of shunts as a primary surgical option to manage glaucoma(11-13). However, whenever a filtering bleb is created, the major challenge to the ophthalmologist remains wound healing modulation to avoid excessive scarring and surgery failure or insufficient scarring and related complications. This emphasizes the need for newer agents with a safer profile and proven efficacy in comparison with our current gold standard technique. Therefore, anti-vascular endothelial growth factor (VEGF) agents, such as bevacizumab, have been investigated in recent years(14-22). Nevertheless, more details about the best route of administration, doses, and the optimal time point in the healing process for the agent to be used are still warranted.
VEGF is a mitogen specific to vascular endothelial cells and is involved in the signal cascade that leads to fibroblast migration. Its effects can be suppressed by bevacizumab, a full-length humanized monoclonal antibody directed against all isoforms of VEGF A, which has been approved by the Food and Drug Administration for the treatment of metastatic colorectal and breast cancer(23). It inhibits angiogenesis, an important part of the wound-healing process that is responsible for the supply of inflammatory cells, mitogenic cytokines such as fibroblast growth factor, oxygen, and nutrients that support the proliferative phase of wound healing. Previous studies have demonstrated that VEGF is increased in the aqueous humor of patients with non-neovascular glaucoma(18,24,25). It has also been reported that high VEGF levels in Tenon tissue are linked to poor surgical outcomes in patients with glaucoma(25). VEGF expression in fibroblasts and inflammatory cells tends to increase after surgical insult. It is involved in angiogenesis, inflammation, and fibrosis, and its suppression could possibly inhibit the excessive scarring that may occur after trabeculectomy(4,26).
The inhibition Inhibition of VEGF by bevacizumab could possibly enhance trabeculectomy outcomes, with a safer profile than MMC, as well as act as an adjunctive to this drug in the scarring process in GFS.
The aim of this study was to determine the effects of bevacizumab and MMC alone and in combination on IOP and the scarring process after modified GFS in rabbits.
METHODS
This was a randomized, prospective, masked-observer study. Thirty New Zealand female rabbits, aged 12 to 14 weeks and weighing 2 to 3 kg, were acclimatized for 7 days and underwent modified GFS, an established, previously described model of glaucoma surgery that consists in making a scleral tract using a 22-gauge intravenous cannula (Insyte®; Becton Dickinson Ind. Cirurg., Juiz de Fora, MG, Brazil) until it reaches the anterior chamber, extending beyond the pupillary margin to avoid pupillary blockage of the tube. At this point, the cannula needle is removed, and the cannula is trimmed and beveled at its scleral end so that it protrudes 1 mm from the insertion point(27). It is then fixed by a 10-0 nylon suture (Ethicon®; Johnson & Johnson, SP, Brazil). The experiment was performed in accordance with the ARVO Statement for the Use of Animals in Ophthalmic and Vision Research. Approval was granted by the institutional Research Ethics Committee in Animal Research.
Treatment regimen
GFS was performed by a single surgeon on the right eye only. The surgeries were performed with the animals under general anesthesia by intramuscular injection of ketamine 50 mg/mL and xylazine 2%. The animals were randomly allocated into three groups according to the medications used during the surgery:
• Group A: Bevacizumab (Avastin®, Genentech, San Francisco, CA, USA). Subconjunctival injection using a 27-gauge needle (1.25-0.05 mL), adjacent to the site of the surgery at the end of the procedure.
• Group B: MMC (Mitocin®, Bristol-Myers Squibb, São Paulo, SP, Brazil) (0.2 mg/mL) soaked in a semilunar 8-mm diameter sponge (25.12 mm2 area), placed between the Tenon capsule and sclera for 3 min, followed by continuous irrigation with 20 mL of balanced salt solution and subconjunctival injection of bevacizumab as described above.
• Group C: MMC application alone, as previously described.
Postoperative regimen
Combined ciprofloxacin and dexamethasone ointment was instilled at the end of surgery and three times a day during the next 5 days of follow-up.
IOP measurements
Baseline IOP measurements were performed using Tonopen Avia (Reichert NY, USA) in the immediate preoperative period and on postoperative days 8, 14, 17, 22, 27, and 30 under the same general anesthesia regimen. Ten readings were taken and averaged. All measurements were taken by a masked observer.
