

Bo-Een Hwang1,2; Woong-Joo Whang2,3; Young-Hoon Park1,2
DOI: 10.5935/0004-2749.2025-0052
ABSTRACT
PURPOSE: To evaluate whether two simplified modifications of flanged intrascleral fixation techniques (Yamane and Canabrava) provide comparable refractive outcomes and complication rates while reducing surgical complexity in trocar-assisted vitrectomy.
METHODS: This retrospective observational study included 88 patients who underwent flanged fixation surgery with vitrectomy. In the modified Yamane technique, a single-path sclerotomy with bilateral symmetry was performed instead of an angled sclerotomy. In the modified Canabrava technique, the intraocular lens was inserted first, followed by the creation of a circular polypropylene loop with 2-mm flange spacing. Postoperative refractive parameters, including intraocular lens astigmatism, and complications such as intraocular lens iris capture were analyzed.
RESULTS: Of the 88 patients, 70 underwent the modified Yamane technique, and 18 underwent the modified Canabrava technique. No significant differences were observed between the two techniques regarding refractive outcomes or postoperative complications, except for surgical duration, which was significantly shorter (p<0.001) in one technique. Mean intraocular lens astigmatism was −0.675 D for Yamane and −0.666 D for Canabrava.
CONCLUSION: Optimizing needle engagement for symmetry in the Yamane technique and narrowing flange spacing while ensuring a circular polypropylene configuration in the Canabrava technique may reduce surgical complexity and improve postoperative outcomes.
Keywords: Polypropylenes; Yamane technique; Vitrectomy; Astigmatism; Lenses, intraocular; Postoperative complications; Suture techniques; Iris.
INTRODUCTION
Since the introduction of flanged intrascleral fixation by Yamane et al.(1), various modifications have been developed, each aiming to improve specific aspects of the original procedure(2). However, for novice or less experienced retinal surgeons, performing the Yamane technique–which requires creating an angled two-plane sclerotomy and symmetric scleral tunnels–can be challenging. In practice, achieving the recommended scleral tunnel orientation of 20° to the corneal limbus and 10° to the iris surface as described by Yamane(3) is often unrealistic for beginners and generally depends on the intuition of experienced surgeons, particularly in the absence of specialized instruments. During this process, complications such as postoperative intraocular lens (IOL) iris capture or IOL tilt may occur.
Canabrava introduced the four-flanged technique using a four-eyelet foldable IOL, demonstrating potential for enhanced postoperative IOL stability(4,5). Nevertheless, this approach also presents challenges in actual surgical practice. For example, maintaining a flange distance >3-mm can be problematic in retinal surgeries involving trocar insertion, owing to limited space during sclerotomy creation. Furthermore, intraocular manipulation may be hindered when a polypropylene monofilament–already threaded through the IOL eyelet–is introduced into the eye, due to issues such as suture tangling or twisting.
In light of these limitations, the present study introduces two simple and intuitive modifications to flanged intrascleral fixation techniques. The aim is to assess whether, in the context of trocar-assisted vitrectomy, these approaches can reduce surgical complexity while maintaining refractive accuracy and acceptable complication rates.
METHODS
Study population
This retrospective observational study was conducted at the Department of Ophthalmology and Visual Science, Seoul St. Mary's Hospital, in accordance with the principles of the Declaration of Helsinki. The study protocol was approved by the Institutional Review Board (IRB) of Seoul St. Mary's Hospital, The Catholic University of Korea (KC24RISI0420). Given its retrospective design and use of anonymized data, the requirement for written informed consent was waived, as per IRB guidelines.
Eighty-eight patients who underwent suture-less flanged intrascleral fixation surgery with vitrectomy, performed by a single surgeon (B.E. Hwang), between June 2022 and 2024 at Seoul St. Mary's Hospital, were included. Medical records were reviewed retrospectively, and all patients were followed up for at least 3 months postoperatively, undergoing comprehensive ophthalmic examinations.
Exclusion criteria were axial length >32 or <22-mm, history of refractive surgery, and presence of other corneal or retinal diseases that could confound refraction or keratometry measurements.
Surgical technique
Modified Yamane technique
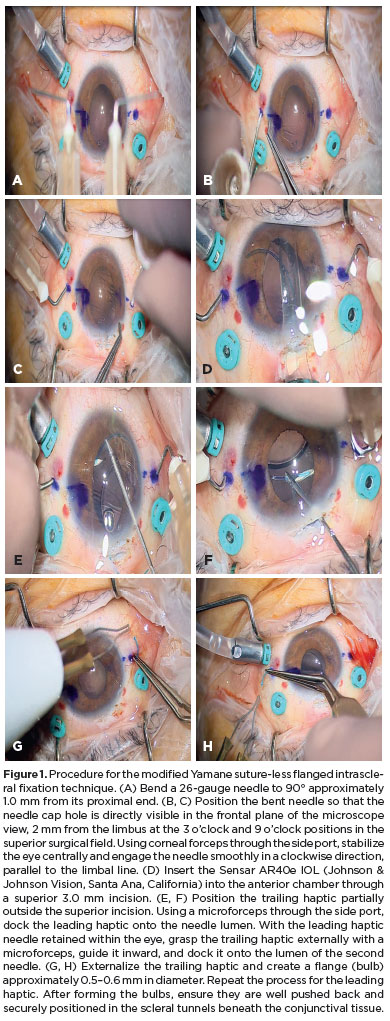
A 26-gauge needle was bent to 90° approximately 1.0-mm from its proximal end. Corneal side ports (1-mm) were created at the 2 o'clock and 10 o'clock positions. The bent needle was positioned so that the needle cap hole was directly visible in the microscope's frontal view, 2-mm from the limbus at the 3 o'clock and 9 o'clock positions in the superior surgical field. Using corneal forceps through the side port, the eye was stabilized centrally, and the needle was engaged smoothly in a clockwise direction, parallel to the limbal line.
