INTRODUCTION
Excimer laser ablation is an effective method for correcting errors of refraction either by surface treatment or by applying laser under a corneal flap. Postoperative results depend on proper centration of the ablation profile on the cornea. Customized excimer laser correction may enable individualized higher-order aberration correction(1). However, centration and compensation for cyclotorsion are crucial in these cases. Many patients were noted to have a cyclotorsion of their eyes when shifting from erect to supine position, with one study reporting as much as 96% of eyes having cyclotorsion(2) and a different study reporting an amount as high as 9.5º(3). Compensation for the cyclotorsion is particularly important in irregular corneas undergoing topography-guided ablation, in eyes with a significant cylindrical component, or when a wavefront-guided treatment is desired. Not all laser platforms are able to automatically correct for the cyclotorsion(4,5). The Schwind Excimer Laser Platform takes eye movements into account and compensates before and during the excimer treatment.
Previous reports have described the effect of centration and cyclotorsion correction on postoperative cylinder and uncorrected visual acuity (UDVA) in eyes with spherocylindrical errors of refraction(1,2,6,7). Here we report the efficacy, reliability, and reproducibility of Static Cyclotorsion Correction (SCC) measurement using the Schwind Amaris excimer laser in eyes undergoing LASIK or t-PRK refractive surgery. We also report the time taken for cyclotorsion measurements and compare the results of treating astigmatism with and without SCC.
METHODS
This is a prospective study conducted on 80 eyes of 40 patients operated in the Ophthalmic Consultants of Beirut, Jal el Dib, Lebanon between the months of May and July of the year 2012. The study was approved by the institutional review board and the ethics committee of the Ophthalmic Consultants of Beirut. This study adhered to the Declarations of Helsinki.
Preoperative testing
Patients wearing soft contact lens were asked to remove their lenses for at least two weeks prior to performing the topography. Patients wearing hard contact lens were not included in this study. The preoperative screening consisted of a complete ophthalmic workup, including UDVA, corrected distance visual acuity (CDVA), manifest refraction, ocular motility, and a full slit lamp examination, which included a dilated fundus examination. Patients also underwent a corneal wavefront analysis using the Keratron Scout Optikon 2000 Corneal Wavefront Analyzer (Optikon 2000 S.p.A., Rome, Italy), an ocular wavefront measurement using the Ocular Wavefront Analyzer (Schwind Eye-Tech Solutions, GmbH, Kleinostheim, Germany), and a Placido-Scheimpflug topography using the Orbscan IIZ (Bausch and Lomb, Rochester, NY). Images used for comparisons of SCC were obtained using the Keratron analyzer. For imaging, the patient was asked to sit erect and the head was adjusted to be straight. The head was positioned such that the vertical axis of the nose was perpendicular to the chin rest. The patient was also asked to look at the fixation light positioned at the center of the machine with their eyes open. No speculum or digital lid opening was performed. An experienced optometrist made all measurements. At least 3 measurements were made, which were used for assessing the reproducibility using a reproducibility curve. Only the best measurements were used in later analyses. Pupil centroid shift was recorded and the laser system was compensated for only when the shift was >0.2 mm in magnitude.
All the details of the study including the surgical procedures were explained to the patients in detail. An oral informed consent for measurements and surgery was obtained prior to making the measurements.
Surgical technique and measurements
All procedures were performed by one surgeon (SF) at the same surgical center using a single excimer laser (Schwind Amaris 500 Excimer laser, Schwind Eye-Tech Solutions, GmbH, Kleinostheim, Germany). Both eyes were operated using the same settings. Patients were given 5 mg of diazepam (Valium®) orally 30-40 minutes before the start of the surgery. One drop of propacaine (Novocain®) and one drop of ofloxacin (Oflox®, Allergan) were applied to both eyes on three occasions, each separated by 2 minute-intervals. The patients were asked to lay flat on the laser table and measurements were first made on the right eye. The fellow eye was occluded. Before each measurement, the patient was asked to look at the blinking fixation light and the head was adjusted to eliminate any possible head tilt, with the vertical axis of the nose aligning with the sagittal plane of the body. Care was taken to ensure that the shoulders were lying equally flat on the table. The centration lights of the laser were used on the glabella to ensure that the head was properly positioned (Figure 1, additional video showing the effect of head rotation on the centration lights can be seen online). The eyes were scrubbed and draped. A closed-loop speculum with suction was used. The amount of SCC and the number of "no-catch" trials were recorded before the speculum was placed, after the speculum was placed, and after the flap was lifted (in LASIK eyes). When performing t-PRK (30 eyes, 37.5%), a third set of measurements was not taken and the laser was directly applied to the virgin cornea.