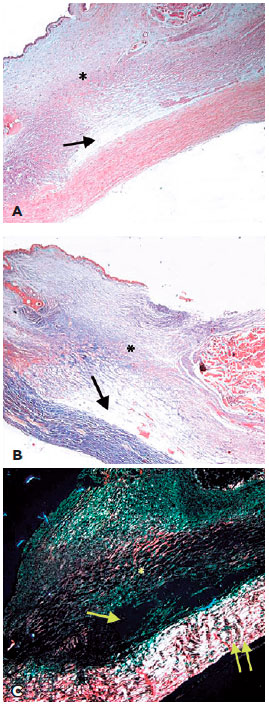
Scarring assessment of scarring process
The rabbits were sacrificed 30 days after surgery by a lethal intravenous injection of pentobarbital. The eyes were enucleated, and the bleb area was cut under microscopic guidance by the surgeon. The specimens were fixed in 10% formaldehyde and embedded in paraffin before5-mm sections were cut. Scarring was assessed by hematoxylin and eosin, Masson’s trichrome, and picrosirius staining of the bleb area, quantifying collagen deposition and fibrosis. The evaluation was masked and performed by an ocular pathologist, who determined the amount of collagen found in the sample as follows:
• Score 0: minimal or no fibrosis.
• Score 1: mild fibrosis.
• Score 2: moderate fibrosis.
• Score 3: severe fibrosis.
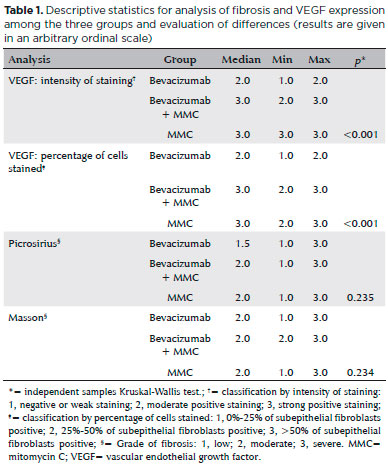
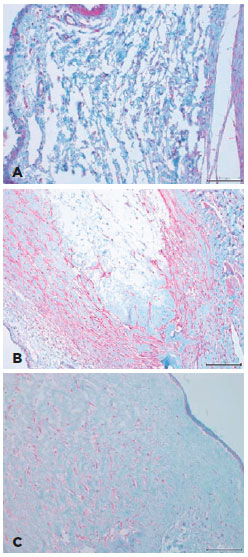
Immunohistochemistry
VEGF expression was determined by semiquantitative immunohistochemistry according to the percentage of positive-staining subepithelial fibroblasts and the intensity of staining based on the Quick Score Method(28). The evaluation was performed by a masked ocular pathologist.
The percentage of positive-staining cells was scored as follows:
• Score 1 (0%-25% of cells stained per section).
• Score 2 (25%-50% of cells stained per section).
• Score 3 (>50% of cells stained per section).
The intensity of staining was scored from 1 to 3 (weak, moderate, or intense staining).
Statistical analysis
The IOP data were analyzed using analysis of variance (ANOVA) for repeated measures. Data on scarring and VEGF expression were analyzed by the Kruskal-Wallis ANOVA test.
RESULTS
There was a statistically significant difference in IOP among the groups in the immediate preoperative period and on postoperative days 8, 14, 17, 22, 27, and 30. The bevacizumab-alone group had a higher IOP level than did the MMC-alone group and the bevacizumab plus MMC group (p<0.01). The bevacizumab plus MMC group had a lower IOP than did the MMC-alone group, but the difference was not statistically significant (p>0.05, ANOVA for repeated measures) (Figure 1). With regard to the scarring process, the amount of fibrosis in the samples was similar for the three stains used (hematoxylin and eosin, Masson’s trichrome, and picrosirius) (Figure 2). Group A had a higher level of fibrosis than did groups B and C (p<0.05, Kruskal-Wallis ANOVA). Group B had more fibrosis than did group C, but the difference was not statistically significant. There was less VEGF expression in group A, as shown by the percentage of cells stained and the intensity of staining, compared with that in groups B and C (p<0.0001, Kruskal-Wallis ANOVA). There was no difference in VEGF expression between groups B and C (Table 1). Examples of the immunohistochemical analyses are shown in figure 3.
