

Antônio Marcelo Barbante Casella1; Michel Eid Farah2; Maria Cristina Martins3; Alexandre Hasegawa4; Ana Paula Miyagusko Taba Oguido1
DOI: 10.1590/S0004-27492008000600025
ABSTRACT
This study correlates fluorescein angiography (FA) and indocyanine green angiography (ICGA) to histopathologic findings in a patient with sympathetic ophtalmia. A male with a perforated trauma in right eye presented after two months a decrease in visual acuity of the left eye. FA and ICGA were performed and the images were correlated with the histopathologic findings of the enucleated eye; FA showed background areas of homogeneous hypofluorescence in the arterial and venous phases, as well as areas of granular progressive hyperfluorescence and leakage from the optic disc. ICGA showed areas of hypofluorescence in the early and intermediate phases of the examination, which persisted until the late phase. During the early phase, there was also diffuse hypofluorescence caused by blockage that allowed observation of areas of partial choroidal circulation. The histopathology of the enucleated right eye showed diffuse choriocapillaris edema and inflammation of the choroids, focal areas of hyperplasia of the retinal pigment epithelium (RPE) as well as foci of epithelioid cells located between the choroid and the RPE. Furthermore, lymphocytic infiltration of the episcleral veins and retinal detachment were present. The hyperfluorescence observed on FA was correlated to retinal detachment and optic nerve inflammation. The hypofluorescence noted on FA and ICGA corresponded to the presence of blocking inflammatory cells (Dalen-Fuchs-like nodules) and to diffuse choriocapillaris edema.
Keywords: Ophthalmia, sympathetic; Fluorescein angiography; Indocyanine green; Case reports
RESUMO
O objetivo deste relato de caso foi correlacionar achados da histopatologia com a angiografia por fluoresceína (AF) e por indocianina verde (AIV) em um paciente com oftalmia simpática. Após dois meses de trauma perfurante no olho direito, o paciente apresentou baixa acuidade visual no olho esquerdo (OE). A AF do OE mostrou áreas de hipofluorescência homogênea na fase arterial e venosa, áreas de progressiva hiperfluorescência granular e vazamento do disco. A AIV mostrou áreas de hipofluorescência na fase inicial à tardia. A histopatologia foi realizada após evisceração do olho direito e demonstrou difuso edema da coriocapilar, inflamação da coróide, áreas focais de hiperplasia do epitélio pigmentar da retina, focos de células epitelióides entre a coróide e o epitélio pigmentar da retina, além da infiltração linfocitária das veias episclerais e descolamento de retina. A hiperfluorescência observada na AF foi correlacionada com o descolamento de retina e inflamação do nervo óptico. A hipofluorescência na AF e AIV correspondeu à presença de células inflamatórias (nódulos de Dalen-Fuchs) e edema coriocapilar difuso.
Descritores: Oftalmia simpática; Angiofluoresceinografia; Verde de indocianina; Relatos de casos
RELATOS DE CASOS
Sympathetic ophthalmia - histopathological correlation with fluorescein and indocyanine green angiography: case report
Oftalmia simpática - correlação da histopatologia com a angiografia por fluoresceína e indocianina verde: relato de caso
Antônio Marcelo Barbante CasellaI; Michel Eid FarahII; Maria Cristina MartinsIII; Alexandre HasegawaIV; Ana Paula Miyagusko Taba OguidoV
IMD. Medical Doctor at Universidade Estadual de Londrina - UEL - Londrina (PR) - Brazil
IIMD. Medical Doctor at Universidade Federal de São Paulo - UNIFESP - São Paulo (SP) - Brazil
IIIMD. Medical Doctor at Faculdade de Medicina de Jundiaí - Jundiaí (SP) - Brazil
IVMD. Medical Doctor at Hospital de Olhos de Londrina (PR) - Brazil
VMD. Medical Doctor at UEL - Londrina (PR) - Brazil
ABSTRACT
This study correlates fluorescein angiography (FA) and indocyanine green angiography (ICGA) to histopathologic findings in a patient with sympathetic ophtalmia. A male with a perforated trauma in right eye presented after two months a decrease in visual acuity of the left eye. FA and ICGA were performed and the images were correlated with the histopathologic findings of the enucleated eye; FA showed background areas of homogeneous hypofluorescence in the arterial and venous phases, as well as areas of granular progressive hyperfluorescence and leakage from the optic disc. ICGA showed areas of hypofluorescence in the early and intermediate phases of the examination, which persisted until the late phase. During the early phase, there was also diffuse hypofluorescence caused by blockage that allowed observation of areas of partial choroidal circulation. The histopathology of the enucleated right eye showed diffuse choriocapillaris edema and inflammation of the choroids, focal areas of hyperplasia of the retinal pigment epithelium (RPE) as well as foci of epithelioid cells located between the choroid and the RPE. Furthermore, lymphocytic infiltration of the episcleral veins and retinal detachment were present. The hyperfluorescence observed on FA was correlated to retinal detachment and optic nerve inflammation. The hypofluorescence noted on FA and ICGA corresponded to the presence of blocking inflammatory cells (Dalen-Fuchs-like nodules) and to diffuse choriocapillaris edema.
