

Mário Scheffer1; Jessica Pronestino de Lima Moreira1,2; Lígia Bahia1,3; Sophia Aguiar Monteiro Borges1,4,5; Alex Jones Flores Cassenote1; Gustavo Rosa Gameiro1,6,7; Rubens Belfort Jr7
DOI: 10.5935/0004-2749.2025-0218
ABSTRACT
PURPOSE: This study aimed to evaluate disparities in the distribution of ophthalmologists and the volume of cataract surgeries across Brazil, considering public and private health sectors and the country's federative units.
METHODS: Data on ophthalmologists were obtained from the National Medical Residency Commission and the Associação Múdica Brasileira. Information on cataract surgeries performed through the Unified Health System was collected from the DATASUS database, while data on procedures covered by private health plans were retrieved from the National Supplementary Health Agency. Population estimates from the 2024 Demographic Census of the Brazilian Institute of Geography and Statistics were used to calculate physician density and surgery rates per 100,000 inhabitants. Associations between the number of ophthalmologists and cataract surgery volume were analyzed using Spearman's correlation coefficient.
RESULTS: Brazil has 16,784 ophthalmologists, representing 8.96 specialists per 100,000 inhabitants. Marked disparities were observed: large cities (>500,000 inhabitants) had 18.75 ophthalmologists per 100,000 residents, whereas municipalities with <50,000 inhabitants had fewer than one. Across federative units, physician density ranged from 19.18 per 100,000 in the Federal District to 4.22 in Maranhão. In 2024, cataract surgery rates varied widely, from 1,012.61 per 100,000 inhabitants in the Southeast to 435.00 in the North. Nationally, Unified Health System performed 736.30 surgeries per 100,000 inhabitants, compared with 1,276.79 in the private sector. On average, each ophthalmologist performed 96.92 cataract surgeries annually.
CONCLUSION: Significant inequalities persist in the geographic distribution of ophthalmologists and in cataract surgery provision, with higher surgical volumes concentrated in the private sector. Targeted policies are required to address regional disparities and improve the equity and efficiency of cataract care delivery in Brazil.
Keywords: Ophthalmologists/supply & distribution; Ophthalmologists/statistics & numerical data; Cataract extraction; Health services accessibility/statistics & numerical data; Healthcare disparities; Health policy; Public health systems; Insurance, Heal
INTRODUCTION
Cataract is the leading cause of blindness worldwide, with a prevalence among individuals aged 40 year and older ranging from 11.8% to 18.8%(1). Globally, more than 20 million cataract surgeries are performed annually(2). Beyond visual impairment, cataracts substantially reduce quality of life by limiting mobility and autonomy, while increasing the risks of falls, depression, and social isolation. This burden generates significant social and economic costs for both individuals and healthcare systems(3,4).
Advances in biometry, intraocular lens (IOL) technology, and surgical techniques have resulted in excellent outcomes, with high levels of postoperative visual recovery and patient satisfaction(5). However, surgical accuracy and safety remain critical concerns in several countries(5).
In Brazil, 34.6% of individuals aged 60 year or older have been diagnosed with cataracts in one or both eyes. Nevertheless, considerable regional disparities persist in timely access to surgical treatment(6).
This descriptive and exploratory study aims to identify inequalities in the volume of cataract surgeries and in the availability of ophthalmologists across Brazilian federative units as well as between the public and private health sectors.
METHODS
The volume of cataract surgeries performed in Brazil in 2023 and 2024 was obtained from two official data sources: DATASUS(7), which records procedures within the universal public healthcare system (SUS), and the National Supplementary Health Agency (ANS), which compiles procedures and payments reported by private health insurance operators(8).
Secondary data on ophthalmologists were collected through cross-referencing and analysis of databases from the National Medical Residency Commission/Ministry of Education (CNRM/MEC) and the Brazilian Medical Association (AMB).
To calculate physician and surgery rates per 100,000 inhabitants, population data were derived from the 2024 update of the Demographic Census by the Brazilian Institute of Geography and Statistics (IBGE)(9). Information on the number of health insurance beneficiaries was obtained from the ANS database, using the quarterly average(10). The population denominator for SUS rates was determined by subtracting the number of people with private health insurance from the total population.