DISCUSSION
Suppression of VEGF by bevacizumab has been under investigation for wound healing modulation in experimental GFS(17-19), However, the best dosage and route of administration of bevacizumab are still to be determined. We chose a single subconjunctival injection because there have been reports of increased bioavailability of bevacizumab with the use of this route(29,30). The drug can be delivered by the transscleral route into intraocular tissues or clearance via conjunctival and lymphatic flow(30). After a single subconjunctival injection, the bevacizumab level was maintained above IC50 (half-maximum inhibitory concentration of bevacizumab) for 8.6 weeks in the retina/choroid and 8.4 weeks in the iris/ciliary body(29). Nomoto et al. showed that the half-life of bevacizumab was longer after subconjunctival injection than after intravitreal injection. This might be explained by a scleral binding mechanism that could respond for sustained release of the drug(29). Other reasons that we chose one single subconjunctival injection at the time of surgery as the route of administration were that it is less invasive than intravitreal injections and the drug would be directly applied to the target site, the subconjunctival space and the surrounding area that suffered the surgical insult. Nevertheless, when this route is used, bevacizumab is likely to have a faster clearance. The conjunctival blood vessels do not have a tight junction barrier, so that bevacizumab can enter the blood circulation by pinocytosis and/or convective transport through paracellular pores in the vascular endothelial layer, as previously noted(29). Clearance can be minimized by a possible scleral depot binding of the drug and the relatively high permeability of the sclera to IgG antibodies(30). Li et al., on the contrary, suggested that VEGF can be partially suppressed for up to 6 days by a single subconjunctival injection of bevacizumab(18).
We found a statistically significant difference in IOP among the three groups during follow-up. IOP was higher when bevacizumab was used alone than when MMC was used alone or in combination with bevacizumab; this difference was possibly related to the higher level of fibrosis in the bevacizumab-alone group. These findings agree with those of Li and coworkers, who also reported no improvement in IOP at any time point after experimental GFS with the use of bevacizumab, in spite of significant inhibition of angiogenesis and fibrosis, as well as improvement in the bleb area(18).
Studies in humans conducted after our study, using a similar approach, showed that, as well as being safe and effective in controlling IOP, bevacizumab subconjunctival injection showed less prominent effect than did MMC(20,21).
On the other hand, Sengupta et al., in a pilot study in humans, performed three sequential bevacizumab subconjunctival injections at distinct time points during and after single- phacotrabeculectomy (immediately preoperatively and postoperatively and on postoperative day 7). The short-term outcomes suggest that sequential subconjunctival injections are equally effective in reducing IOP as MMC(22).
We found a higher level of fibrosis when intraoperative bevacizumab was used alone, compared with its combined use with MMC and even MMC alone. Although previous studies have shown the potent antifibrotic activity of bevacizumab when used alone and combined with 5-FU in the same type of experimental GFS, bevacizumab was administered at the end of surgery and weekly for 3 weeks, or even for 7 weeks, and its action was not compared with that of the most potent antiproliferative drug used in trabeculectomy, i.e., MMC(17-19). Such aggressive and costly treatment has to be considered to obtain higher levels of VEGF inhibition(19).
An additional antiscarring effect of bevacizumab used in combination with MMC was not observed in our study, in agreement with the results of Kiddee et al. in a recent prospective placebo trial, in which a single subconjunctival injection of bevacizumab did not appear to have an additive benefit on outcomes of trabeculectomy with the use of MMC in humans(31).
Paula et al. showed that even small amounts of bevacizumab could lower the proportion of VEGF-expressing fibroblasts in a rabbit model(32). We also were able to demonstrate by immunohistochemical analyses that VEGF expression was lower in the bevacizumab-alone group, as evident from both the percentage of cells stained and the intensity of staining. Interestingly, however, there was no statistically significant difference in VEGF expression between the groups receiving MMC alone and in combination with bevacizumab. VEGF suppression in the bevacizumab plus MMC group was not evident, suggesting a possible interaction between these drugs when used concomitantly at the same site, as well as a lack of benefit from using intraoperative subconjunctival bevacizumab as an adjunct drug with MMC in trabeculectomy.
Bevacizumab alone was not as effective at modulation of the scarring process after trabeculectomy as was bevacizumab combined with MMC or even MMC alone. Use of the two drugs combined was associated with lower mean IOP and less fibrosis, but these effects did not significantly differ from those with the use of MMC alone. Higher inhibition of VEGF was found when bevacizumab was used alone, but such anti-VEGF action was not evident when bevacizumab was combined with MMC. This result is in accordance with previous studies in humans that could not demonstrate an additional beneficial effect of bevacizumab when it was combined with MMC in trabeculectomy, and even in postoperative needling, and reoperations(31,33,34).
