

Kenji Sakata1; Maurício Maia2; Leonardo Matsumoto2; Emerson K. Oyamaguchi2; Ana Cristina A. Carvalho3; Northon Knoblauch3; Adilson Gil de Oliveira Filho3
DOI: 10.1590/S0004-27492000000300009
RESUMO
Objetivo: Analisar os valores da pressão intra-ocular (PIO) entre diferentes grupos de pacientes (diabéticos, hipertensos com ou sem retinopatia) e a população normal. Métodos: Realizou-se a aferição da pressão intra-ocular (PIO) em um total de 924 olhos de 482 pacientes com idade igual ou maior que 40 anos (x=56,70; dp=11,89) examinados segundo um protocolo de estudo que incluiu medida da PIO, pressão arterial e glicemia, além da fundoscopia. A determinação da PIO foi obtida pelo tonômetro de aplanação de "Goldmann" e a glicemia foi aferida por meio de tiras reativas (Dextrostix -- Bayer). Em seguida, os pacientes foram divididos em 7 (sete) grupos: hipertensos, hipertensos com retinopatia, diabéticos, diabéticos com retinopatia, hipertensos e diabéticos, hipertensos e diabéticos com retinopatia e a população controle. Resultados: Pelo teste de ANOVA-uma via, numa distribuição normal no nível de significância de 5%, observou-se que o valor médio da PIO é significativamente maior no grupo de pacientes hipertensos sem retinopatia (média PIO=16,10), no grupo dos hipertensos com retinopatia (média PIO=16,33) e no grupo de diabéticos e hipertensos com retinopatia retinopatia (média PIO=16,95). Conclusões: Observou-se que o valor médio da PIO é progressivamente mais elevado conforme o tempo de evolução da doença hipertensiva e também quando esta se encontra associada à diabetes mellitus.
Descritores: Diabetes; Hipertensão; Pressão intra-ocular; Glaucoma
ABSTRACT
Purpose: To correlate the values of intraocular pressure (IOP) obtained by applanation tonometer (Haag-Streit, Bern, Switzerland) in patients with diabetes mellitus (with or without diabetic retinopathy), hypertension (with or without hyper-tensive diabetic retinopathy) and the normal population. Patients and Methods: Subjects participating in the Glau-coma Project (n = 924, 40 or more years old) were examined according to standard protocols including IOP measu-rement, fundoscopy, blood pressure and glucose deter-mination. Patients were divided into seven groups: diabetic patients without diabetic retinopathy, hypertensive patients without hypertensive retinopathy, diabetic hypertensive patients without retinopathy, diabetic patients with diabetic retinopathy, hypertensive patients with hypertensive retinopathy, diabetic hypertensive patients with retinopathy and population-based control. Results: Applying the one-way ANOVA test to a normal distribution at 5% significance, it was observed that IOP values were higher in the groups of hypertensive patients without retinopathy (mean = 16.10), hypertensive patients with hypertensive retinopathy (mean = 16.33) and diabetic hypertensive patients with retinopathy (mean = 16.95) when compared with the other groups. Conclusion: The mean IOP value increases progressively with the evolution of systemic hypertensive disease and when it is associated with diabetes.
Keywords: Diabetes; Hypertension; Intraocular pressure; Glaucoma
Analysis of the intraocular pressure in diabetic, hypertensive and normal patients (Glaucoma Project)
Kenji Sakata (1)
Maurício Maia (2)
Leonardo Matsumoto (2)
Emerson K. Oyamaguchi (3)
Ana Cristina A. Carvalho (4)
Northon Knoblauch (4)
Adilson Gil de Oliveira Filho (4)
INTRODUCTION
Intraocular pressure constitutes the most important risk factor for the emergence of glaucoma 1,2, a pathology often associated with systemic arterial hypertension and diabetes mellitus. According to several studies, no significant relationship between systemic blood pressure and glaucoma has been observed. There is a report on the coexistence of hypertensive disease and glaucoma with normal IOP and glaucoma with high IOP 3.
Diabetes mellitus is an important ocular risk factor 4,5 with the occurrence of retinopathy, certain types of lens opacification (cataract), intraocular pressure increase, rubeosis iridis and possibly open angle glaucoma during its course 5. Many studies have suggested an increase in the relative risk of people with diabetes mellitus to present ocular hypertension during the clinical course of the disease favoring the emergence of open angle glaucoma 5.
The purpose of this study is to observe the intraocular pressure behavior in arterial hypertension and diabetes mellitus which are clinical entities proven to be related to a higher risk for glaucoma development by verifying if there is a significant difference between IOP values in patients with hypertension, diabetes and the control population.
PATIENTS AND METHODS
Nine hundred and twenty-four eyes from 428 patients with age equal to or over 40 years (mean = 56.7 years), 140 (29.04%) being males and 324 (70.95%) females, residents of the city of Curitiba - PR, were studied (data from 11 patients, 21 eyes, were excluded because did could not be included in any of the analyzed groups). These patients were divided into 7 groups as shown in Table 1.