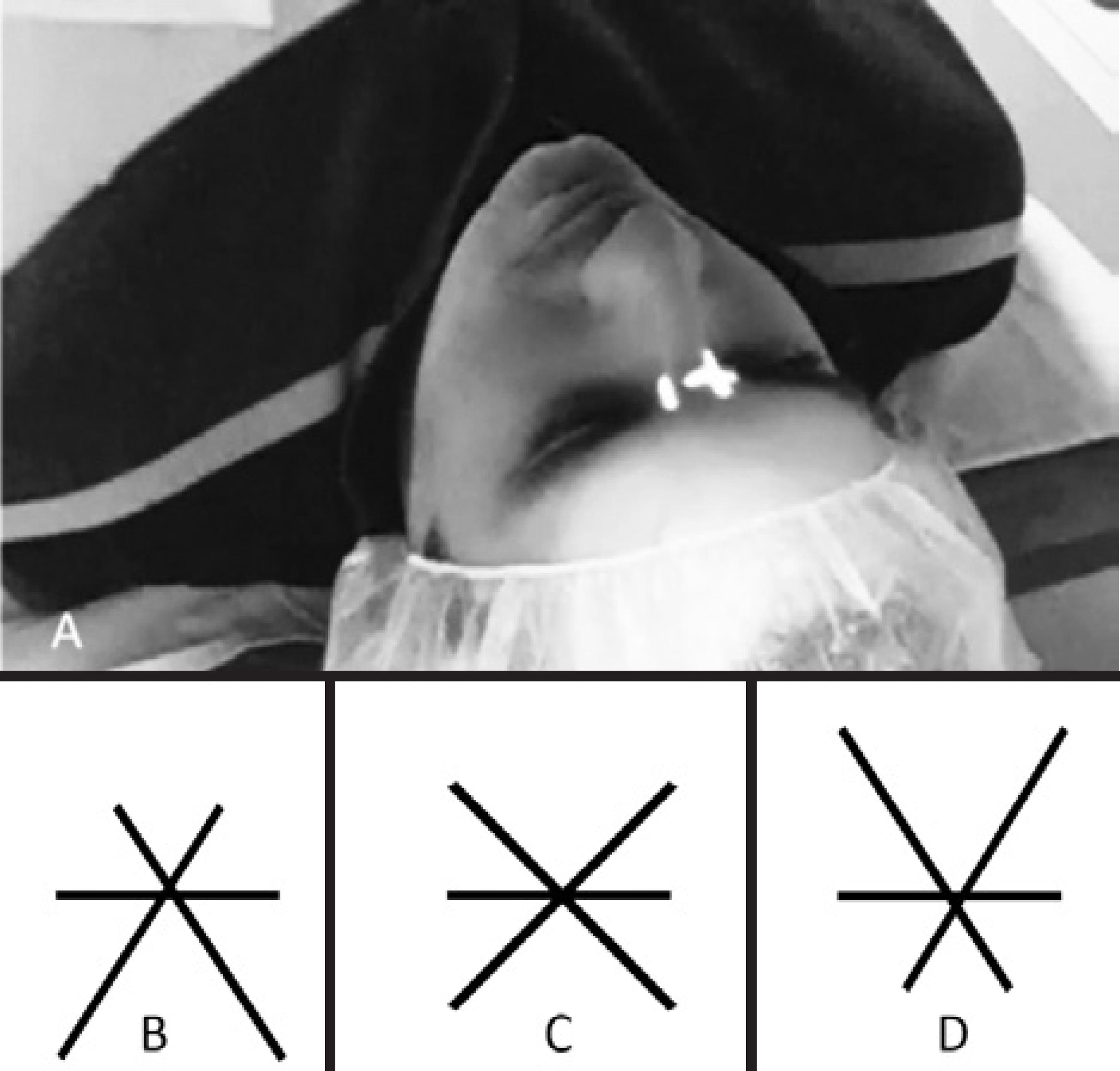
Figure 1 Adjustment of head positioning using the centration lights of the excimer laser on the glabella. A) Patient position on the excimer laser table: shoulders lying flat on the bed and head facing straight at the fixation light. The axis of the nose is aligned with the sagittal axis of the body. Three line-lights are brought into focus and proper superposition as in C). When the chin is tilted excessively down or up, the lights shows pattern B) or D), respectively.