REFERENCES
1. Lama PJ, Fechtner RD. Antifibrotics and wound healing in glaucoma surgery. Surv Ophthalmol. 48(3):314-46.
2. Broadway DC, Grierson I, Stürmer J, Hitchings RA. Reversal of topical antiglaucoma medication effects on the conjunctiva. Arch Ophthalmol (Chicago, Ill 1960). 1996;114(3):262-7.
3. Addicks EM, Quigley HA, Green WR, Robin AL. Histologic characteristics of filtering blebs in glaucomatous eyes. Arch Ophthalmol. 1983;101(5):795-8.
4. Yamanaka O, Kitano-Izutani A, Tomoyose K, Reinach PS. Pathobiology of wound healing after glaucoma filtration surgery. BMC Ophthalmol. 2015;15 Suppl 1:157.
5. Heuer DK, Parrish RK, Gressel MG, Hodapp E, Palmberg PF, Anderson DR. 5-fluorouracil and glaucoma filtering surgery. II. A pilot study. Ophthalmology. 1984;91(4):384-94.
6. Fluorouracil Filtering Surgery Study one-year follow-up. The Fluorouracil Filtering Surgery Study Group. Am J Ophthalmol. 1989; 108(6):625-35.
7. Suñer IJ, Greenfield DS, Miller MP, Nicolela MT, Palmberg PF. Hypotony maculopathy after filtering surgery with mitomycin C. Incidence and treatment. Ophthalmology. 1997;104(2):207-14; discussion 214-5.
8. Greenfield DS, Suñer IJ, Miller MP, Kangas TA, Palmberg PF, Flynn HW. Endophthalmitis after filtering surgery with mitomycin. Arch Ophthalmol. 1996;114(8):943-9.
9. Desai MA, Gedde SJ, Feuer WJ, Shi W, Chen PP, Parrish RK 2nd. Practice preferences for glaucoma surgery: a survey of the American Glaucoma Society in 2008. Ophthalmic Surg Lasers Imaging. 2011;42(3):202-8.
10. De Fendi LI, Arruda G V, Scott IU, Paula JS. Mitomycin C versus 5-fluorouracil as an adjunctive treatment for trabeculectomy: a meta-analysis of randomized clinical trials. Clin Exp Ophthalmol. 2013;41(8):798-806.
11. Dhingra S, Khaw PT. The Moorfields safer surgery system. Middle East Afr J Ophthalmol. 2009;16(3):112-5.
12. Maris PJ Jr., Ishida K, Netland PA. Comparison of trabeculectomy with Ex-PRESS miniature glaucoma device implanted under scleral flap. J Glaucoma. 2007;16(1):14-9.
13. Khaw PT, Chiang M, Shah P, Sii F, Lockwood A, Khalili A. Enhanced trabeculectomy: the Moorfields Safer Surgery System. Dev Ophthalmol. 2012;50:1-28.
14. Mathew R, Barton K. Anti--vascular endothelial growth factor therapy in glaucoma filtration surgery. Am J Ophthalmol. 2011;152(1): 10-5.e2.
15. Grewal DS, Jain R, Kumar H, Grewal SP. Evaluation of subconjunctival bevacizumab as an adjunct to trabeculectomy. a pilot study. Ophthalmology. 2008;115(12):2141-5.e2.
16. Takihara Y, Inatani M, Kawaji T, Fukushima M, Iwao K, Iwao M, et al. Combined intravitreal bevacizumab and trabeculectomy with mitomycin C versus trabeculectomy with mitomycin C alone for neovascular glaucoma. J Glaucoma. 2011;20(3):196-201.
17. How A, Chua JL, Charlton A, Su R, Lim M, Kumar RS, et al. Combined treatment with bevacizumab and 5-Fluorouracil attenuates the postoperative scarring response after experimental glaucoma filtration surgery. Investig Ophthalmol Vis Sci. 2010;51(2):928-32.
18. Li Z, Van Bergen T, Van de Veire S, Van de Vel I, Moreau H, Dewerchin M,et al. Inhibition of vascular endothelial growth factor reduces scar formation after glaucoma filtration surgery. Investig Ophthalmol Vis Sci. 2009;50(11):5217-25.