Sequential examination of arterial blood pressure, blood glucose values, fundoscopy and tonometry were performed.
Patients with a systolic blood pressure (SP) ³160 mmHg and/or diastolic blood pressure (DP) ³100 mmHg, assessed by the authors, as well as those with a previous history of arterial hypertension, either under treatment or indicated for, as confirmed during the examination, were considered hypertensives.
Patients were considered diabetics when fasting glucose was above 120 mg/ml or postprandial glucose ³150 mg/dl, by the Dextrostix method, as well as those with a previous diagnosis of diabetes mellitus, under treatment, as confirmed during the examination.
IOP measurements were always performed between 8.00 a.m. and 12.00 p.m. by Goldmann applanation tonometry.
Direct and indirect fundoscopies were performed with the aim to detect lesions due to diabetes mellitus and/or arterial hypertension. In the case of diabetic patients, lesions compatible with proliferative and nonproliferative diabetic retinopathy, such as macular exudate, microaneurysms, dilated and tortuous retinal vessels, retinal hemorrhage, ischemia, macular edema and neovascularization, were searched. In hypertensive patients, the purpose of fundoscopy was to observe alterations in retinal arterioles, cotton-wool spots, exudates, hemorrhage, extensive microvascular alterations and papilledema, according to the classification by Wagener and Keith of 1939 for patients with hypertensive retinopathy.
Eventual findings of other lesions, not characteristic of diabetes mellitus or arterial hypertension, were excluded from this study.
Descriptive analyses showed the values for means, standard deviations, minimum and maximum IOP in all patient groups, in addition to the differences of values in each group.
The one-way ANOVA test, with normal distribution and 5% significance was used to compare the mean IOP values between the studied patient groups.
RESULTS
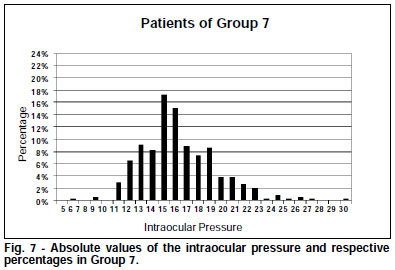
The IOP values of each of the 7 studied groups, their means, standard deviations, minimum and maximum values as well as the number of eyes in each group (total of 914 eyes from 428 patients) are shown in Table 2.

The one-way ANOVA test, by which each group is separately compared with the control group, showed significant values for IOP increase in groups 1, 3 and 6. On the basis of the 5% level of significance, groups 2, 4 and 5 did not show significant results with p = 0.11398, p = 0.47419 and p = 0.74505, respectively.
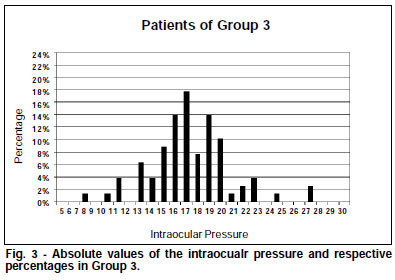
IOP variations found for each group of this study may be seen in Figures 1-7, which show the absolute value of this variable and respective percentage in each group.

