

Ersan Ersin Demirel1; Emrah Ozturk2; Abuzer Gunduz3
DOI: 10.5935/0004-2749.2025-0045
ABSTRACT
PURPOSE: To evaluate the effect of using a single iris retractor, affixed to the anterior capsulorhexis at the 12 o'clock position, on the ease of capsular tension ring implantation.
METHODS: This prospective comparative study comprised 37 patients with zonular weakness attributed to pseudoexfoliation syndrome who underwent capsular tension ring implantation during cataract surgery. In Group 1, a single iris retractor was inserted into the anterior capsulorhexis at the 12 o'clock position. Group 2 did not receive this intervention. Zonular weakness was graded on a scale of 1–5, and the subjective difficulty of capsular tension ring implantation was categorized as easy, medium, or difficult.
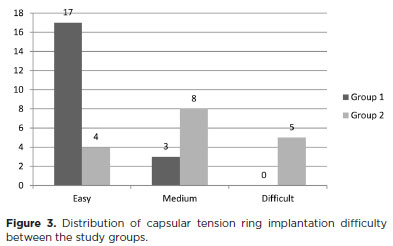
RESULTS: Group 1 and 2 comprised 20 and 17 patients, respectively. There were no significant differences between the groups in age, sex distribution, and presence of glaucoma (p=0.53, p=0.28, and p=1.00, respectively). The mean zonular weakness score was significantly higher in Group 1 (3.35 ± 0.45) than in Group 2 (2.71 ± 0.59; p=0.02). Capsular tension ring implantation was significantly easier in the iris retractor group (p<0.001).
CONCLUSIONS: Placement of a single iris retractor attached to the anterior capsulorhexis at the 12 o'clock position may facilitate easier capsular tension ring implantation, even in patients with greater zonular weakness. This technique could reduce the risk of capsular tension ring displacement into the iridocorneal angle or ciliary sulcus.
Keywords: Capsular tension ring; Cataract; Iris hook; Pseudoexfoliation syndrome; Zonular weakness; Cataract extraction; Phacoemulsification; Capsulorhexis.
INTRODUCTION
Zonulopathy is a significant risk factor for complications during cataract surgery. Common causes include pseudoexfoliation syndrome, degenerative myopia, ocular trauma, and iatrogenic zonular injury(1). Management strategies for zonulopathy involve minimizing lens manipulation and rotation and the use of surgical instruments such as capsular hooks, capsular tension rings (CTRs), and capsular tension segments(2).
The CTR is widely used in cataract surgery for patients with zonulopathy to improve surgical outcomes and reduce complications. It supports areas of zonular laxity and helps maintain the integrity of the capsular bag. Capsular hooks are another tool used to stabilize the capsule during phacoemulsification in cases of zonular instability. Unlike iris hooks, which support the capsule through a looped design, capsular hooks distribute force over a broader area, reducing the risk of anterior capsule tears(2). However, iris hooks are often used in clinical practice when capsular hooks are unavailable(3,4).
Several techniques have been described for CTR insertion. Common approaches include the use of an injector or a freehand bimanual technique, which guides the leading eyelet into the capsular bag(1). In both methods, the posterior end is advanced, the anterior end is maneuvered around the capsular bag, and finally, the posterior end is released beneath the capsulorhexis. The ideal CTR insertion technique should be easy to perform and should avoid additional zonular damage. Consequently, variations such as the fishtail, modified fishtail, and suture-guided techniques have been reported(1,5-7). Additionally, capsular or iris hooks can be used during CTR implantation, similar to their role in phacoemulsification(8).
In this study, we placed a single iris retractor at the 12 o'clock position on the anterior capsulorhexis edge before CTR insertion. The aim was to evaluate the effect of using a single iris hook on the ease of CTR implantation.
METHODS
This prospective, comparative, single-center study included 37 eyes with cataracts associated with pseudoexfoliation syndrome that underwent phacoemulsification surgery, posterior chamber intraocular lens (IOL) implantation, and CTR insertion between January 2020 and July 2021. The study was conducted at the Department of Ophthalmology, Malatya Training and Research Hospital, a tertiary care facility in Malatya, Turkey. Written informed consent was obtained from all participants prior to surgery, and all procedures adhered to the principles of the Declaration of Helsinki. The study protocol was approved by the Inonu University Malatya Clinical Research Ethics Committee (Reference number: 2020/116).
Patients with pseudoexfoliation syndrome and sufficient pupil dilation for phacoemulsification, achieved through medical treatment, were included. All patients underwent comprehensive ocular evaluation, including best-corrected visual acuity (BCVA) assessment using Snellen charts, anterior and posterior segment examination, and intraocular pressure (IOP) measurement. In cases where cataract-related media opacity prevented fundus assessment via ophthalmoscopy, B-scan ocular ultrasonography was performed.