Following needle insertion, a Sensar AR40e IOL (Johnson & Johnson Vision, Santa Ana, California) was inserted into the anterior chamber through a superior 3.0-mm incision, leaving the trailing haptic partially outside the incision. Using a microforceps through the side port, the leading haptic was docked into the needle lumen. With the leading haptic retained within the eye, the trailing haptic was grasped externally using a microforceps, guided inward, and docked into the lumen of the second needle. The trailing haptic was then externalized and cauterized approximately 1.5–2-mm from its tip to create a flange measuring about 0.5–0.6-mm in diameter(6)–roughly three times the IOL haptic size. The same procedure was repeated for the leading haptic. Both flanges were then pushed back securely into the scleral tunnels beneath the conjunctival tissue (Figure 1 and Video 1).
Modified Canabrava technique
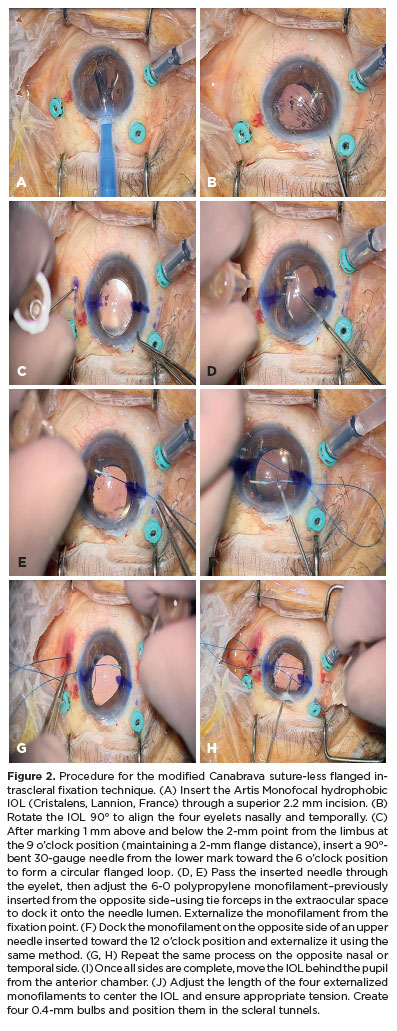
An Artis Monofocal hydrophobic IOL (Cristalens, Lannion, France) was inserted through a superior 2.2-mm incision and rotated 90° to align the four eyelets nasally and temporally. Both ends of a 6-0 polypropylene monofilament were cut diagonally to a length of 7 cm. The monofilament was partially inserted through a corneal side port created at the 3 o'clock position. After marking 1-mm above and below the 2-mm point from the limbus at 9 o'clock (maintaining 2-mm flange spacing), a 90°-bent 30-gauge needle was inserted from the lower mark toward the 6 o'clock position to form a circular flanged loop.
The needle was passed through the IOL eyelet, and the monofilament–previously inserted from the opposite side–was docked into the needle lumen using tie forceps in the extraocular space. With microforceps through the superior incision, the monofilament was firmly docked and externalized. The same steps were repeated for the opposite side (toward 12 o'clock) and the remaining nasal or temporal side.
Once all four sides were complete, the IOL was moved behind the pupil from the anterior chamber. The lengths of the four externalized monofilaments were adjusted to center the IOL and maintain appropriate tension. Each externalized end was cauterized to create a 0.4-mm flange and placed into the scleral tunnels(6) (Figure 2 and Video 2).
Study protocol
Comprehensive postoperative examinations were performed to identify complications related to scleral fixation, including IOL iris capture, flange extrusion, vitreous hemorrhage, changes in intraocular pressure (IOP), cystoid macular edema, and endophthalmitis.
Intraocular pressure astigmatism was calculated by subtracting corneal astigmatism from total astigmatism, considering whether both were aligned on the same axis or different axes. IOL power was determined preoperatively using the third-generation Holladay 1 formula, targeting emmetropia. The difference between the postoperative spherical equivalent refraction and the target diopter was recorded. Additional measurements included axial length and corneal diameter (white-to-white) to assess factors potentially influencing postoperative IOL refraction.
Statistical analysis
All statistical analyses were performed using SPSS for Windows, version 24.0 (SPSS, Inc., Chicago, Illinois). Independent t tests were used to compare continuous variables between the modified Yamane and Canabrava Groups, and two-sided Fisher's exact tests were used for categorical variables. A p-value <0.05 was considered statistically significant.