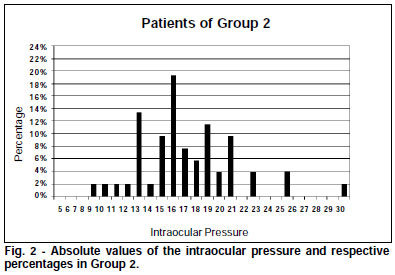



Of the 314 hypertensive patients without retinopathy, 51 (16.24%) showed IOP³19 mmHg, with one value of 60 mmHg, the highest among all groups.
Of the 79 hypertensive patients with hypertensive retinopathy, 17 (21.52%) presented IOP ³ 19 mmHg.
Of the total of diabetic and hypertensive patients with some retinopathy, either diabetic or hypertensive, 11 patients (28.20%) showed IOP ³ 19 mmHg. In this group, p = 0.00526 shown by the one-way ANOVA test was the most significant among the correlated groups.
DISCUSSION
As already mentioned in the Result section, the IOP values increased progressively from the hypertensive patients without retinopathy, to the hypertensive with retinopathy and diabetic hypertensive with retinopathy. This shows the relationship between ocular hypertension and evolution of systemic hypertensive disease and association with diabetes mellitus.
In this study no increased IOP values could be observed when considering only diabetic patients, which disagrees with the Australian "The Blue Mountains Eye Study" 6. Contrariwise, according to the "Baltimore Eye Survey" 7, there is an association of diabetes mellitus with IOP increase; however, this not very expressive increase is not associated with evolution towards open angle glaucoma.
The results of the "Barbados Eye Study" 8 showed that IOP increase is related to systemic arterial blood pressure, a fact that supports the present study. In addition, that study reports a relationship between IOP increase and diabetes mellitus, a fact that could not be proved in the present study, but supports the "The Blue Mountains Eye Study" and the "Baltimore Eye Survey".
Although there is a tendency of patients with long-standing diabetes to develop diabetic retinopathy and progress to amaurosis, the relationship between IOP increase, glaucoma and diabetes is still a matter of controversy7.
REFERENCES
1. Leske CM, Connel AMS, Wu SY, Hyman LG, Schachat AP. Risk factors for open-angle glaucoma. Arch Ophthalmol 1995;113:918-24.
2. Nicolela, MT. Fluxo sanguíneo ocular em glaucoma: métodos de avaliação e importância. Arq. Bras. Oftalm. 1997;60-6:639-49.
3. Dielemans I, Vingerling JR, Algra D, Hofman A, Grobbee DE, Jong PTVM. Primary open-angle glaucoma, intraocular pressure, and systemic blood pressure in the general elderly population. Ophthalmology 1995;102:54-60.
4. Quigley HA, Enger C, Katz J, Sommer A, Scott R, Gilbert D. Risk factors for the development of glaucomatous visual field loss in ocular hypertension. Arch Ophthalmology 1994;112:644-9.
5. Klein BEK, Klein R, Moss SE. Incidence of self reported glaucoma in people with diabetes mellitus. Br J Ophthalmol 1997;81:743-7.
6. Mitchell P, Smith W, Chey T, Healey PR. Open-angle glaucoma and diabetes. Ophthalmology 1997;104:712-8.
7. Tielsch JM, Katz J, Quigley HA, Javitt JC, Sommer A. Diabetes, intraocular pressure, and primary open-angle glaucoma in the Baltimore eye survey. Ophthalmology 1995;102:48-53.
8. Wu SY, Leske C. Associations with intraocular pressure in the Barbados eye study. Arch Ophthalmol 1997;115:1572-6.
This study was carried out on the basis of data of the Glaucoma Project - University Extension Project - UFPR. The Glaucoma Project has the support of the Rotary Club - Cristo Rei, Allergan-Frumtost Laboratories, town councillor Rui Hara, and Extension and Cultural Sub-Rectory - UFPR.
(1) Responsável pelo
Setor de Glaucoma do Departamento de Oftalmo-Otorrinolaringologia do Hospital
das Clínicas ¾ UFPR.
(2) Residentes do 2º ano de Oftalmologia
do Hospital das Clínicas ¾ UFPR.
(3) Residente do 1º ano de Oftalmologia
Hospital das Clínicas ¾ UFPR.
(4) Acadêmicos do 4º ano do curso
de Medicina ¾ UFPR.
The authors have no proprietary interest in the development of marketing of the instruments or medications referred to in the text.
Address for correspondence: Kenji Sakata. R. Itupava, 1428, Alto da Rua XV. Curitiba (PR) CEP 80040-000. e-mail: [email protected]