Exclusion criteria included significant zonulysis, lens subluxation, prior ocular surgery or laser treatment, history of ocular trauma or disorders (except glaucoma), and any intraoperative compromise of capsular integrity prior to CTR implantation. Recorded variables included age, sex, operated eye, preoperative BCVA and IOP, presence of mature cataract and glaucoma, degree of zonular weakness, difficulty of CTR implantation, and intraoperative complications.
All patients had varying degrees of zonular weakness, which were subjectively graded by a surgeon on a scale from 1 to 5. The first 20 patients (Group 1) received a single iris retractor at the 12 o'clock position on the anterior capsulorhexis during CTR implantation. The subsequent 17 patients (Group 2) underwent CTR implantation without an iris retractor. The same surgeon graded the difficulty of CTR implantation as easy, medium, or difficult. "Easy" was defined as uneventful CTR implantation in a single attempt; "difficult" was defined as migration of the posterior CTR end into the iridocorneal angle or ciliary sulcus or an observable increase in the zonular defect; and the remaining cases were classified as "medium".
All surgeries were performed by a single experienced surgeon (A.G.) under local or general anesthesia. Corneal incision site and iris hook placement were determined based on the surgeon's right-handed preference. A 2.4-mm corneal phaco incision was made at the 10 o'clock position. A 5.5-mm continuous curvilinear capsulorhexis was created, followed by multi-quadrant cortical split hydrodissection. Nucleus removal was performed using the phaco quick-chop technique.
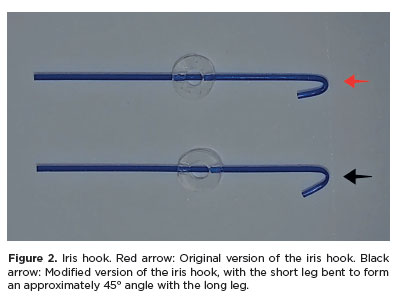
Late CTR implantation was performed in all cases after complete removal of the nucleus and cortex. The capsular bag was filled with 1.4% sodium hyaluronate (CrownVisc 1.4%, Miray Medikal, Bursa, Turkey) and the CTR was inserted. Prior to CTR implantation, it was essential for the capsular bag to be tense and devoid of folds. In Group 1, a single iris retractor (Ovation International, India) was positioned at the 12 o'clock edge of the anterior capsulorhexis before CTR implantation (Figure 1). Before the insertion, the short distal end of the retractor was bent at a 45° angle relative to the longer proximal segment to reduce the risk of anterior capsule tear (Figure 2). A polymethyl methacrylate CTR type 4 (13–11 mm; Madhu Instruments, New Delhi, India) was implanted into the capsular bag using a freehand bimanual technique. The trailing eyelet was positioned easily by elevating the capsule against the undersurface of the attached iris retractor. Subsequently, a single-piece foldable acrylic posterior chamber IOL was inserted into the capsular bag.
Statistical analysis
Data were analyzed using SPSS for Windows (version 22.0; IBM Corp., Armonk, New York). Descriptive statistical data for categorical variables were expressed as numbers, and statistical data for continuous variables were reported as mean ± standard deviation or median (min–max). Normality of distribution was assessed using the Shapiro–Wilk test. The t-test and Mann–Whitney U test were used for between-group comparisons of quantitative variables, and chi-square tests were used for qualitative data to investigate differences between the two groups. P-value less than or equal to 0.05 was considered statistically significant.
RESULTS
A total of 37 patients were included in the study, 20 in Group 1 and 17 in Group 2. Women comprised 35.0% of Group 1 and 17.6% of Group 2. The mean age was 70.8 ± 9.0 and 72.5 ± 8.6 years in Group 1 and 2, respectively. There were no statistically significant differences between the groups in terms of gender, age, operated eye, preoperative BCVA, IOP, presence of mature cataract, and glaucoma (Table 1).
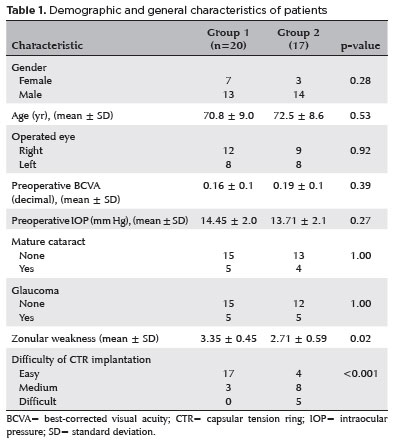
The mean degree of zonular weakness score was significantly higher in Group 1 (3.35 ± 0.45) than in Group 2 (2.71 ± 0.59; p=0.02). The difficulty of CTR implantation also differed significantly between the groups, with implantation rated as easier in the iris retractor group (p<0.001; Figure 3). In Group 2, "difficult" rating was assigned to five patients, whereas none in Group 1 received this rating. In these five cases, the posterior end of the CTR migrated into the iridocorneal angle or ciliary sulcus, complicating the procedure. Significant complications such as capsular rupture or CTR dislocation did not occurred during CTR implantation in both group. However, capsular rupture occurred during phacoemulsification in two patients initially scheduled for CTR implantation. Consequently, CTRs were not implanted in these cases, and they were excluded from the study.