Keywords: Ophthalmia, sympathetic/pathology; Fluorescein angiography; Indocyanine green; Case reports [Publication type]
RESUMO
O objetivo deste relato de caso foi correlacionar achados da histopatologia com a angiografia por fluoresceína (AF) e por indocianina verde (AIV) em um paciente com oftalmia simpática. Após dois meses de trauma perfurante no olho direito, o paciente apresentou baixa acuidade visual no olho esquerdo (OE). A AF do OE mostrou áreas de hipofluorescência homogênea na fase arterial e venosa, áreas de progressiva hiperfluorescência granular e vazamento do disco. A AIV mostrou áreas de hipofluorescência na fase inicial à tardia. A histopatologia foi realizada após evisceração do olho direito e demonstrou difuso edema da coriocapilar, inflamação da coróide, áreas focais de hiperplasia do epitélio pigmentar da retina, focos de células epitelióides entre a coróide e o epitélio pigmentar da retina, além da infiltração linfocitária das veias episclerais e descolamento de retina. A hiperfluorescência observada na AF foi correlacionada com o descolamento de retina e inflamação do nervo óptico. A hipofluorescência na AF e AIV correspondeu à presença de células inflamatórias (nódulos de Dalen-Fuchs) e edema coriocapilar difuso.
Descritores: Oftalmia simpática/patologia; Angiofluoresceinografia; Verde de indocianina; Relatos de casos [Tipo de publicação]
INTRODUCTION
Sympathetic ophthalmia (SO) is a rare bilateral granulomatous panuveitis that occurs following ocular perforation or surgical trauma. The occurrence of SO is estimated to be 0.4 to 1.4% of all uveitis and 0.1 to 0.3% of all traumatized eyes(1).
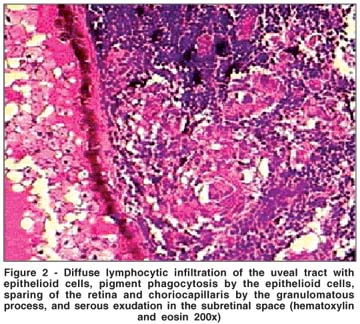
Histopathologic examination indicates a diffuse granulomatous inflammation of the uveal tract, composed primarily of loosely or tightly aggregated epithelioid cells, with preservation of choriocapillaris and retina. Yellowish-white nodules (Dalen-Fuchs) are observed between Bruch's membrane and retinal pigment epithelium (RPE) and contain macrophages, abnormal retinal pigment cells, epithelioid cells and T-lymphocytes(2).
Fluorescein angiography (FA) and more recently, indocyanine green angiography (ICGA) have been useful tools in the diagnosis and management of SO(3-4). FA findings vary and may show either hypofluorescent spots that represent the blockage by foci of cellular infiltration in the superficial choroid or hyperfluorescence in late phases possibly secondary to slow leakage of dye through the RPE beneath exsudative retinal detachment, as well as from optic disc staining. In some cases, only ICGA can detect hypofluorescent spots that represent blockage by edema as well as inflammatory infiltration in the choroid and overlying the RPE(3,5-7).
The purpose of this study was to correlate the FA and ICGA findings with the histopathologic features of a patient with the clinical diagnosis of SO.