Cataract surgery rates per ophthalmologist were also calculated according to the federative units of Brazil.
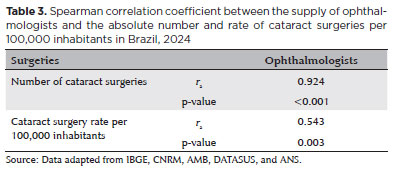
The Spearman correlation coefficient was applied to assess the association between the number of ophthalmologists and the number of cataract surgeries. This was performed in two ways: using the absolute number of surgeries and using surgery rates per 100,000 inhabitants. Statistical analyses were conducted with IBM SPSS software, version 24.0 (Chicago, Illinois), with the significance level set at 5%.
RESULTS
In 2024, there were 16,784 practicing ophthalmologists in Brazil. However, there were 19,054 specialist registrations, as 2,270 individuals (13.5%) were registered with more than one Regional Medical Council and may work in more than one state. The majority of specialists were male (56.3%), with a mean age of 48 years, and 55.9% resided in the country's state capitals.
The distribution of ophthalmologists across Brazil was highly uneven, with 18 federative units below the national average of 8.96 specialists per 100,000 inhabitants (Figure 1). The Federal District had the highest concentration (19.18), followed by São Paulo (11.25) and Espírito Santo (10.97). In contrast, Amazonas (3.60), Pará (3.77), and Maranhão (4.22) recorded the lowest ratios. Among municipalities, the 48 cities with populations of 500,000 or more had 18.75 ophthalmologists per 100,000 inhabitants, while the 3,823 municipalities with fewer than 50,000 residents had fewer than one per 100,000.
At the national level, cataract surgery rates were 779.07 procedures per 100,000 inhabitants in 2023 and 868.69 in 2024 (Tables 1 and 2). In 2024, the SUS accounted for 64% of all cataract surgeries, corresponding to 736.30 procedures per 100,000 inhabitants who relied exclusively on the public system. In 2023, SUS was responsible for 60% of surgeries, with a rate of 607.10 per 100,000 inhabitants. In absolute terms, the public sector performed 984,009 surgeries in 2023 and 1,181,837 in 2024, representing a 20% increase.
In the private sector, among individuals covered by health insurance (approximately one-quarter of the population), the rate was 1,276.79 surgeries per 100,000 insured individuals in 2024, accounting for 36% of the national total. In 2023, private health plans performed 40% of all cataract surgeries, with a rate of 1,340.89 per 100,000 insured individuals. In absolute numbers, the private sector conducted 665,244 surgeries in 2023 and 664,861 in 2024, showing stability with a slight decrease of 0.1%.
In 2024, private health plans performed 73.4% more cataract surgeries per 100,000 inhabitants than SUS, compared with a difference of 121% in 2023. Regional variation was substantial: In 2024, the Southeast registered 1,012.61 surgeries per 100,000 inhabitants, while the North had only 435.04. Across all regions, the private sector performed more procedures than the public sector. The greatest disparities occurred in the North, where private plans performed 157% more surgeries than SUS, and in the South, where the difference was 138%. In the Southeast, Northeast, and Central-West, the differences were 39%, 71%, and 87%, respectively.
When total cataract surgery production (SUS plus private) was considered, the federative units with the lowest rates per 100,000 inhabitants, far below the national average, were Amapá (246.00), Tocantins (256.06), Rondônia (397.31), Acre (404.71), Federal District (413.00), Amazonas (444.36), and Maranhão (452.59; Table 2). The low rate in the Federal District was particularly notable, given that it had the highest concentration of ophthalmologists. In several states, surgical production was concentrated in capital cities, such as Manaus.
In most federative units, surgery rates were higher among those with private health insurance than among SUS users. Exceptions included Amazonas, Roraima, Amapá, Piauí, and Bahia, where the public sector performed more procedures. In Rio de Janeiro, Mato Grosso, and Goiás, surgery rates were similar between the two sectors (Table 2).