RESULTS
Demographic characteristics, refractive measurements, and postoperative complications are summarized in table 1. Of the 88 patients included, 70 underwent the modified Yamane technique, and 18 underwent the modified Canabrava technique.
There were no statistically significant differences between the two groups in refractive outcomes or postoperative complications, except for surgical duration, which was significantly different between techniques (p<0.001).
Mean IOL astigmatism was −0.675 D in the Yamane Group and −0.666 D in the Canabrava Group. The mean difference between the target spherical equivalent and postoperative spherical equivalent was −0.266 D for Yamane and −0.261 D for Canabrava.
In the Yamane Group, IOL iris capture occurred in four cases (5.7%), and flange extrusion beneath the conjunctival tissue was observed in two cases (2.9%).
DISCUSSION
In the modified Yamane technique, the primary challenge lies in controlling the length and symmetry of the scleral tunnels(2) (Figure 3A–3C). Our approach involves marking 2-mm from the limbus and directly engaging the needle at this point. When a trocar is in place, a shortened tunnel length is preferred to minimize spatial constraints, using a single-path insertion method. The needle, pre-bent at 90°, is engaged to ensure maximal symmetry by orienting the needle opening directly toward the microscope's frontal plane.
Intraocular lens iris capture, one of the most common postoperative complications of the Yamane technique, occurred in 5.7% of cases in our series–slightly lower than the 8% rate reported by Yamane(1). This finding suggests that shorter tunnels with optimized symmetry do not increase the risk of IOL tilt or dislocation.
The modified Canabrava technique differs in that the IOL is inserted before the polypropylene monofilament is passed through the eyelets, preventing twisting or tangling and reducing surgical time. Using a 30-gauge needle, we pass a 6-0 polypropylene monofilament through the IOL in an inverted U shape, maintaining a flange distance of 2-mm in a circular loop configuration to optimize the position of the bulb and polypropylene (Figure 3D–3F).
Furthermore, achieving bilateral symmetry in the Yamane modification and ensuring a circular-loop configuration in the Canabrava modification, combined with optimal bulb sizing, helped minimize flange extrusion rates (Figure 4).
In summary, modifications to both the Yamane and Canabrava techniques simplified surgical steps during trocar-assisted vitrectomy and yielded favorable refractive accuracy and complication rates. These findings confirm that the techniques maintain clinical safety while improving surgical efficiency. In the Yamane technique, focusing on precise needle engagement for bilateral symmetry–rather than creating longer, angled scleral tunnels–can produce favorable postoperative outcomes. In the Canabrava technique, reducing flange spacing and ensuring the polypropylene forms a true circle can prevent bulb exposure, while inserting and then fixating the IOL can avoid monofilament twisting and shorten surgical duration.
ACKNOWLEDGMENTS
This study was supported by the Basic Science Research Program through the National Research Foundation of Korea (RS-2023-00253065).
AUTHORS' CONTRIBUTIONS:
Significant contribution to conception and design: Bo-Een Hwang, Woong-Joo Whang, Young-Hoon Park. Data Acquisition: Bo-Een Hwang. Data Analysis and Interpretation: Bo-Een Hwang. Manuscript Drafting: Bo-Een Hwang. Significant intellectual content revision of the manuscript: Young-Hoon Park. Final approval of the submitted manuscript: Bo-Een Hwang, Woong-Joo Whang, Young-Hoon Park. Statistical analysis: Bo-Een Hwang. Obtaining funding: Young-Hoon Park. Supervision of administrative, technical, or material support: Woong-Joo Whang. Research group leadership: Young-Hoon Park.
REFERENCES
1. Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology. 2017;124(8):1136-42.
2. Yamane S, Ito A. Flanged fixation: Yamane technique and its application. Curr Opin Ophthalmol. 2021;32(1):19-24.
3. Yamane S, Maruyama-Inoue M, Kadonosono K. Needle stabilizer for flanged intraocular lens fixation. Retina. 2019;39(4):801.
4. Canabrava S, Andrade N, Jr., Henriques PR. Scleral fixation of a 4-eyelet foldable intraocular lens in patients with aphakia using a 4-flanged technique. J Cataract Refract Surg. 2021;47(2):265-9.
5. Canabrava S, Carvalho MS. Double-flanged polypropylene technique: 5-year results. J Cataract Refract Surg. 2023;49(6):565-70.
6. Kronschlager M, Blouin S, Ruiss M, Findl O. Attaining optimal flange size with 5-0 and 6-0 polypropylene sutures for scleral fixation. J Cataract Refract Surg. 2022;48(11):1342-5.
Submitted for publication:
February 6, 2025.
Accepted for publication:
July 25, 2025.
Approved by the following research ethics committee: Seoul St. Mary's Hospital, The Catholic University of Korea (KC24RISI0420).
Data Availability Statement: The datasets generated and/or analyzed during the current study are included in the manuscript.
Edited by
Editor-in-Chief: Newton Kara-Júnior
Associate Editor: Richard Y. Hida
Disclosure of potential conflicts of interest: The authors declare no potential conflicts of interest.