INTRODUCTION
Epiretinal membrane (ERM) is a type of nonvascular fibrocellular proliferation that develops on the surface of the internal limiting membrane and causes retinal wrinkling and distortion. Spectral domain optical coherence tomography (SD-OCT) has yielded unprecedented details about ERM, the retinal structure, the overlying vitreous layer, and has reliably resolved details of individual retinal layers(1-3). One layer that is clearly delineated by SD-OCT represents the junction between the photoreceptor's inner and outer segments (IS/OS junction). In normal eyes, this junction is visible as a hyperreflective line immediately above the retinal pigment epithelium. Disruption of this layer reflects an anatomical disruption of the retinal photoreceptors(4,5). Studies involving SD-OCT in patients with ERM have shown that visual acuity deteriorates as a result of IS/OS junction disruption(6-10), and that there is thickening of the central macula(8-12) and outer retina(11,12). In support of this, Oster et al.(13) found that the IS/OS junction was a more useful predictor of poor visual acuity when compared with central macular thickness.
Currently, both preoperative and postoperative IS/OS disruption are known to lead to visual acuity deterioration in eyes with ERM; however, very little information is currently available about the relationship between IS/OS disruption and the ERM grade. Furthermore, the ERM grade during which IS/OS disruption begins has yet to be discerned. In this study, we evaluated the relationships of IS/OS disruption, macular thickness, and ERM grade with visual acuity. Additionally, we evaluated the relationship between IS/OS disruption and ERM grade.
METHODS
Data of patients with different ERM grades who had undergone SD-OCT scanning (HRA-2; Heidelberg Engineering, Heidelberg, Germany) were retrospectively reviewed, in accordance with the tenets of the Declaration of Helsinki. Only patients with primary ERM were included in the study. We excluded patients with primary vitrectomy and ocular disorders associated with ERM, such as uveitis, and patients with macular disorders and/or significant cataracts that blocked the visualization of ERM during fundoscopy and SD-OCT scans. The final study group was comprised of a total of 54 eyes of 54 patients. We obtained each patient's age, sex, and best-corrected visual acuity (BCVA) from medical records.
All patients underwent SD-OCT evaluations involving horizontal and vertical scans performed at maximal resolution through the fovea. Patients also underwent fundus imaging via color fundus photography (Topcon, Paramus, NJ, USA) to visualize details of the fundus. For each patient, the ERM severity was graded on fundus images using a three-step scale as described previously(13). Grades 1, 2, and 3 ERM were defined as a visible membrane without retinal striae or vessel distortion, mild to moderate macular striae or vessel straightening, and moderate to severe striae and vascular straightening, respectively (Figure 1 A, B, and C, respectively). A single observer (S.K.) who was blinded to the visual acuity and SD-OCT scan data graded all fundus images.

Figure 1 Fundus grading of the epiretinal membrane (ERM). A) Example of a grade 1 ERM with minimal retinal surface changes. B) Early macular striae are visible in a grade 2 ERM. C) A combination of large macular striae and prominent vascular straightening are seen in a grade 3 ERM.
Next, we measured several variables from the SD-OCT images. Foveal thickness, which was calculated using a caliper feature on the SD-OCT instrument with manual correction as needed, was determined as an average of the values from both horizontal and vertical scans. The photoreceptor IS/OS layer was evaluated for 500 μm in either direction of the fovea on both horizontal and vertical scans, and a diagnosis of a disrupted IS/OS junction was based on the absence and/or irregularity of the aforementioned hyperreflective line (Figure 2 A, B). One observer (R.A.), who was blinded to the clinical findings of the patients (e.g., visual acuity and ERM grade), measured the retinal layer thickness and assessed the status of the IS/OS junction.