The proportion of surgeries performed by SUS relative to the total production varied widely. It exceeded 90% in Acre, Bahia, Piauí, Amapá, Roraima, and Amazonas but fell below 50% in the Federal District and Mato Grosso do Sul. In 2024, surgical productivity per ophthalmologist also varied significantly, ranging from an average of 180.38 procedures per year in Piauí and 147.20 in Alagoas to only 21.54 in the Federal District and 37.06 in Tocantins (Figure 2).
Finally, calculation of the Spearman correlation coefficient (Table 3) revealed a strong correlation between the number of cataract surgeries and the number of ophthalmologists. However, when adjusted for population, this association weakened, suggesting that additional factors may influence surgical output. These likely include professional and behavioral aspects of ophthalmologists as well as structural characteristics of the healthcare system, such as service accessibility, diagnostic capacity, the organization of local and regional care networks, and referral pathways.
DISCUSSION
This study underscores the value of combining secondary data from administrative records on healthcare production and payments generated by SUS managers and private health operators.
As with physicians in general and other medical specialties(11), ophthalmologists are more concentrated in the South and Southeast, a pattern also observed in other Latin American healthcare systems(12).
Although SUS performs the largest absolute number of cataract surgeries, population-adjusted rates show that private health plans provide significantly more procedures. These findings help explain the long waiting times for cataract surgery within SUS(13) and may inform the design of public policies, such as the Agora Tem Especialistas program launched by the federal government in 2025(14).
Over the 2 years analyzed, SUS increased its cataract surgery output, consistent with previous reports(15,16). This growth has been linked to greater federal funding, contracting of private ophthalmology clinics by public administrators, allocation of congressional amendments, and implementation of surgical task forces(15,16).
Access to cataract diagnosis and treatment varies both across and within countries(17,18). With a national rate of 868.7 surgeries per 100,000 inhabitants, Brazil trails behind France (1,493.0)(19), Belgium (1,416.0)(19), Germany (1,153.7)(19), Japan (1,148.0)(20), and the United Kingdom (956.2)(19) but surpasses China (220.5)(21) and Mexico (147.5)(22), where the reported rates may, to some extent, underestimate the actual surgical volume.
Surgical productivity per ophthalmologist varies widely across regions and among professionals. This heterogeneity should be considered when planning specialist training and defining the number of procedures to be offered through SUS.
Further research is warranted to clarify the factors driving these disparities. They may relate to structural issues, such as healthcare financing and system organization, or to patient-level determinants, including income, social conditions, and geographic location. Other potential factors include the availability of ophthalmologists qualified or willing to perform surgeries within SUS and the pricing and reimbursement structures for cataract procedures and intraocular lenses.
Strategies to address these inequities include coordinating initiatives and resources across government levels, reallocating private-sector capacity to public services, standardizing practices and pricing, and engaging ophthalmologists through fair remuneration and adequate working conditions. Cataract surgery could thereby serve as a model case for demonstrating the viability of Brazil's constitutionally mandated universal public healthcare system.
This study has limitations. There are no data on whether ophthalmologists are available to perform surgeries. Surgical records in DATASUS, which rely on reporting from municipal and state health departments, may contain inaccuracies, as may service production data submitted to ANS by private insurance operators. Additionally, procedures paid directly by private patients were not captured.
In conclusion, this study presents new empirical evidence of overlapping geographic and structural inequalities in Brazil, as observed in the supply of ophthalmologists and the volume of cataract surgeries performed across regions, federative units, and healthcare sectors. By delaying timely access to surgical treatment, these disparities force patients to live longer with visual impairment, reducing quality of life and increasing the burden of preventable blindness. Urgent measures are therefore required to overcome inequalities in access to cataract surgery and ophthalmologists in Brazil.
ACKNOWLEDGMENTS
This study was supported by Fundação Faculdade de Medicina (FFM), Secretaria de Gestão do Trabalho e da Educação na Saúde (SGTES) do Ministúrio da Saúde e Organização Pan-Americana da Saúde (OPAS), agreement (OPAS /FFM SCON2023-00159.
AUTHORS' CONTRIBUTIONS:
Significant contribution to conception and design: Mário Scheffer, Jessica Pronestino de Lima Moreira, Lígia Bahia, Sophia Aguiar Monteiro Borges, Alex Jones Flores Cassenote, Gustavo Rosa Gameiro, Rubens Belfort Jr. Data acquisition: Mário Scheffer, Jessica Pronestino de Lima Moreira, Lígia Bahia, Sophia Aguiar Monteiro Borges, Alex Jones Flores Cassenote, Gustavo Rosa Gameiro, Rubens Belfort Jr. Data analysis and interpretation: Mário Scheffer, Jessica Pronestino de Lima Moreira, Lígia Bahia, Sophia Aguiar Monteiro Borges, Alex Jones Flores Cassenote, Gustavo Rosa Gameiro, Rubens Belfort Jr. Manuscript drafting: Mário Scheffer, Jessica Pronestino de Lima Moreira, Lígia Bahia, Sophia Aguiar Monteiro Borges, Alex Jones Flores Cassenote, Gustavo Rosa Gameiro, Rubens Belfort Jr. Significant intellectual content revision of the manuscript: Mário Scheffer, Jessica Pronestino de Lima Moreira, Lígia Bahia, Sophia Aguiar Monteiro Borges, Alex Jones Flores Cassenote, Gustavo Rosa Gameiro, Rubens Belfort Jr. Final approval of the submitted manuscript: Mário Scheffer, Jessica Pronestino de Lima Moreira, Lígia Bahia, Sophia Aguiar Monteiro Borges, Alex Jones Flores Cassenote, Gustavo Rosa Gameiro, Rubens Belfort Jr. Statistical analysis: Mário Scheffer, Jessica Pronestino de Lima Moreira, Lígia Bahia, Sophia Aguiar Monteiro Borges, Alex Jones Flores Cassenote, Gustavo Rosa Gameiro, Rubens Belfort Jr. Obtaining funding: Mario Scheffer. Supervision of administrative, technical, or material support: Mario Scheffer, Rubens Belfort Jr. Research group leadership: Mario Scheffer, Rubens Belfort Jr.
REFERENCES
1. Chen X, Xu J, Chen X, Yao K. Cataract: advances in surgery and whether surgery remains the only treatment in future. Adv Ophthalmol Pract Res. 2021;1(1):100008.
2. Rossi M, Romano MR, Iannetta D, Romano V, Gualdi L, D'Agostino I, et al. Cataract surgery practice patterns worldwide: a survey. BMJ Open Ophthalmol. 2021;6(1):e000464.
3. Marques AP, Ramke J, Cairns J, Butt T, Zhang JH, Muirhead D, et al. Global economic productivity losses from vision impairment and blindness. EClinicalMedicine. 2021;35:100852
4. Burton MJ, Ramke J, Marques AP, Bourne RRA, Congdon N, Jones I, et al. The Lancet Global Health Commission on Global Eye Health: vision beyond 2020. Lancet Glob Health. 2021;9(4):e489-e551.
5. Moore J, McNeely R, Moutari S. Cataract surgery in the small adult eye: a review. Clin Exp Ophthalmol. 2025;53(5):558-69.
6. Instituto Brasileiro de Geografia e Estatística - IBGE. Pesquisa Nacional de Saúde: 2019: ciclos de vida: Brasil [Internet] Rio de Janeiro: IBGE; 2021. 132p. Available from: https://biblioteca.ibge.gov.br/visualizacao/livros/liv101846.pdf
7. Brasil. Ministúrio da Saúde. DATASUS Tecnologia da Informação a serviço do SUS. Produção ambulatorial: (SIA/SUS) [Internet]. Brasília, DF: MS. Available from: https://datasus.saude.gov.br/acesso-a-informacao/producao-ambulatorial-sia-sus/
8. Brasil. Agência Nacional de Saúde Suplementar - ANS. D-TISS-Painel dos dados do TISS [Internet]. Brasília, DF: Ministúrio da Saúde. Available from: https://www.gov.br/ans/pt-br/acesso-a-informacao/perfil-do-setor/dados-e-indicadores-do-setor/d-tiss-painel-dos-dados-do-tiss
9. Instituto Brasileiro de Geografia e Estatística - IBGE. Estimativas da população residente para os municípios e unidades da federação brasileiros com data de referência em 1º de julho de 2024 [Internet]. Rio de Janeiro: IBGE; 2024. Available from: https://www.ibge.gov.br/estatisticas/sociais/populacao/9103-estimativas-de-populacao.html
10. Brasil. Agência Nacional de Saúde Suplementar - ANS. ANS Tabnet: informações em saúde suplementar. Brasília: ANS; atualização trimestral. Available from: https://www.ans.gov.br/anstabnet
11. Scheffer M, coordenador. Demografia Múdica no Brasil 2025. Brasília, DF: Ministúrio da Saúde; Faculdade de Medicina da Universidade de São Paulo; Associação Múdica Brasileira; 2025.