19. Memarzadeh F, Varma R, Lin LT, Parikh JG, Dustin L, Alcaraz A, et al. Postoperative use of bevacizumab as an antifibrotic agent in glaucoma filtration surgery in the rabbit. Investig Ophthalmol Vis Sci. 2009;50(7):3233-7.
20. Akkan JU, Cilsim S. Role of subconjunctival bevacizumab as an adjuvant to primary trabeculectomy: a prospective randomized comparative 1-year follow-up study. J Glaucoma. 2015;24(1):1-8.
21. Nilforushan N, Yadgari M, Kish SK, Nassiri N. Subconjunctival bevacizumab versus mitomycin C adjunctive to trabeculectomy. Am J Ophthalmol. 2012;153(2):352-7.e1.
22. Sengupta S, Venkatesh R, Ravindran RD. Safety and efficacy of using off-label bevacizumab versus mitomycin C to prevent bleb failure in a single-site phacotrabeculectomy by a randomized controlled clinical trial. J Glaucoma. 2012;21(7):450-9.
23. Hurwitz H, Saini S. Bevacizumab in the treatment of metastatic colorectal cancer: safety profile and management of adverse events. Semin Oncol. 2006;33(5 Suppl 10):S26-S34.
24. Hu DN, Ritch R, Liebmann J, Liu Y, Cheng B, Hu MS. Vascular endothelial growth factor is increased in aqueous humor of glaucomatous eyes. J Glaucoma. 2002;11(5):406-10.
25. Lopilly Park HY, Kim JH, Ahn MD, Park CK. Level of vascular endothelial growth factor in tenon tissue and results of glaucoma surgery. Arch Ophthalmol. 2012;130(6):685-9.
26. Wilgus TA, Ferreira AM, Oberyszyn TM, Bergdall VK, Dipietro LA. Regulation of scar formation by vascular endothelial growth factor. Lab Invest. 2008;88(6):579-90.
27. Esson DW, Neelakantan A, Iyer SA. Expression of connective tissue growth factor after glaucoma filtration surgery in a rabbit model. Invest Ophthalmol Vis Sci. 2004;45(2):485-91.
28. Faingold D, Marshall J-C, Antecka E, Di Cesare S, Odashiro AN, Bakalian S, et al. Immune expression and inhibition of heat shock protein 90 in uveal melanoma. Clin Cancer Res. 2008;14(3):847-55.
29. Nomoto H, Shiraga F, Kuno N, Kimura E, Fujii S, Shinomiya K, et al. Pharmacokinetics of bevacizumab after topical, subconjunctival, and intravitreal administration in rabbits. Investig Ophthalmol Vis Sci. 2009;50(10):4807-13.
30. Ambati J, Gragoudas ES, Miller JW, You TT, Miyamoto K, Delori FC, et al. Transscleral delivery of bioactive protein to the choroid and retina. Invest Ophthalmol Vis Sci. 2000;41(5):1186-91.
31. Kiddee W, Orapiriyakul L, Kittigoonpaisan K, Tantisarasart T, Wangsupadilok B. Efficacy of adjunctive subconjunctival bevacizumab on the outcomes of primary trabeculectomy with mitomycin C: a prospective randomized placebo-controlled trial. J Glaucoma 2015; 24(8):600-6.
32. Paula JS, Ribeiro VR, Chahud F, Cannellini R, Monteiro TC, Gomes EC, et al. Bevacizumab-loaded polyurethane subconjunctival implants: effects on experimental glaucoma filtration surgery. J Ocul Pharmacol Ther. 2013;29(6):566-73.
33. Tai TY, Moster MR, Pro MJ, Myers JS, Katz LJ. Needle bleb revision with bevacizumab and mitomycin c compared with mitomycin C alone for failing filtration blebs. J Glaucoma. 2015;24(4):311-5.
34. Saeed AM, AboulNasr TT. Subconjunctival bevacizumab to augment trabeculectomy with mitomycin C in the management of failed glaucoma surgery. Clin Ophthalmol. 2014;8:1745-55.
Submitted for publication:
August 24, 2017.
Accepted for publication:
February 5, 2018.
Approved by the following research ethics committee: Universidade Federal de São Paulo (# 1227/09)
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose