INTRODUCTION
Extraocular muscle disease is typically associated with thyroid disease. However, other rarer etiologies such as neoplasms and infection should also be considered(1-4).
Lymphomas are the most common malignant tumors of the orbit in adults, and the majority of these are secondary to other systemic findings(5,6). On the basis of the classification of the World Health Organization (WHO), and with some modifications from the Revised European and American Lymphoma (REAL) classification, the most common histological type is B-cell lymphoma(6-9). Jakobiec recommended the term B-cell lymphoma of the extranodal marginal zone to indicate the histological subtype of soft tissue tumors located in the orbit. He also suggested that the designation of mucosa-associated lymphoma (MALT) was not appropriate for cases of muscle involvement and should be used only for cases of conjunctival, lacrimal gland, and lacrimal sac area involvement(6).
Certain specific areas such as the conjunctiva, infraorbital tissues, lacrimal system, and extraocular muscles show a good response to treatment and a better prognosis (63%, 58%, 28%, and 13%, respectively)(1,6,9). Eyelid involvement is related to a worse prognosis(6).
Here we describe the case of a 55-year-old man with orbital non-Hodgkin B-cell MALT lymphoma and emphasize its atypical presentation as medial rectus muscle myositis.
CASE REPORT
A 55-year-old presented with progressive eye pain and low visual acuity in the right eye since 2 years. His past medical history was unremarkable, and he denied the use of any medications. He had previously undergone treatment for glaucoma in both eyes with travaprost and brimonidine. During the ophthalmologic examination, his visual acuity was 20/70 in the right eye and counting fingers at 1.5 m in the left eye. The right eye exhibited proptosis (exophthalmometry base 100 = 31 mm in the right eye and 14 mm in the left eye), which was associated with chemosis, conjunctival hyperemia, lower eyelid retraction, exotropia, and ocular motility limitation (Figure 1). There was no palpable regional lymphadenopathy. According to Goldmann tonometry, his intraocular pressure was 32 mmHg in the right eye and 30 mmHg in the left eye. Fundoscopy revealed a cuptodisc ratio of 0.9 × total in the right eye and 0.7 × 0.8 in the left eye, with no other changes. Computed tomography (CT) and magnetic resonance imaging (MRI) of the orbit showed a significantly larger fusiform medial rectus muscle in the right eye, with tendon involvement (Figure 2).