The cornea of the eyes that were to undergo LASIK (50 eyes, 62.5%) was marked and washed with BSS. The suction ring was applied and maintained until the pressure on the console reached a value between 600 and 630 mmHg. The flap was done using the Schwind pendular microkeratome with hinges placed superiorly. The flap was reflected superiorly along its hinge. Patient position was examined and adjusted as described earlier, and a third set of 5-SCC measurements was recorded. Following this, laser ablation was applied. Intraoperative Dynamic Cyclotorsion Control (DCC) was used in all cases.
All patients received the routine postoperative treatment regimen and follow-up, including steroid, artificial tears, and antibiotic drops for the first week, a steroid taper for one month, and artificial tears for at least 3 months( 8). Astigmatism (manifest and cycloplegic cylinder) was measured preoperatively and at 3 months postoperatively. We assessed the postoperative astigmatism and the effect of SCC compensation in the eyes that underwent LASIK.
Variables assessed and statistical analysis
We noted the number of times when SCC could not be measured (percentage "no catch"). The percentage of registration was calculated as, (Eyes in which measurements were successful/Total number of eyes) x 100%. We recorded the amount of cyclotorsion and subcategorized SCC into those with a negative value (counter-clockwise) and those with a positive value (clockwise). Time taken for completing the measurement was also recorded from the moment the "measure" button was pressed on the screen to the time the result was displayed on the screen.
Reproducibility, as indicated by the standard deviation and the accuracy of the measurements were compared. Astigmatism analysis was performed using the polar method of vector analysis( 9) with cycloplegic cylinder values compared. The paired Student t-test was used for statistical analysis. A p-value less than 0.05 was considered statistically significant.
RESULTS
Demographics
This study included 80 eyes of 40 patients with mild to moderate errors of refraction. Thirty eyes (37.5%) underwent t-PRK, and 50 eyes (62.5%) underwent LASIK. The mean age of patients was 23.67 ± 4.19 years. Of the 40 patients, 21 were males (52.5%). The mean preoperative sphere was -3.06 ± 2.82 D (-7.25 D to +4.25 D) with a preoperative cylinder of +1.36 ± 0.98 D (+0.25 D to +3.00 D). The mean preoperative spherical equivalent (SE) was -2.56 ± 2.86 D. All eyes had a preoperative CDVA equal to or better than 20/20.
Ability to measure SCC
We were unable to measure SCC in 30 eyes (37.5%) before the speculum was placed, in 7 eyes (8.8%) after the speculum was inserted, and in 6 eyes (12.0% eyes that underwent LASIK) after the flap was lifted. In 2 eyes (4.0%) that were to undergo LASIK, the SCC measurement was not successful after lifting the flap (no-catch in 5 consecutive measurements). However, the measurement could be made before and after the speculum placement.
The percentage of registration was 62.5% pre-speculum, 91.2% after placing the speculum, and 88.0% after lifting the flap. The percentage of "no catch" in the total number of measurements was 63.8%, 14.9%, and 26.9% pre-and post-speculum placement, and post-flap lift, respectively.