CASE REPORT
A 53-year-old male farmer reported a reduction of visual acuity (VA) and pain in the left eye (LE) for the last three days after a history of penetrating ocular injury in the right eye (RE) with a thorn two months previously with no surgical repair.
The VA was no light perception in the RE and counting fingers at 2 meters in the LE. RE biomicroscopy showed a leukomatous corneal neovascularization, and the intraocular pressure (IOP), as well as the fundoscopy, were impossible to determine. The LE presented mild conjuntival hyperemia, cornea with thin keratic precipitates, and the anterior chamber with Tyndall, flare, fibrine. There was and mild opacification of the lens (1+/4+). IOP was 9 mmHg. Ophthalmoscopy showed a moderate vitreitis, optic disk edema, yellowish-white infiltrating spots at the level of RPE (Dalen-Fuchs nodules), serous retinal detachment in the inferior temporal and macular region as well as nasal and temporal serous choroidal detachment.
The ultrasonography diagnosed total retinal detachment in the RE and serous retinal detachment with choroidal thickening in the LE. FA and ICGA studies were performed with the Ophthalmic Imaging System, OIS 1024 Fundus Camera, USA, by injecting respectively 2.5 cc 20% sodium fluorescein and 25 mg indocyanine green. FA showed areas of hypofluorescence in the arterial and venous stages as well as pinpoint granular progressive hyperfluorescence in the areas of serous retinal detachment during all phases of the examination and optic disc leakage during late phases (Figure 1A). ICGA showed large choroidal vessel abnormalities characterized by poor delineation of their walls, areas of hypofluorescence in the early and intermediate phase, which persisted until the late phase of the examination (Figure 1B).
Enucleation treatment of the injured eye was proposed and performed three days after the symptoms started and a high dosis of topical (1 drop each 2 hours) and systemic (100 mg/ prednisone daily) corticosteroids; 1% atropine eye drops every 8 hours were also used. The inflammatory process was resolved and the patient's VA improved to 20/40. Corticoid treatment continued for 6 more months and was then reduced gradually.
Histopathology revealed diffuse lymphocytic infiltration of the uveal tract with epithelioid cell nests, pigment phagocytosis by the epithelioid cells, absence of necrosis, and sparing of the retina and choriocapillaris by the granulomatous process. The inflammatory process also involved the scleral channels. The retina was totally detached with exudation in the subretinal space (Figure 2). The retina structures were disrupted with gliosis and atrophic changes. The anterior segment of the eye was totally disorganized in its normal anatomy and revealed a corneal perforation.
DISCUSSION
SO is defined as a granulomatous, bilateral, diffuse and rare uveitis that occurs as a complication following penetrating trauma, or intraocular surgery. It has been postulated that in its genesis a choroidal and retinal antigens (S and IRBP) would get in touch with the immunological system, causing an autoimmune bilateral reaction(2).
The time between trauma and onset of symptomatology varies from weeks to years in most cases within the first year1 - 65% had happened in the first two months(2,8).
The findings on FA vary according to the literature(4). Some authors(9) showed active SO with typically hyperfluorescent RPE level lesions, in the late phase. And another found thin hyperfluorescence areas in the arterial phase, which corresponded to histopathologic features of Dalen-Fuchs nodules; the optic nerve head may display vascular dilatation and angiographic leakage(10). It has been reported that the typical fundus angiographic appearance is that of multiple early hyperfluorescent sites of choroidal leakage, these sites could correspond to the clinically observed Dalen-Fuchs nodules(4), but in our study we correlated the hyperfluorescent areas with the exudative retinal detachment. The less common appearance of SO is that of early hypofluorescent lesions on angiography; this appearance is similar to that seen in acute multifocal posterior placoid pigment epitheliopathy in which the lesions block the choroidal fluorescence in the early phase and stain in the late phase(4). The RPE status has been correlated whether the Dalen-Fuchs nodules have an intact or a disrupted overlying RPE that determine the hyperfluorescent or hypofluorescent sign in the early phase(4).