Figure 1 Ectoscopy showing chemosis, conjunctival hyperemia, lower eyelid retraction, exotropia, and limited ocular motility in the right eye
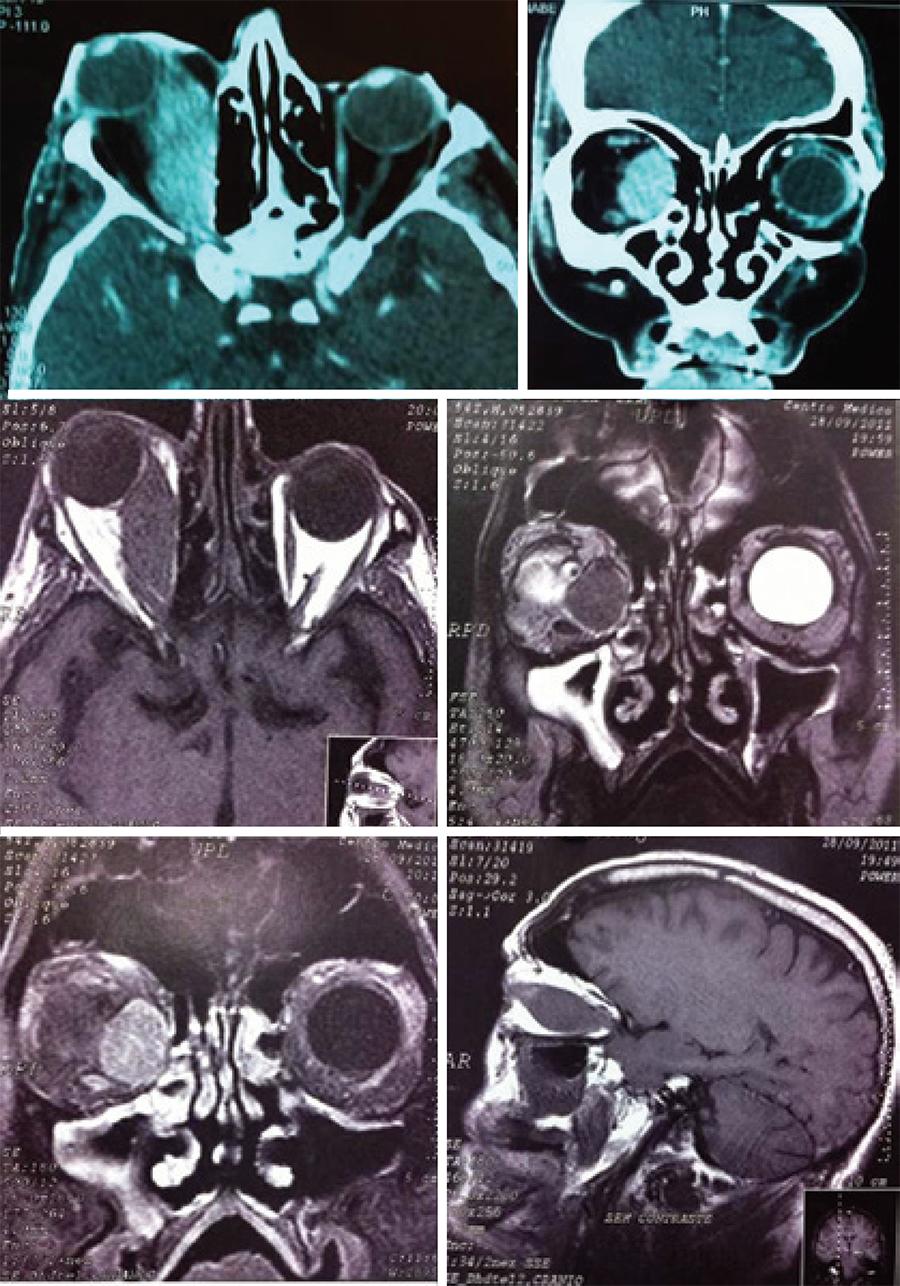
Figure 2 Computed tomography (two photos above) and magnetic resonance imaging (four photos below) of the orbit show that the optic nerve is deflected upward and to the side, with fusiform enlargement of the right medial rectus muscle in full extension, tendon involvement, no damage to the bones of the orbital wall, and no signs of cortical erosion
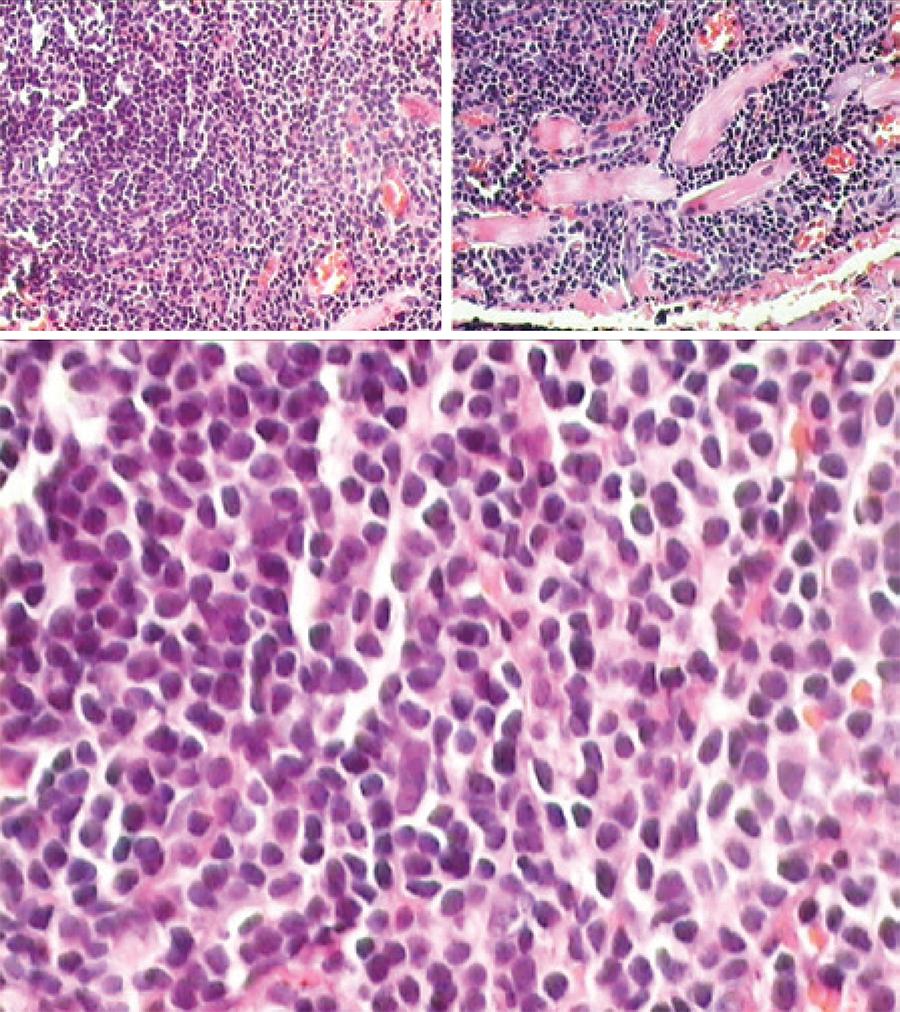
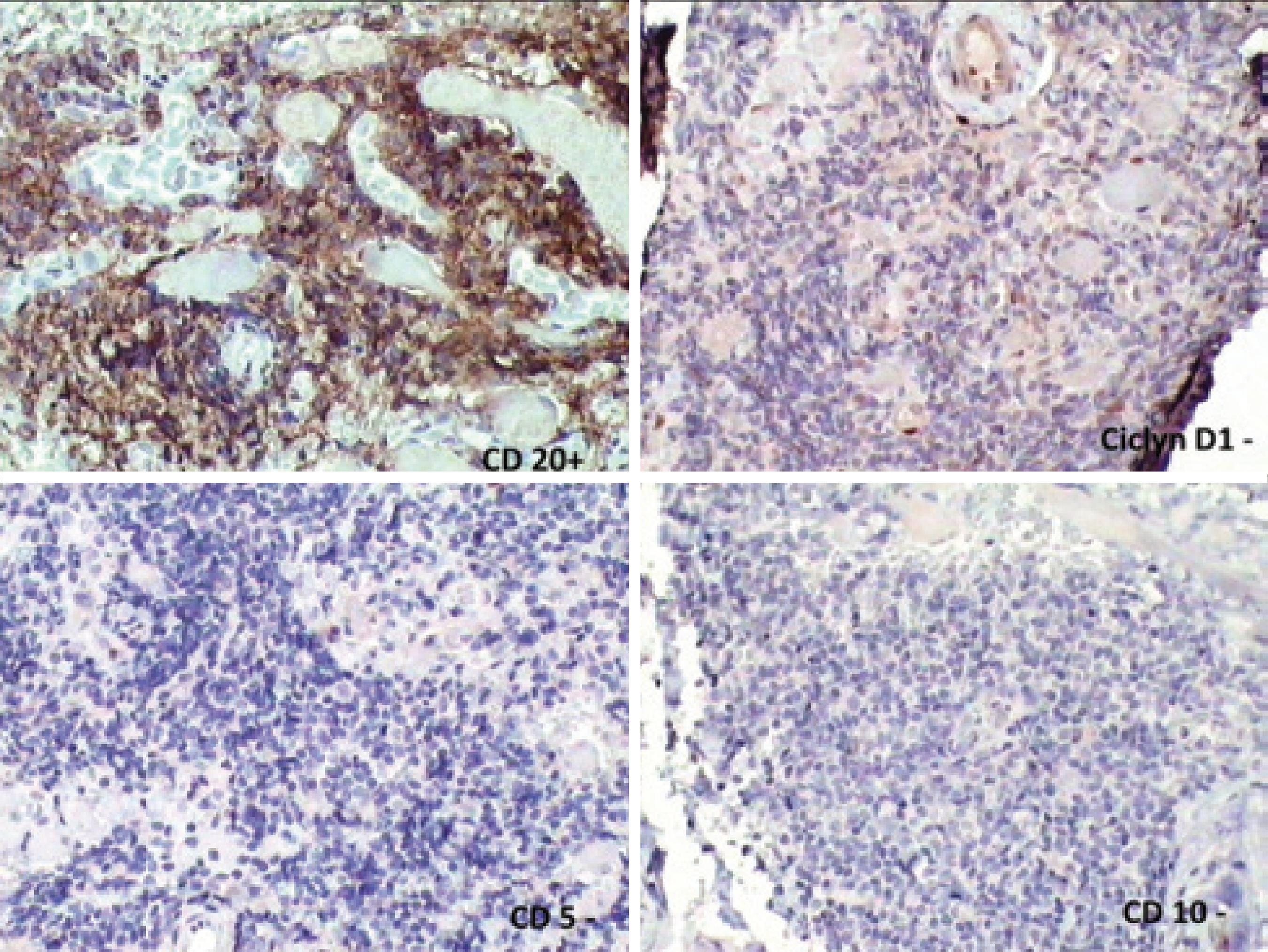
The patient's routine laboratory tests were normal, including thyroid hormones and antibodies. The Mantoux test (purified protein derivative; PPD) was strongly reactive (22 mm). A biopsy was scheduled, and the hematoxylineosin staining of the biopsied tissue showed a relatively homogeneous small cell population with slight nuclear irregularity, inconspicuous nucleoli, and scant cytoplasm (Figure 3). Immunohistochemistry confirmed non-Hodgkin B-cell MALT lymphoma that was CD20 (+), CD3 (+), cyclin D1 (-), CD5 (-), CD10 (-), CD23 (-), and BCL2 (-) (Figure 4). The patient was referred to the hematology department for systemic staging and treatment.
