

Rafaella Nascimento e Silva1,2; Lycia Maria Martins Pinho Pedral Sampaio1; Aline Silveira Moriyama1,3; Nicolas Cesário Pereira1,3; Mark Lane4; Hudson Vergennes da Silva1; Adriana dos Santos Forseto1,5
DOI: 10.5935/0004-2749.20180021
ABSTRACT
Purpose: Donated corneas are classified as tectonic if there are defects within any layers of the cornea which would prevent a satisfactory visual outcome after transplantation. This study aimed to evaluate whether some tectonic corneas have sufficient endothelial characteristics to allow their use in posterior lamellar keratoplasty, and explored their reclassification for use in this sight-improving procedure.
Methods: A retrospective review of all corneal tissues preserved by the Sorocaba Eye Bank from January to April of 2014 was performed. All donated corneas classified as tectonic were included. Endothelial tissue was defined as healthy and viable for posterior lamellar keratoplasty if endothelial cell density was ≥2000 cells/mm2. Additional parameters analyzed included Descemet folds and stretch marks, loss of endothelial cells, corneal endothelial polymegathism/ pleomorphism, pseudo-guttata, and reflectivity.
Results: During the study period, 2,847 corneas were preserved, of which 423 (14.85%) were classified as tectonic. Of these, 87 (20.56%) were reported as having endothelial viability and were included in the posterior lamellar keratoplasty group. Average corneal endothelial cell density of this group was 2,471 SD ± 256 cells/mm2 (range 2012-2967 cells/mm2).
Conclusion: A significant number of corneas classified as tectonic showed endothelial viability and were included in the posterior lamellar keratoplasty group (20.56%). Despite stromal and/or epithelial alterations, these corneas could have been potentially distributed for posterior lamellar transplantation to improve vision, thus reducing the corneal transplantation waiting period. This study highlights how corneal tissue reclassification could increase the potential amount of corneal tissue available for optical transplantation.
Keywords: Corneal transplantation; Eye banks; Tissue donors; Cornea; Tissue and organ procurement
RESUMO
Objetivo: Avaliar a vitalidade endotelial das córneas classificadas como tectônicas e discutir a viabilidade de seu uso na ceratoplastia lamelar posterior.
Métodos: Realizou-se uma revisão retrospectiva de todos os tecidos corneanos preservados pelo Banco de Olhos Sorocaba de janeiro a abril de 2014. Todas as córneas doadas classificadas como tectônicas foram incluídas e avaliadas com ênfase na vitalidade endotelial. Os parâmetros de avaliação da lâmpada de fenda de cada córnea e densidade de células endoteliais medidos por microscópio especular foram registrados: córneas que apresentavam vitalidade endotelial apesar de alterações no estroma e/ou no epitélio foram selecionadas e incluídas em um grupo denominado grupo lamelar posterior. O tecido endotelial foi definido como saudável e viável para a ceratoplastia lamelar posterior, se houvesse uma densidade de células endoteliais ≥2.000 células/mm2. Outros parâmetros também foram analisados, incluindo; estrias ou pregas na Descemet, perda de células endoteliais, polimegatismo e pleomorfismo endotelial, pseudo-guttata e reflexividade endotelial.
Resultados: Durante o período do estudo, foram preservadas 2.847 córneas, das quais 423 (14,85%) foram classificadas como tectônicas. Dessas, 87 (20,56%) apresentaram vitalidade endotelial e foram incluídos no grupo lamelar posterior. A densidade média das células endoteliais da córnea deste grupo era de 2.471 SD ± 256 células/mm2, variando de 2.012 a 2.967 células/mm2.
Conclusão: Um número significativo de córneas classificadas como tectônicas apresentaram vitalidade endotelial e foram incluídas no grupo lamelar posterior (20,56%). Apesar de alterações estromais e/ou epiteliais, estas córneas poderiam ter sido potencialmente distribuídas para transplantes lamelares posteriores com finalidade ótica, otimizando a disponibilidade de tecidos, com impacto positivo na saúde pública.