In 1998, some authors(3) used ICGA in two patients with SO and showed numerous hypofluorescence areas in the intermediate phase, which became isofluorescent in the late phase. The lesions disappeared with corticosteroid treatment and other areas remained hypofluorescent in the late phase. In our study there were only hypofluorescent areas that also remained in the late phase, probably due to a blockage caused by a choroidal inflammatory cellular infiltration and the choroidal edema. The study(3) does not mention the correlation between these areas with the histopathologic findings, as the ones reported in the present study. We also found poor visualization of the choroidal circulation during the early phase that could be caused either by large choroidal vessel inflammation or overlying retinal edema.
We are unaware of previous reports in Medline of correlation of ICGA and histopathologic findings. This study shows the correlation between the FA and ICGA angiographic and histopathologic findings. The hypofluorescent areas in the ICGA did not corresponded to areas of non-perfusion, but instead they were due to the presence of inflammatory cell blockage and the choriocapillaris edema that was confirmed by the hystopathologic findings. FA is often unable to image through RPE abnormality and does not image choroidal circulation very well, although we could correlate FA progressive hyperfluorescence with the exudative retinal detachment. ICGA would be helpful in these cases of posterior uveitis with choroidal involvement, such as SO for better understanding of the disease and maybe for treatment evaluation.
REFERENCES
1. Chan CC, Roberge RG, Whitcup SM, Nussenblatt RB. 32 cases of sympathetic ophthalmia. A retrospective study at the National Eye Institute, Bethesda, Md., from 1982 to 1992. Arch Ophthalmol. 1995;113:597-600. Erratum in: Arch Ophthalmol. 1995;113(12):1507.
2. Lacerda RR, Nehemy MB. Oftalmia simpática. In: Abujamra S, editor. Retina e vítreo: clínica e cirúrgica. São Paulo: Roca; 2000. Seção VII, cap.1. p.637-9.
3. Bernasconi O, Auer C, Zografos L, Herbort CP. Indocyanine green angiographic findings in sympathetic ophthalmia. Graefes Arch Clin Exp Ophthalmol. 1998; 236(8):635-8.
4. Sharp DC, Bell RA, Patterson E, Pinkerton RM. Sympathetic ophthalmia. Histopathologic and fluorescein angiographic correlation. Arch Ophthalmol. 1984;102(2):232-5.
5. Reynard M, Riffenburgh RS, Minckler DS. Morphological variation of Dalén-Fuchs nodules in sympathetic ophthalmia. Br J Ophthalmol. 1985;69(3):197-201.
6. Yannuzzi LA, Freund KB. Vogt-Koyanagi-Harada Syndrome. In: Yannuzzi LA, Flower RW, Slakter JS, editors. Indocyanine green angiography. St Louis: Mosby; 1997. p.259-69.
7. Bouchenaki N, Herbort CP. The contribution of indocyanine green angiography to the appraisal and management of Vogt-Koyanagi-Harada disease. Ophthalmology. 2001;108(1):54-64.
8. Lottenberg CL, Belfort Júnior R, Abreu MT, Domingues Neto S, Hirata PS, Petrilli AMN, et al. Seis pacientes com oftalmia simpática: experiência de 13 anos. Arq Bras Oftalmol. 1986;49(3):82-5.
9. Lewis ML, Gass DM, Spencer WH. Sympathetic uveitis after trauma and vitrectomy. Arch Ophthalmol. 1978;96(2):263-7.
10. Dreyer WB Jr, Zegarra H, Zacov ZN, Gutman FA. Sympathetic ophthalmia. Am J Ophthalmol. 1981;92(6):816-23.
 Address for Correspondence:
Address for Correspondence:
Antonio Marcelo Barbante Casella
Av. Bandeirantes, 500 - Apto. 109
Londrina (PR) CEP 86010-010 - Brasil
Email: [email protected]
Recebido para publicação em 09.04.2008
Última versão recebida em 20.07.2008
Aprovação em 30.08.2008
Trabalho realizado no Department of Surgery, Section of Ophthalmology of Universidade Estadual de Londrina - UEL - Londrina (PR) - Brazil.
Nota Editorial: Depois de concluída a análise do artigo sob sigilo editorial e com a anuência do Dr. João Borges Fortes Filho sobre a divulgação de seu nome como revisor, agradecemos sua participação neste processo.