The mean time taken per SCC measurement was 15.1 ± 2.7 seconds (range was 9.0 to 25.0 seconds). The mean time taken for 5 consecutive measurements was 3.6 ± 0.7 minutes (range was 2.0 to 5.5 minutes).
The mean standard deviation between the 5 successive measurements was 2.33º before speculum placement, 1.83º after speculum placement, and 1.96º after flap lift.
The effect of the speculum on SCC measurement
In the eyes with a counter-clockwise rotation, the mean SCC was -4.3º and -3.2º pre-, and post-speculum, respectively (p=0.304), whereas in the eyes with a clockwise rotation, the mean SCC was +4.3º and +4.9º pre-, and post-speculum, respectively (p=0.706).
Before placing the speculum, 11 measurements showed an SCC of 0º (3.3%), 79 measurements (23.6%) showed an SCC of >±2º, and 36 measurements (10.8%) had an SCC of >±5º. After averaging the 5 measurements for each eye, 6 eyes (15.0%) were found to have no cyclotorsion, 35 eyes (43.8%) had a cyclotorsion of >±2º, and 14 eyes (17.5%) had a cyclotorsion of >±5º.
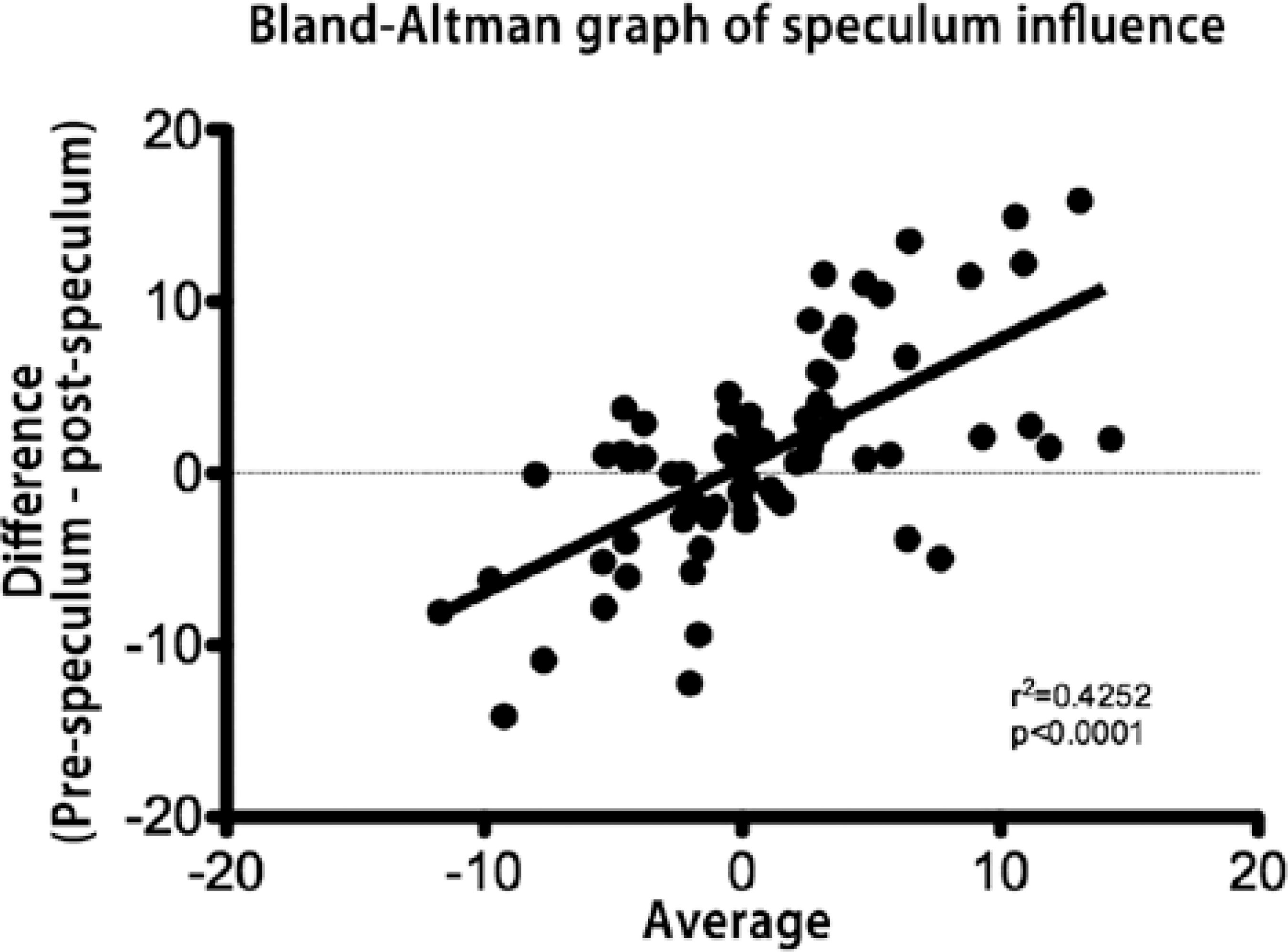
After placing the speculum, 34 measurements showed an SCC of 0º (10.3%), 151 measurements (45.8%) showed an SCC of >±2º, and 88 measurements (26.7%) showed >±5º SCC. After averaging the 5 measurements for each eye, 4 eyes (5.0%) had no cyclotorsion, 33 eyes (41.2%) had a cyclotorsion of >±2º, and 10 eyes (12.5%) had a cyclotorsion >±5º. Table 1 shows the distribution of