DISCUSSION
CTRs implantation can present various challenges and complications. Traditional methods typically employ an injector or a freehand bimanual technique to guide the leading eyelet into the capsular bag. The torque generated where the CTR connects with the capsular bag may exacerbate zonular stress, potentially leading to extended or iatrogenic zonular dialysis(9). Using Miyake–Apple analysis, Ahmet et al. reported capsular bag displacement of 0.5–4.0 mm during CTR insertion(10), underscoring the risk of additional zonular stress.
Several techniques have been proposed to minimize the risk of additional zonular damage and prevent complications during CTR implantation, including the fishtail, modified fishtail, and suture-guided techniques(1,5–7). The fishtail technique involves bending the CTR in half and inserting the apex through the corneal incision to minimize rotation and capsular bag displacement(5); however, the excessive bending required can damage the CTR. Rixen et al. addressed this limitation with the fishtail on a line technique(1), which uses a suture in the leading eyelet. However, both techniques limit direct control over the leading eyelet, and the fishtail on a line requires an inserter. The suture-guided CTR technique improves control by passing a suture through the leading eyelet using microforceps, reducing torque and entanglement during implantation(7). However, this technique requires an inserter and a secondary microsurgical instrument. Cendelin et al. modified this technique by adding a loop to the suture and using a hook instead of microforceps, allowing simultaneous cortical cleanup during early CTR insertion(6).
The technique used in our study does not require microforceps, injectors, or sutures, making it a cost-effective alternative for clinics with limited resources. Additionally, it avoids excessive CTR bending, eliminating the risk of fracture.
Capsular hooks are valuable in stabilizing the capsular bag during lens aspiration and CTR implantation(8). They provide countertraction and prevent bag rotation(8). In the fishtail technique, Angunawela et al. highlighted the benefit of supplementary capsule hooks in stabilizing the bag and providing additional protection to the residual zonules(5). However, concurrent use of capsular hooks and CTRs can be problematic if the CTR navigate through the distal loop of the hook(11). In our study, we used an iris retractor instead of a capsular hook to achieve similar stabilization. Both devices can extend the capsulorhexis margin and provide anterior–posterior support to the zonular–lens complex in cases of zonular weakness(12).
We modified the freehand bimanual technique by placing an iris retractor at the 12 o'clock position of the anterior capsulorhexis before CTR insertion, evaluating its effect on CTR implantation. This modification make implantation significantly easier than the traditional approach (p<0.001). As the degree of zonular weakness increases, CTR implantation becomes more susceptible to complications. In Group 1, the degree of zonular weakness was significantly high (p=0.02). Our technique facilitated easy CTR implantation, even in Group 1, who were more disadvantaged for CTR implantation than Group 2.
Our approach presents several advantages. First, it may reduce the risk of iatrogenic damage to the iris root, capsule, and zonules by preventing CTR displacement into the iridocorneal angle or ciliary sulcus. Second, by supporting the upper zonules, it potentially limits additional zonular damage by balancing the inferior force generated by the anterior end of the CTR during rotation within the capsular bag. Third, by fixing the anterior capsulorhexis and iris margin in relative proximity, it potentially limits zonular damage resulting from rotational forces during implantation. However, the short distal end of an iris retractor does not reach the equatorial capsular bag(11), limiting support to the upper zonules.
In our protocol, to implant the CTR into the capsular bag in both eyes, the phaco incision was placed at 10 o'clock, and the CTR was rotated clockwise. The iris retractor was placed at 12 o'clock to counterbalance the force exerted on the opposite side of the incision during CTR implantation using the freehand bimanual technique. This placement also prevented trailing eyelet of the CTR, which is implanted through the corneal phaco incision at 10 o'clock position and rotated clockwise, from dislocating into the iridocorneal angle or ciliary sulcus. The position of the single iris retractor can be adapted depending on the incision site and rotation direction during CTR implantation.
The reported incidence of cataract surgery complications in pseudoexfoliation syndrome ranges from 1% to 25%(13,14), and CTR use can reduce this rate. In our study, capsular rupture occurred in two patients (5.4%) during phacoemulsification, who were scheduled for CTR implantation. However, no significant complications occurred during CTR implantation in both group.