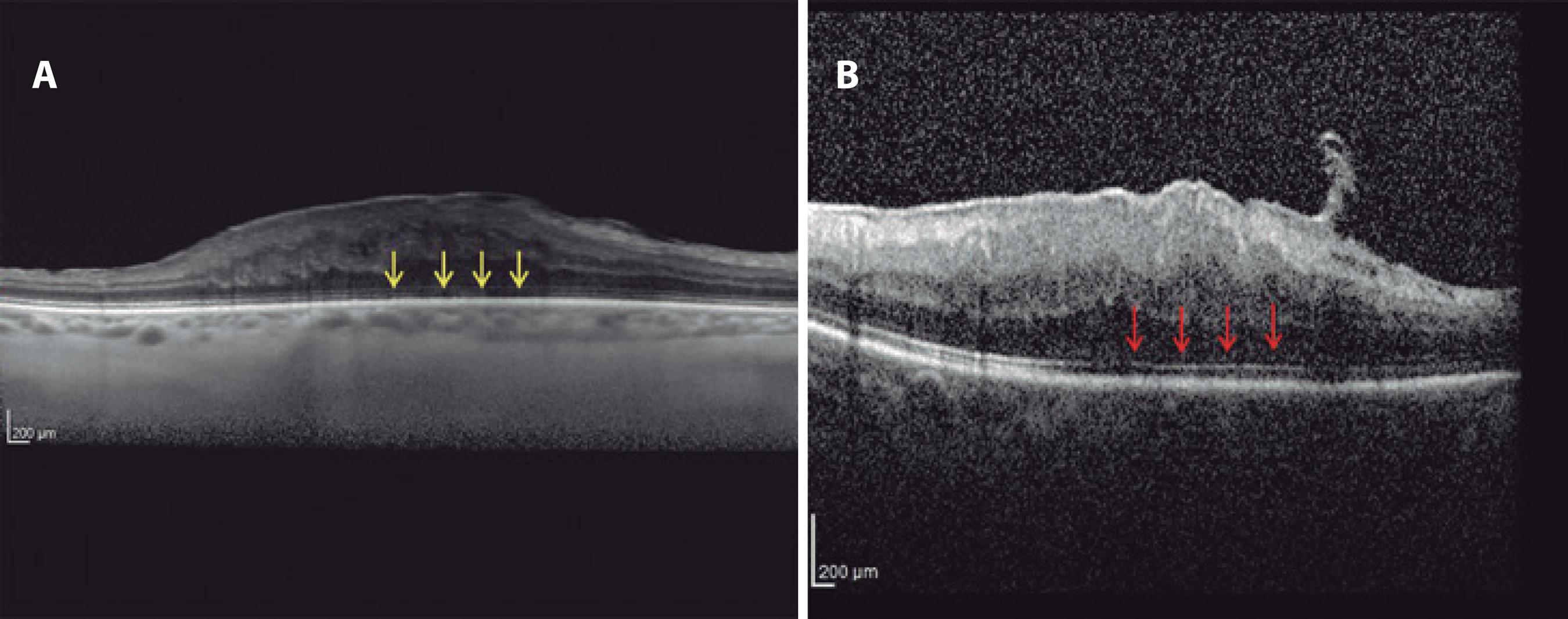
Figure 2 A) Example of an intact inner segment/outer segment (IS/OS) junction. B) Example of a disrupted IS/OS junction (arrow).
Correlations of BCVA with age, central retinal thickness, ERM grade, and IS/OS disruption were evaluated using linear regression analysis. In addition, eyes were divided into three groups with respect to ERM grade: group 1, eighteen (33.3%) eyes with grade 1 ERM; group 2, 21 (38.9%) eyes with grade 2 ERM; and group 3, 15 (27.8%) eyes with grade 3 ERM. The relationships of IS/OS disruption, central macular thickness, and BCVA with the ERM grade were also evaluated through linear regression analysis.
Statistical analysis
SPSS version 11.6 (SPSS, Inc., Chicago, IL, USA) was used for the statistical analysis. Visual acuity values weres converted to logMAR units for the statistical analyses. In addition to the linear regression analyses mentioned above, a one-way analysis of variance with a post-hoc Tukey's test was used to compare the three groups with respect to BCVA and central macular thickness. Categorical variables were compared between the groups with the χ2 test. A P value <0.05 was considered statistically significant.
RESULTS
Of the 54 patients, 20 (37.0%) were men and 34 (63.0%) were women. The mean age of the patients was 67.9 ± 9.2 years (range: 41-84 years). In addition, the mean logMAR visual acuity and mean central retinal thickness were 0.4 ± 0.32 (range: 0.0-2.0) and 462.6 ± 119.8 μm (range: 271-877 μm), respectively. Twenty-nine (53.7%) of the eyes exhibited IS/OS disruption. Notably, the correlation of age with BCVA was not significant (r2=0.018, p=0.334). However, BCVA exhibited significant correlations with central retinal thickness (r2=0.531, p=0.000), IS/OS disruption (r2=0.304, p=0.000), and ERM grade (r2=0.287, p=0.000). The characteristics and clinical data of the patients are shown in table 1.
Table 1 Characteristics of patients classified according to epiretinal membrane grade
| Group 1 (n=18) | Group 2 (n=21) | Group 3 (n=15) | P value | |
|---|---|---|---|---|
| Age (years) | 66.20 ± 11.20 | 67.80 ± 8.50 | 70.00 ± 7.50 | 0.519 |
| Sex (%) | ||||
| Male/female | 37.8/62.2 | 33.3/66.7 | 41.70/58.30 | 0.300 |
| BCVA | 0.20 ± 0.14 | 0.42 ± 0.22 | 0.64 ± 0.43 | 0.000* |
| CMT (µm) | 383.20 ± 81.60 | 465.50 ± 87.10 | 554.00 ± 135.60 | 0.000* |
| IS/OS junction (%) | ||||
| Disrupted/Intact | 11.1/88.9 | 66.7/33.3 | 86.70/13.30 | 0.000* |
*statistically significant; BCVA= best-corrected visual acuity; CMT= central macular thickness; IS/OS= inner segment/outer segment.
The three groups, stratified according to ERM grade, were compared with respect to age, sex, BCVA, central macular thickness, and IS/OS disruption. Age and sex were found to be similar among the groups (p=0.519 and p=0.300, respectively). In terms of BCVA, groups 1 and 2 differed significantly (p=0.038), whereas the difference between groups 2 and 3 was not statistically significant (p=0.070). Central macular thickness was significantly greater in group 2 compared to group 1 (p=0.031) and in group 3 compared to group 2 (p=0.033).