SCC measurements based on the amount of cyclotorsion. Figure 2 shows the effect of the speculum on the SCC measurements. The Bland-Altman plot shows the difference between measurements made before and after inserting the speculum. The difference was statistically significant and was more pronounced when SCC was >2º.
Table 1 Distribution of static cyclotorsion correction (SCC) measurements based on the amount measured, at each time-point
| Amount | Time-point | % |
|---|---|---|
| 0 ➡ |2|° | Pre-speculum | 33.87% |
| Post-speculum | 46.15% | |
| Post-flap lift | 38.30% | |
| |2.01| ➡ |5|° | Pre-Speculum | 37.30% |
| Post-Speculum | 22.12% | |
| Post-Flap Lift | 38.40% | |
| >±5.01° | Pre-Speculum | 29.00% |
| Post-Speculum | 31.73% | |
| Post-Flap Lift | 22.30% |
The effect of the flap lift on SCC measurement
In the eyes that had a counterclockwise rotation, the mean SCC was -3.2º before lifting the flap and -2.8º after lifting the flap (p=0.138), whereas in the eyes that had a clockwise rotation, the mean SCC was +4.9º before the flap was lifted and +2.0º after lifting the flap (p=0.203).
Before lifting the flap, 34 measurements (10.3%) showed an SCC of 0º, 151 measurements (45.8%) showed >±2º SCC, and 88 measurements (26.7%) had an SCC of >±5º. After averaging the 5 measurements for each eye, 4 eyes (5.0%) showed no cyclotorsion, 33 eyes (41.2%) had a cyclotorsion of >±2º, and 10 eyes (12.5%) had a cyclotorsion of >±5º.