Descritores: Transplante de córnea; Bancos de olhos; Doadores de tecidos; Córnea; Obtenção de tecidos e órgãos
INTRODUCTION
Corneal transplantation is reported to be the most frequent type of transplant performed around the world(1,2). In Brazil alone, there has been a reported increase in corneal transplants from 3,626 procedures in 2000 to 14,534 cases in 2016(3,4). Indications for corneal transplantation can be classified into four domains; optical (to restore sight), tectonic/reconstructive (to restore anatomy of the globe), therapeutic (to remove corneal tissue which is infected or inflamed and unresponsive to treatment), and cosmetic (to improve aesthetics of the eye, particularly in patients with corneal scars)(5). Optical keratoplasties are the most prevalent, followed by tectonic and therapeutic(6).
In Brazil, donated corneas are often classified as optical or tectonic. They are defined as optical if all the corneal layers are viable and if they can be used to perform penetrating corneal transplantation to improve visual acuity. Donated corneas are defined as tectonic if there are defects within any corneal layers which would prevent a satisfactory visual outcome(5,7).
There are a number of techniques which can be utilized in corneal transplantation including penetrating keratoplasty (where all layers of the cornea are replaced), and lamellar keratoplasty (where specific layers are transplanted; further sub-divided into anterior and posterior procedures). In anterior lamellar keratoplasties, only anterior layers of the cornea are replaced; this technique is therefore utilized to treat conditions where the posterior layers remain intact. Conversely, in posterior lamellar keratoplasties (PLK), only posterior layers are replaced. This technique is particularly useful in the treatment of corneal endothelial pathologies(8-10).
Penetrating keratoplasty was historically the commonest procedure performed for the treatment of general corneal pathologies. However, as lamellar keratoplasty is associated with a lower risk of rejection, much research has been undertaken to help improve this technique(9-16).
A number of posterior lamellar techniques have been developed including Descemet stripping automated keratoplasty (DSEK), Descemet stripping automated endothelial keratoplasty (DSAEK), and Descemet membrane endothelial keratoplasty (DMEK). These procedures have been designed to reduce risk of rejection and improve final visual outcomes(9,17,18). Since 2012, PLK has become the predominant type of corneal transplant performed in the United States(19).
PLK replaces dysfunctional endothelium with a functional donor graft. Anterior layers of the donated cornea are not used in surgery and therefore the condition of the anterior cornea does not impact the ability to perform PLK. The procedure requires only a healthy and functioning endothelial layer. Grafts with anterior defects such as stromal scars were traditionally used for tectonic/ reconstructive purposes only, even if they had a viable endothelium. With the advent of PLK, it is now possible to use these grafts in optical procedures and not solely for tectonic purposes.
In Brazil, eye banks are responsible for selection, collection, evaluation, and preservation of donor tissue and are required to send audit information to the State Transplantation Center(20). The National Transplantation System is exclusively managed by the government and is responsible for distribution of all available corneal grafts.
The Sao Paulo State Health Bureau/State Transplantation Center and the local Cornea and Eye Banks Technical Committee have made efforts to propose a new classification system for donated corneas to optimize resources. A recent technical note published in Sao Paulo announced the inclusion of two new categories for donated corneas: anterior lamellar and posterior lamellar. It is hoped that this new classification can be adopted at the national level and that this will help increase the number of corneas available for optical transplantation.
The purpose of this study was to evaluate endothelial characteristics of corneas classified as tectonic, and to explore feasibility of their use in PLK.
METHODS
A review of all corneal tissue preserved by the Sorocaba Eye Bank from January 2014 to April 2014 was performed. The review classified the tissue as optical, tectonic, or discarded. In the Sorocaba Eye Bank (BOS -Banco de Olhos de Sorocaba), after tissue preservation, each corneal parameter is classified using slip lamp evaluation from 0 to 4 (0, excellent; 1, good; 2, average; 3, tectonic use only; 4, unacceptable). Donor tissues classified as 3 in one or more domains are mainly reserved for use in emergency or tectonic procedures(8,15).