DISCUSSION
The extraocular muscles may be involved in several systemic diseases, initially manifesting as orbital myositis. The most common etiology of this pathology in the orbit is Graves' ophthalmopathy, which is an organspecific autoimmune process with inflammation, edema, and secondary fibrosis. Bilateral symmetric muscle involvement is observed in 70% patients. The usual pattern of clinical involvement in decreasing order of frequency is as follows: inferior, medial, superior, and lateral muscles(3).
In our patient, Graves' ophthalmopathy was the first diagnostic hypothesis according to the history and clinical findings. Therefore, we requested laboratory tests and imaging studies to confirm this hypothesis. Because the thyroid profile and antithyroid antibodies were normal and CT and MRI findings were unremarkable, the hypothesis of Graves' ophthalmopathy became less likely. During our search for the specific etiology, we also considered infectious causes, which are very common in our country. Then, we asked for several serologies and a PPD, which was the only positive test. At that time, our diagnosis was tuberculosis myositis. To confirm this hypothesis and initiate specific treatment, we performed an incisional biopsy, which, to our surprise, revealed non-Hodgkin B-cell MALT lymphoma.
The causes of nonthyroidrelated enlargement of the extrinsic muscles are diverse and include inflammatory (idiopathic, sarcoidosis, Crohn's disease, systemic lupus erythematosus, rheumatoid arthritis, and Wegener's granulomatosis), vascular (carotid-cavernous fistula and arteriovenous malformation), neoplastic (metastatic, secondary or primary), infectious (secondary to orbital cellulitis or primary), depositionrelated (amyloid), traumatic, and iatrogenic causes(3). Despite its rare occurrence, orbital lymphomas should be considered in the differential diagnosis of this type of condition(3). Another rare etiology that should be considered, particularly in endemic regions such as Brazil, is myositis caused by tuberculosis(4).
Lymphomas with the presentation of myositis and no other symptoms are very rare in the scientific literature. The largest series of ocular adnexal lymphomas described in the scientific literature (353 cases) do not describe this type of clinical presentation. There have been few revisions or only isolated case reports(1,2,5,7-9). Different authors have mentioned diplopia, periorbital inflammation, restriction of motility, and proptosis as the main clinical findings(1,5,7-9). Such symptomatology may suggest the impairment of ocular muscles. Watkins et al. and Lacey et al. mention that the upper muscles are more frequently involved, particularly the superior rectus and the superior oblique muscles, respectively(1,3). Lacey et al. also determined that the disease is usually unilateral, describing only one patient with symmetrical bilateral infiltration(3). In our patient, there was unilateral involvement of the medial rectus muscle, as observed in the case described by Rossman et al.(2). Histologically, the muscle involvement is mainly nodular and does not spare the tendons(1,3).
The clinical presentation of non-Hodgkin B-cell MALT lymphoma or extranodal marginal zone lymphoma in the orbit is indolent with a low risk of progression in the bone marrow, indicating a good prognosis in most cases(2,3). Our patient was symptomatic for 2 years and had no metastasis, emphasizing the indolent course of the disease.
Imaging studies such as CT and MRI allow for the observation of the increased thickness of the affected muscle and tendon involvement. This information, together with the clinical signs and pathology, can confirm the diagnosis. In our patient, imaging studies revealed tendon involvement, which suggested a differential diagnosis of Graves' ophthalmopathy. In imaging studies, other characteristics of thyroid ophthalmopathy that may be observed include welldefined fusiform enlargement of the muscle (especially posteriorly) with smooth borders, no tendon enlargement, normal orbital fat, preseptal edema, and lacrimal gland prolapse(3).
Confirmation of the diagnostic biopsy with immunohistochemistry is essential, and the usual findings are as follows: CD 20 (+), CD 43 (+), BCL 6 (-) MUM1 (-), p16 (+), p21 (-), pRB (-) p53 (-), and cyclin D1 (-)(3). Our patient was CD 20 (+), CD 10 (-), CD 23 (-), BCL2 (-), and cyclin D1 (-) in B-cells and CD3 (+) and CD 5 (+) in Tlymphocytes. Genetically, the translocations most frequently encountered are t (3;14) (p14.1;q32) involving FOXP1 and IgH and t(14;18)(q32;q21) involving IgH and MALT1( 6,10).
When the diagnosis of non-Hodgkin B-cell MALT lymphoma was established, we immediately sent the patient to the Hematology department of UNIFESP for treatment. Multidisciplinary evaluation and systemic staging was mandatory because of good response to treatment and good prognosis.
In conclusion, the findings from our case indicate that it is important to consider lymphoma as one of the differential diagnoses in cases of isolated myositis, although Graves' ophthalmopathy should continue to be the first diagnosis to be considered.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