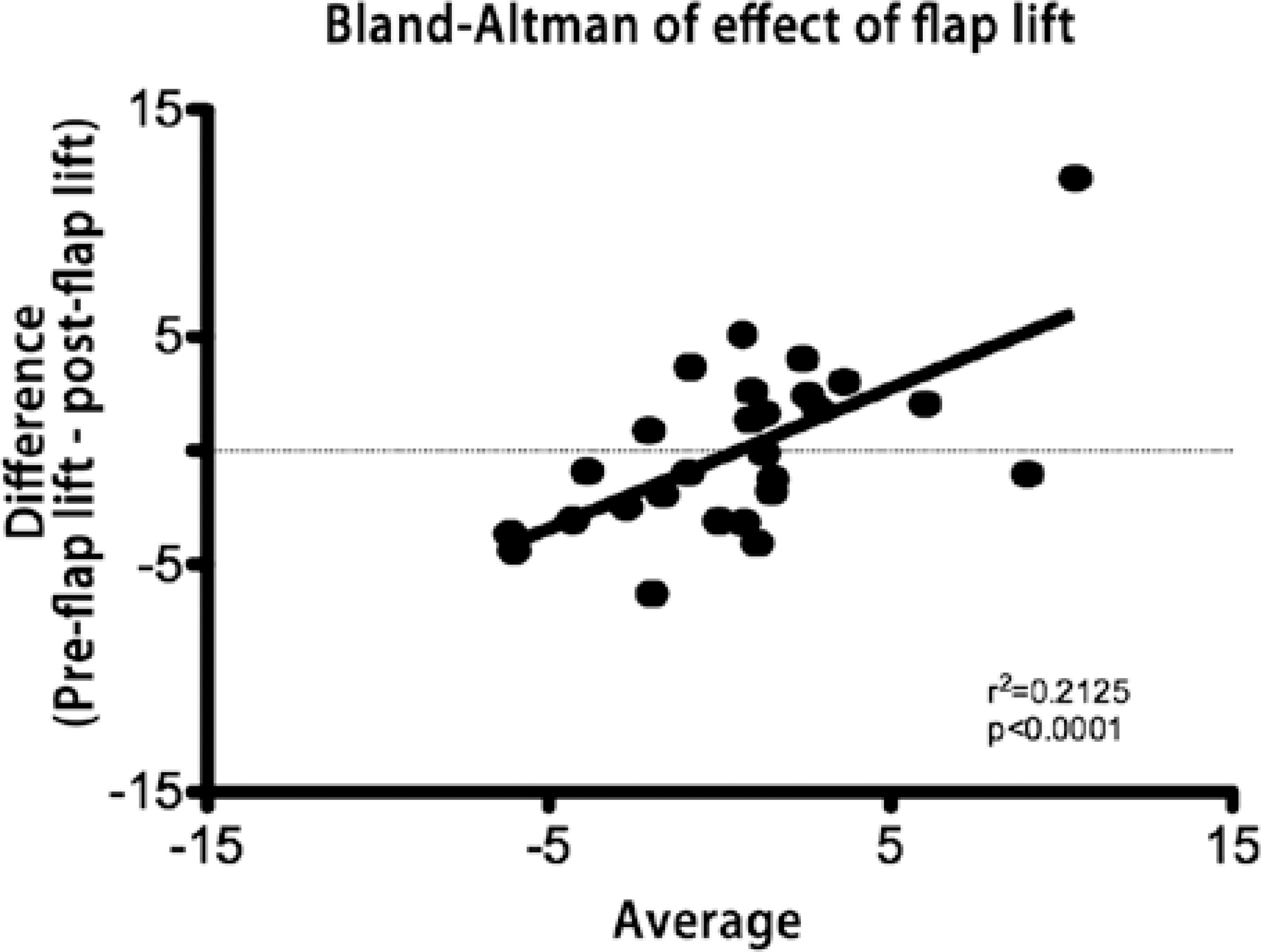
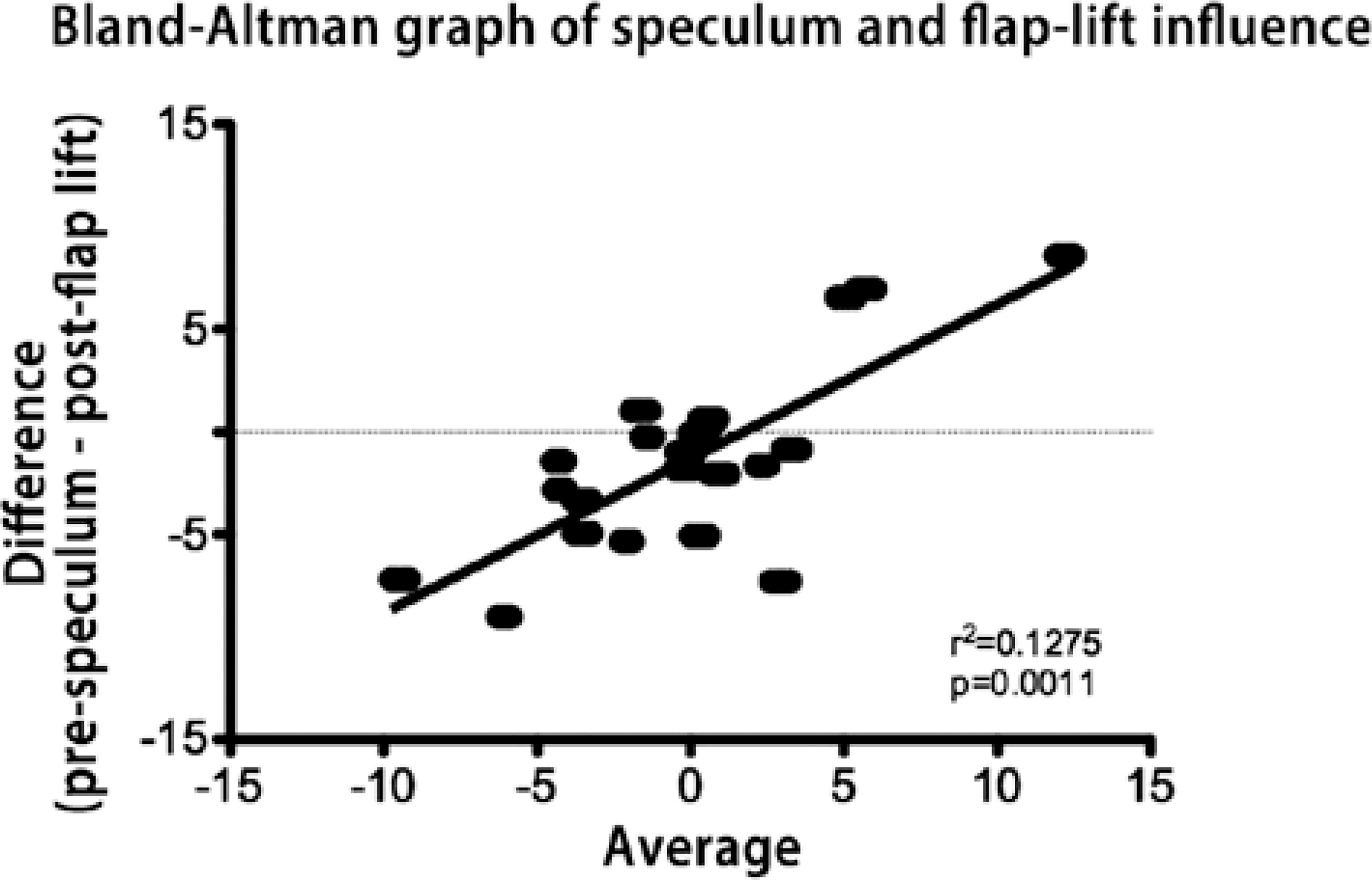
After the flap was lifted, 15 measurements (9.4%) showed an SCC of 0º, 71 measurements (44.4%) showed >±2º SCC, and 25 measurements (15.6%) showed an SCC of >±5º. After averaging the 5 measurements for each eye, 3 eyes (6.0%) showed no cyclotorsion, 33 eyes (66.0%) had a cyclotorsion of >±2º, and 9 eyes (18.0%) had a cyclotorsion of >±5º. Figure 3 shows the Bland-Altman plot of the difference between the measurements made before and after lifting the flap. The difference was statistically significant and was more pronounced when SCC was >2º. Figure 4 shows the Bland-Altman plot of the difference in the measurements made before the speculum placement and after lifting the flap in the eyes that underwent LASIK surgery. There was no statistical significance between the first and the last set of measurements.