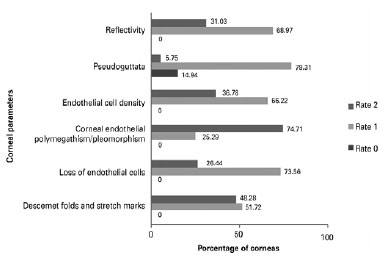
Within the tectonic group, endothelial tissue was defined as healthy and viable for PLK if it had cell density ≥2,000 cells/mm2. Grafts were classified as 0 (excellent) when cell count was ≥3,000 cells/mm2; 1 (good) when it ranged from 2,999 to 2,500 cells/mm2; and 2 (average) from 2,000 to 2,499 cells/mm2. Additional endothelial parameters including Descemet folds and stretch marks, loss of endothelial cells, corneal endothelial polymegathism/pleomorphism, pseudo-guttata, and reflectivity were also graded using the same rating system.
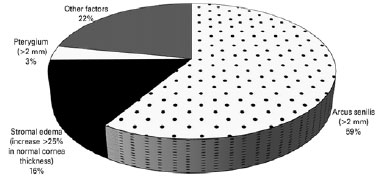
Tectonic corneas graded 0, 1, or 2 in endothelial parameters were considered viable for PLK, even if they were graded 3 in one or more epithelial or stromal parameters. Epithelial and stromal characteristics that resulted in a score of 3 included: >50% of corneal epithelial exposure, presence of an epithelial defect >4 mm in size, central epithelial or sub-epithelial opacity, arcus senilis >2 mm in size, pterygium >2 mm in size, and marked stromal edema increasing corneal thickness by >25%.
Data analysis (quantitative and qualitative analyses) was carried out using Microsoft Excel 2010, Microsoft Corporation, Seattle, WA, United States.
RESULTS
During the 4-month study period, the Sorocaba Eye Bank preserved 2,847 corneas. Of these, 1,177 (41.34%) were classified as optical, 423 (14.85%) were classified as tectonic and 1,247 (43.80%) were discarded.
In the 423 classified as tectonic, main reasons for not being utilized for optical transplantation included the presence of Descemet's folds or Descemet's striae (n=221 or 52.24%), arcus senilis (n=93 or 21.98%), and endothelial pleomorphism (n=95 or 22.45%). Over half (62%) of the tectonic corneas were eventually discarded as they reached their expiration date before use, and 87 (20.56%) of those evaluated would have had adequate endothelial cell count and sufficient scores in all endothelial parameters to permit their use in PLK.
The average corneal endothelial cell density within this subset was 2,471 SD ± 256 cells/mm2 (range 2,0122,967 cells/mm2). Of these 87 corneas, 15 had excellent or good ratings in all endothelial parameters. Figure 1 shows the percentage of corneas graded as excellent, good, or average in each of the six domains. Figure 2 indicates why these donated corneas were originally classified as tectonic grafts despite a viable endothelium. These causes included arcus senilis (59%), stromal edema (16%), and pterygium (3%). Other epithelial and stromal factors described in the methods were responsible for 22% of the cases.
DISCUSSION
Blindness and visual impairment due to corneal pathology are a significant public health problem in the developing world(21,22). Corneal transplantation is a viable option for visual rehabilitation in those who are blind secondary to corneal diseases(22).
Corneal transplantation surgery has come a long way since Edward Zirm first performed a corneal graft. During the last century, there have been ongoing efforts to improve the technique and results of this surgery(23).
Recent emphasis has been on performing selective excision of diseased corneal tissue and its replacing it with healthy donor corneal grafts(2). These include deep anterior lamellar keratoplasty and endothelial keratoplasties (DSEK, DSAEK, and DMEK). These techniques have resulted in one donated cornea being used to treat two patients by separating anterior and posterior layers from a single graft(8). Unfortunately, in Brazil, the legislative structure is not yet in place to allow eye banks to offer pre-cut anterior and posterior corneal grafts.
Brazil has one of the largest public corneal transplant systems in the world(24). This service comprises harvesting and processing of donated corneas by eye banks. Additionally, patients never pay for a cornea. In Brazil, this service is funded and regulated by the public health system known as the Sistema Único de Saúde (SUS). If patients choose to have this surgery performed outside the SUS accredited network, it is possible for them to fund it personally or through private health insurance(25).