IS/OS distortion was observed in two (11.1%) of the eyes in group 1, 14 (66.7%) of the eyes in group 2, and 13 (86.7 %) of the eyes in group 3. The difference in IS/OS disruption between groups 1 and 2 was found to be statistically significant (p=0.000), whereas the difference between groups 2 and 3 was not significant (p=0.310). Characteristics of the three groups are shown in table 2.
Table 2 Comparison of BCVA, CMT, and IS/OS disruption between groups
| Mean | P value | |
|---|---|---|
| BCVA (logMAR) | ||
| Group 1 - Group 2 | 0.20 ± 0.14 - 0.42 ± 0.22 | 0.038 |
| Group 2 - Group 3 | 0.42 ± 0.22 - 0.64 ± 0.43 | 0.070 |
| CMT (µm) | ||
| Group 1 - Group 2 | 383.2 ± 81.6 - 465.5 ± 87.1 | 0.031* |
| Group 2 - Group 3 | 465.5 ± 87.1 - 554.0 ± 135.6 | 0.033* |
| Disrupted IS/OS junction (%) | ||
| Group 1 - Group 2 | 11.1 - 66.7 | 0.000* |
| Group 2 - Group 3 | 66.7 - 86.7 | 0.310 |
*statistically significant; BCVA= best-corrected visual acuity; CMT= central macular thickness; IS/OS= inner segment/outer segment.
DISCUSSION
Retinal traction caused by an ERM leads to morphological changes that affect the entire retina, including the photoreceptor layer, rather than merely the superficial layers. This characteristic is important because longstanding morphological changes in the retina can lead to irreversible functional damage. Extensive studies of the integrity of the photoreceptor IS/OS line have demonstrated a significant association between an intact IS/OS line and better postoperative BCVA after successful removal of an ERM(6,7,10,14). Inoue et al.(6) evaluated the prognostic value of IS/OS line integrity and observed significantly better postoperative BCVA in patients with an intact IS/OS junction pre-operation. Furthermore, using preoperative SD-OCT scans, Cobos et al.(15) observed significantly better postoperative BCVA in eyes with an intact IS/OS junction, compared to eyes with an irregular or disrupted IS/OS junction.
In another study of 41 patients who underwent surgery for ERM, potential prognostic factors that may influence functional outcomes were investigated. Notably, the baseline CRT and appearance of the foveal contour did not significantly influence distance and near visual acuity outcomes at 3-month follow-up. However, patients with a continuous or interrupted IS/OS line exhibited significant improvements in distance and near visual acuity at 3 months, as well as a significantly higher rate of improvements in both distance and near visual acuity, compared to patients with a nearly absent IS/OS line(7). Suh et al.(8) evaluated 101 eyes of 101 patients with idiopathic ERM who underwent PPV for ERM removal. OCT-detected photoreceptor disruption, which was potentially irreversible, was found to be a good predictor of poor visual outcomes in eyes with idiopathic ERM. The authors postulated that early membrane removal might prevent additional photoreceptor damage in ERM patients with photoreceptor disruption. In the present study, the central macular thickness increased significantly as the ERM grade increased. In addition, differences in IS/OS disruption rates and BVCA were only significant between patients with grade 1 and grade 2 ERM. We believe that these findings suggest the presence of IS/OS disruption, even at early stages of ERM, and indicate that the main disruption occurs between grades 1 and 2.
Mitamura et al.(10) used OCT to evaluate 70 eyes of 70 consecutive patients who underwent vitrectomy for idiopathic ERM; evaluations were conducted before and at 3 and 6 months after surgery. In that study, the preoperative IS/OS junction grade correlated significantly with BCVA at 6 months. However, central foveal thickness did not correlate with BCVA between 3 and 6 months. Massin et al.(16) also reported that the preoperative macular thickness did not correlate with the postoperative BCVA. In our study, the correlation of CMT with BCVA was stronger than the correlation of IS/OS with BCVA. Interestingly, the IS/OS disruption rate and mean BCVA did not differ between grade 2 and 3 ERMs, whereas the mean CMT was higher in grade 3 ERMs relative to grade 2 ERMs.
Suh et al.(8) reported that 12 of 37 eyes (32.40%) with a postoperatively disrupted IS/OS junction possessed an intact preoperative IS/OS junction; in contrast, only 5 of the 64 eyes (7.81%) with an intact IS/OS junction exhibited a preoperatively disrupted IS/OS junction. As we think that IS/OS disruption begins during the early stages of ERM, we suggest that early membrane removal should be considered to prevent additional photoreceptor damage in patients with ERM.
We must note some limitations of the present study. Notably, the study featured a retrospective design and lacked a control group. In addition, only a small number of patients were included, and this might have affected the reliability of the statistical analysis.
In conclusion, the IS/OS junction appears to be disrupted during the early stages of ERMs. Grade 3 ERMs had a significantly higher incidence of IS/OS disruption, a finding that suggested by the poorer surgical outcomes reported in other studies. Future prospective studies with larger sample sizes are needed to determine the relationship between the IS/OS junction and ERM development.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