Study of astigmatism correction
Among the eyes that had a cylinder between +1.00 D and +2.00 D (40 eyes), those in which SCC measurement was successful (20 eyes) were compared to 20 matched eyes that underwent LASIK in which SCC measurement was not possible. The eyes in which SCC measurement was successful had a preoperative cylinder of +1.53 D@1º as compared to a value of +1.86 D@-1º when SCC was not used (p=0.865). After 3 months of surgery, the mean cylinder became +0.34 D@3º in the eyes where SCC was used and +0.23 D@7º in the eyes where SCC was not used (p=0.611). Both preoperative and postoperative cylinders did not show any statistically significant differences between the groups (p>0.05). Postoperatively, 10% of the eyes had a cylinder ≥1D when SCC was used and 20% when SCC was not used (p<0.001).
DISCUSSION
The SCC measurement on the Schwind Custom Ablation Manager (CAM) platform is based on an algorithm that registers landmarks and patterns on the iris and limbus. These landmarks taken from the topography image are recognized by the cameras of the laser system. The resultant angular difference between the images is recorded as the SCC. In the Schwind Amaris Excimer laser platform, the measurement starts from the center of the iris and rotates spirally, recognizing and registering points on the iris as it rotates. To the best of our knowledge, this is the first study that assessed the accuracy and reliability of SCC measurements made using the Schwind CAM platform. The ablation profile is adjusted to compensate the measured cyclotorsion.
Cyclotorsion can be due to many causes: i) positional (the eyes cyclorotate when the patient assumes a supine position), ii) secondary to head tilt (thus assuring a correct position on the laser bed is crucial), iii) unmasking of a cyclophoria (patients had a motility assessment preoperatively) following monocular occlusion(6,7), or iv) secondary to distortion of the globe by the speculum. Compensating for the induced cyclotorsion as a result of assuming a supine position leads to better results of astigmatism correction(10-12). Although cylinder values of >1 D were not common, we found that this difference was neither statistically nor clinically significant in postoperative cylinder.
It has been reported that the percentage of eyes with "no catch" varies between 5 to 10%(10,13,14). We found that the percentage of "no catch" dropped when the speculum was placed. This was expected since more of the limbus will be exposed when a lid-speculum is placed and blinking is abolished. SCC registration after lifting the flap diminished because the image of the iris is less recognizable due to the stromal dryness.
The mean standard deviation between the 5 successive measurements was 2.3º before speculum placement, 1.8º after speculum placement, and 2.0º after the flap was lifted. Many practitioners opt to measure SCC only once before deciding whether or not to compensate for the SCC while operating. The Schwind Excimer laser software does not store repeated measurements and only allows re-measurements if the surgeon suspects the SCC value. Therefore, it is not possible to have an average of multiple consecutive measurements or to revert to a previously determined value. Additionally, although we rehydrated all corneas initially and after the second set of measurements, the measurement time was long, leading to increased corneal desiccation. The time taken for the SCC measurement could be shortened by the use of a Sirius Schwind (Schwind Eye-Tech Solutions, GmbH, Kleinostheim, Germany) instrument (discussion with company representative).
The variation between the measurements likely originated from various factors-the ocular surface dries out easily when the eye is left open by the speculum (since blinking is suppressed) and the time taken for repeated measurements is relatively long. Additionally, many of the eyes were found to "wiggle and jiggle" before stabilizing.
If the laser system stored data from successive measurements, the surgeon will be able to verify the reproducibility and calculate a weighted average that can be used for customization. Additionally, faster measurements would lead to less corneal dryness and increase the yield of measurements. For custom treatments this becomes a necessity, particularly since rotational malposition can be high(15).
One limitation of this study is that the follow-up was done at 3 months postoperatively. A second limitation is that the precise assessment of the "wiggle and jiggle" that some patients experience during the course of the procedure was not possible since the laser system was not equipped for the continuous video-monitoring of the eye movement.
CONCLUSION
Although the SCC measurement is a simple and straightforward maneuver, the measurement is not always possible. There was no statistically significant difference between the measurements made pre-and post-speculum placement, and post-flap lift. When the cylinder was significant, the residual astigmatism correction was better when SCC was used.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