In December 2016, the number of patients in Brazil awaiting a corneal transplant was 10,923. In the same period, there were 3,427 patients awaiting corneal transplantation in the state of Sao Paulo alone, with an estimated waiting time of nine months(3). It is of paramount importance that corneal tissues are correctly graded and utilized effectively to help reduce this burden.
PLK is overtaking penetrating keratoplasty as the predominant surgical technique for endothelial replacement in Brazil. In 2014, the Sorocaba Ophthalmologic Hospital/Sorocaba Eye Bank (BOS) performed 321 PLKs, accounting for 18.94% of all corneal transplants performed (n=1,694). As a philanthropic institution, most surgeries at this hospital are performed under the public health system (SUS), and corneal transplants at this hospital serve patients from all states of Brazil.
PLK involves selective transplantation of the posterior cornea and therefore can utilize corneas with anterior pathology such as arcus senilis or scars from refractive surgery. In 2005, the medical advisory board of the Eye Bank Association of America revised standard criteria allowing the use of tissue with good endothelial cells but with anterior pathology to be transplanted using PLK surgery(17).
In Brazil, data on quality of corneas processed and preserved in various eye banks is scarce. To optimize the use and distribution of corneas nationally, we have analyzed the endothelial cell count of corneas previously classified as tectonic to understand if these grafts could feasibly be used in PLK.
This study showed that a significantly large number of corneas classified as tectonic probably had a viable endothelium, which would have allowed their use in PLK (20.56%). Such corneas could have been potentially used in endothelial transplantation for optical purposes. They accounted for 3.05% (87/2,847) of the total number of corneas preserved by BOS during the study period.
Limitations of this study include its retrospective study design which did not allow for individual reassessment of corneas, and lack of comparative national and regional data.
In conclusion, this study highlights corneal graft reclassification as an approach to increase the potential number of grafts available for optical transplantation. The ability to use tectonic grafts for optical transplantation has the potential to revolutionize corneal transplantation in Brazil, reduce waiting lists, and offer the possibility of improved visual outcomes to thousands of patients.
REFERENCES
1. Gain P, Jullienne R, He Z, Aldossary M, Acquart S, Cognasse F, et al. Global survey of corneal transplantation and eye banking. JAMA Ophthalmol. 2016;134(2):167-73.
2. Saldanha BO, Oliveira RE Jr, Araujo PL, Pereira WA, Simao Filho C. Causes of nonuse of corneas donated in 2007 in Minas Gerais. Transplant Proc. 2009;41(3):802-3.
3. Dimensionamento dos Transplantes no Brasil e em cada estado. Associação Brasileira de Transplantes de Órgãos. 2009/2016.
4. Associação Brasileira de Transplantes de Órgãos. Registro Brasileiro de Transplantes. RBT Anual - Janeiro/Dezembro 2010 [Internet]. São Paulo: ABTO; 2010. [citado 2012 Jul 21]. Disponível em: http://www.abto.org.br/abtov03/Upload/file/RBT/2010/1.pdf
5. Tan DT, Janardhanan P, Zhou H, Chan YH, Htoon HM, Ang LP, et al. Penetrating keratoplasty in Asian eyes: the Singapore Corneal Transplant Study. Ophthalmology. 2008;115(6):975-82.e1.
6. Wagoner MD, Ba-Abbad R, Al-Mohaimeed M, Al-Swailem S, Zimmerman MB. Postoperative complications after primary adult optical penetrating keratoplasty: prevalence and impact on graft survival. Cornea. 2009;28(4):385-94.
7. Garralda A, Epelde A, Iturralde O, Compains E, Maison C, Altarriba M, et al. [Cornea transplant]. An Sist Sanit Navar. 2006;29 Suppl 2:163-73. Spanish.
8. Vajpayee RB, Sharma N, Jhanji V, Titiyal JS, Tandon R. One donor cornea for 3 recipients: a new concept for corneal transplantation surgery. Arch Ophthalmol (Chicago, Ill: 1960). 2007;125(4):552-4.