12. Hong H, Mújica OJ, Anaya J, Lansingh VC, López E, Silva JC, et al. The challenge of universal eye health in Latin America: distributive inequality of ophthalmologists in 14 countries. BMJ Open. 2016;6(11):e012819.
13. Teófilo S, Dantas D, Cravo A. Mais procurada do SUS, cirurgia de catarata pode levar em múdia 137 dias para ser realizada. O Globo (Rio de Janeiro) [Internet]. 19 Março 2025. Available from: https://oglobo.globo.com/saude/noticia/2025/03/19/mais-procurada-do-sus-cirurgia-de-catarata-pode-levar-em-media-137-dias-para-ser-realizada.ghtml
14. Brasil. Ministúrio da Saúde. Governo Federal lança o Agora Tem Especialistas para ampliar o atendimento à população e reduzir tempo de espera no SUS [Internet]. Brasília, DF: MS; 2025. Available from: https://www.gov.br/saude/pt-br/assuntos/noticias/2025/maio/governo-federal-lanca-o-agora-tem-especialistas-para-ampliar-o-atendimento-a-populacao-e-reduzir-tempo-de-espera-no-sus
15. Kara-Junior N, Rossi S. Epidemiology of cataract-related blindness in Brazil: 30 years of public policy evolution: a review article. Am J Ophthalmol. 2025;273:205-11.
16. Laboissièrre P. Mutirões oftalmológicos no Brasil causaram complicações em 222 pessoas: dados são do Conselho Brasileiro de Oftalmologia. Agência Brasil (Brasília) [Internet]. 22 Maio 2025. Available from: https://agenciabrasil.ebc.com.br/saude/noticia/2025-05/mutiroes-causaram-complicacoes-e-perda-de-visao-em-222-pessoas-no-pais
17. Kauch CY, Blachley TS, Lichter PR, Lee PP, Stein JD. Geographic variation in the rate and timing of cataract surgery among US communities. JAMA Ophthalmol. 2016;134(3):267-76.
18. Rossi T, Romano MR, Iannetta D, Romano V, Gualdi L, D'Agostino I, et al. Cataract surgery practice patterns worldwide: a survey. BMJ Open Ophthalmol. 2021;6(1):e000464.
19. European Commission. Eurostat. Statistical reports [Internet]. Available from: https://commission.europa.eu/resources/statistics/search-eurostat-statistics_pt
20. Wada S, Miyake M, Hata M, Kido A, Kamei T, Akada M, et al. Annual trends of ophthalmic surgeries in Japan's super-aged society, 2014-2020: a national claims database study. Sci Rep. 2023;13(1):22884.
21. The China study: accessibility and affordability of cataract surgery has improved in China- but there is still more achieve. The Ophthalmologist. [Internet]. 15 set. 2018. Available from: https://theophthalmologist.com/issues/2018/articles/sep/the-china-study
22. Cataract surgical rates. Community Eye Health. 2017;30(100):88-89.
Submitted for publication:
July 30, 2025.
Accepted for publication:
August 26, 2025.
Data Availability Statement: The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request, subject to justified conditions.
Edited by
Editor-in-Chief: Newton Kara-Júnior
Disclosure of potential conflicts of interest: The authors declare no potential conflicts of interest.