Limitations of this study include the small sample size. Studies with larger sample size could provide a more comprehensive understanding of the outcomes associated with CTR implantation. Additionally, the grading of zonular weakness and implantation difficulty was subjective, which may have introduced bias. To reduce variability, all surgeries and assessments were performed by a single surgeon.
In conclusion, we describe a simple, safe, and effective modification of the freehand bimanual technique for CTR implantation. This modification significantly reduces stress on already compromised zonules compared with traditional methods. Positioning a single iris retractor at the 12 o'clock location of the anterior capsulorhexis before CTR insertion significantly simplifies the implantation procedure, helps prevent CTR displacement into the iridocorneal angle and ciliary sulcus, and may reduce radial and circumferential zonular stress compared with the freehand bimanual technique.
AUTHORS' CONTRIBUTIONS:
Significant contribution to conception and design: Abuzer Gunduz. Data Acquisition: Ersan Ersin Demirel, Abuzer Gunduz. Data Analysis and Interpretation: Emrah Öztürk. Manuscript Drafting: Ersan Ersin Demirel. Significant intellectual content revision of the manuscript: Abuzer Gunduz. Final approval of the submitted manuscript: Ersan Ersin Demirel, Emrah Ozturk, and Abuzer Gunduz. Statistical analysis: Emrah Ozturk. Obtaining funding: not applicable. Supervision of Administrative, Technical, or Material Support: Emrah Ozturk, Abuzer Gunduz. Research group Leadership: Abuzer Gunduz.
REFERENCES
1. Rixen JJ, Oetting TA. Fishtail on a line technique for capsular tension ring insertion. J Cataract Refract Surg. 2014;40(7):1068-70.
2. Finklea B. Zonulopathy: evaluation and surgical management. EyeWiki [Internet]. [cited 2025 May 24]. Available from: https://eyewiki.aao.org/Zonulopathy:_Evaluation_and_Surgical_Management.
3. Merriam JC, Zheng L. Iris hooks for phacoemulsification of the subluxated lens. J Cataract Refract Surg. 1997;23(9):1295-7.
4. Ozturk E, Gunduz A. Optimal timing of capsular tension ring implantation in pseudoexfoliation syndrome. Arq Bras Oftalmol. 2021;84(2):158-62.
5. Angunawela RI, Little B. Fish-tail technique for capsular tension ring insertion. J Cataract Refract Surg. 2007;33(5):767-9.Comment in: J Cataract Refract Surg. 2007;33(11):1840.
6. Cendelin J, Rusnak S. Loop-on-suture-guided insertion for easier capsular tension ring insertion and residual cortex removal. J Cataract Refract Surg. 2020;46(11):1561-3.
7. Page TP. Suture-guided capsular tension ring insertion to reduce risk for iatrogenic zonular damage. J Cataract Refract Surg. 2015;41(8):1564-7.
8. Khokhar S, Gupta S, Nayak B, Gogia V. Capsular hook-assisted implantation of modified capsular tension ring. BMJ Case Rep. 2016;2016:bcr2015214274.
9. Jacob S, Agarwal A, Agarwal A, Agarwal S, Patel N, Lal V. Efficacy of a capsular tension ring for phacoemulsification in eyes with zonular dialysis. J Cataract Refract Surg. 2003;29(2):315-21.
10. Ahmed II, Cionni RJ, Kranemann C, Crandall AS. Optimal timing of capsular tension ring implantation: Miyake-Apple video analysis. J Cataract Refract Surg. 2005;31(9):1809-13.
11. Grove K, Condon G, Erny BC, Chang DF, Kim T. Complication from combined use of capsule retractors and capsular tension rings in zonular dehiscence. J Cataract Refract Surg. 2015;41(11):2576-9.
12. Yaguchi S, Yaguchi S, Bissen-Miyajima H. Evaluation of lens capsule stability using capsular tension ring, iris retractor, and capsule expander using a porcine model with zonular dehiscence. Invest Ophthal Vis Sci. 2019;60(10):3507-13.
13. Moreno J, Duch S, Lajara J. Pseudoexfoliation syndrome: clinical factors related to capsular rupture in cataract surgery. Acta Ophthalmol (Copenh). 1993;71(2):181-4.
14. Drolsum L, Haaskjold E, Sandvig K. Phacoemulsification in eyes with pseudoexfoliation. J Cataract Refract Surg. 1998;24(6):787-92.
Submitted for publication:
February 19, 2025.
Accepted for publication:
July 25, 2025.
Approved by the following research ethics committee: Inonu University Malatya (# 2020/116).
Data Availability Statement: The datasets generated and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Edited by
Editor-in-Chief: Newton Kara-Júnior
Associate Editor: Camila Koch
Funding: This study received no specific financial support.
Disclosure of Potential Conflicts of Interest: The authors declare no potential conflicts of interest.