9. Tan DT, Dart JK, Holland EJ, Kinoshita S. Corneal transplantation. Lancet. 2012;379(9827):1749-61.
10. Terry MA. The evolution of lamellar grafting techniques over twenty-five years. Cornea. 2000;19(5):611-6.
11. Suh LH, Yoo SH, Deobhakta A, Donaldson KE, Alfonso EC, Culbertson WW, et al. Complications of Descemet's stripping with automated endothelial keratoplasty: survey of 118 eyes at One Institute. Ophthalmology. 2008;115(9):1517-24.
12. Lee JS, Desai NR, Schmidt GW, Jun AS, Schein OD, Stark WJ, et al. Secondary angle closure caused by air migrating behind the pupil in descemet stripping endothelial keratoplasty. Cornea. 2009;28(6): 652-6.
13. Shih CY, Ritterband DC, Rubino S, Palmiero PM, Jangi A, Liebmann J, et al. Visually significant and nonsignificant complications arising from Descemet stripping automated endothelial keratoplasty. Am J Ophthalmol. 2009;148(6):837-43.
14. Glasser DB. Tissue complications during endothelial keratoplasty. Cornea. 2010;29(12):1428-9.
15. Sharma N, Agarwal P, Titiyal JS, Kumar C, Sinha R, Vajpayee RB. Optimal use of donor corneal tissue: one cornea for two recipients. Cornea. 2011;30(10):1140-4.
16. Rose L, Briceno CA, Stark WJ, Gloria DG, Jun AS. Assessment of eye bank-prepared posterior lamellar corneal tissue for endothelial keratoplasty. Ophthalmology. 2008;115(2):279-86.
17. Eye Bank Association of America. Medical Standards. These standards have the apporval of the Eye Banking Committee of the American Academy of Ophthalmology [Internet]. Washington, DC: EBAA; 2005. [cited 2016 Jul 21].
18. Ang M, Wilkins MR, Mehta JS, Tan D. Descemet membrane endothelial keratoplasty. Br J Ophthalmol. 2016;100(1):15-21.
19. Eye Bank Association of America. Statistical Report [Internet]. Washington, DC: EBAA; 2015. [cited 2016 Jun 21]. Available from: http://restoresight.org/what-we-do/publications/statistical-report/
20. Brasil. Ministério da Saúde. Agência Nacional de Vigilância Sanitária. Resolução nº 67, de 30 de setembro de 2008. Dispõe sobre o Regulamento Técnico para o Funcionamento de bancos de tecidos oculares de origem humana [Internet]. Brasília, DF; MS; 2008. [citado 2016 Mar 19]. Disponível em: http://bvsms.saude.gov.br/bvs/saudelegis/anvisa/2008/res0067_30_09_2008.html
21. Smith GT, Taylor HR. Epidemiology of corneal blindness in developing countries. Refract Corneal Surg. 1991;7(6):436-9. Comment in: Refract Corneal Surg. 1991;7(6):417-8.
22. Oliva MS, Schottman T, Gulati M. Turning the tide of corneal blindness. Indian J Ophthalmol. 2012;60(5):423-7.
23. Moffatt SL, Cartwright VA, Stumpf TH. Centennial review of corneal transplantation. Clin Exp Ophthalmol. 2005;33(6):642-57. Comment in: Clin Exp Opthalmol. 2006;34(4):387-8.
24. Marinho A. [A study on organ transplantation waiting lines in Brazil's Unified National Health System]. Cad Saúde Pública. 2006; 22(10):2229-39. Portuguese.
25. Bonfadini G, Roisman V, Prinz R, Sarlo R, Rocha E, Campos M. Doação e fila de transplante de córnea no Estado do Rio de Janeiro. Rev Bras Oftalmol. 2014;73(4):237-42.
Submitted for publication:
May 17, 2017.
Accepted for publication:
September 24, 2017.
Funding: No specific financial support was available for this study. This study was supported by.
Disclosure of potential conflicts of interest: ML was supported by a joint award from the Birdshot Uveitis Society/Fight for Sight (24BU151). The others authors do not have any potential conflict of interest to disclose.
Approved by the following research ethics committee: Plataforma Brasil/ Comitê de ética em pesquisa do Hospital Oftalmológico de Sorocaba (CAAE 30275714.3.0000.0088.)