

Tiago Santos Prata1,2,3; Isabella Cristina Tristão Pinto Resende4; Daniela Mauricio Ribeiro2; Fábio Nishimura Kanadani1,2,3; Izabela Negrão Frota de Almeida1,2,5
DOI: 10.5935/0004-2749.2025-0020
ABSTRACT
Angle-closure glaucoma is a major cause of visual impairment worldwide, with Plateau iris syndrome presenting management challenges. We present a case report of a 58-year-old woman with advanced, uncontrolled angle-closure glaucoma and Plateau iris. Her history included laser peripheral iridotomy and three glaucoma medications in both eyes. Different treatments were implemented. For the eye with lower intraocular pressure, fewer peripheral anterior synechiae, and milder disease: phacoemulsification with intraocular lens implantation. For the eye with more advanced disease, a two-step approach was used: slow-coagulation transscleral cyclophotocoagulation using the double-arc protocol, followed by phacoemulsification with intraocular lens implantation 2 months later. Both eyes achieved improved visual acuity and intraocular pressure control with fewer medications, without significant complications. This case highlights transscleral cyclophotocoagulation followed by phacoemulsification as an alternative to combined surgeries in uncontrolled angle-closure glaucoma with Plateau iris, offering a simpler technique, more predictable refractive and pressure-control outcomes, and more straightforward postoperative management.
Keywords: Glaucoma, angle-closure/surgery; Iris diseases/surgery; Laser coagulation/methods; Phacoemulsification; Lens implantation, intraocular; Case reports
INTRODUCTION
Angle-closure glaucoma (ACG) is a major cause of visual impairment worldwide. It is characterized by elevated intraocular pressure (IOP) due to impaired drainage of aqueous humor, often resulting from anatomic abnormalities that block the trabecular meshwork. Plateau iris syndrome presents unique management challenges among the forms of ACG due to its distinct anatomical configuration(1).
Regarding treatment, laser peripheral iridotomy (LPI), the first-line therapy, is insufficient if there is persistent IOP elevation or extensive peripheral anterior synechiae (PAS)(1). Phacoemulsification also deepens the anterior chamber (AC) and widens the angle, relieving IOP(2). However, in more advanced disease or anatomical challenges, it may not adequately control IOP, requiring combined or sequential interventions(3).
Traditionally, combined phacoemulsification and trabeculectomy are used in advanced cases but carry a higher risk of complications, particularly in eyes with Plateau iris(3). An alternative is a two-step strategy using transscleral cyclophotocoagulation (TSCPC) with the double-arc slow-coagulation TSCPC protocol (DA-TSCPC), followed by phacoemulsification. This approach may be safe and effective for complex cases(4).
A PubMed literature review on September 16, 2024, using the keywords “Transscleral Cyclophotocoagulation” and “Plateau iris”, identified one successful case of ACG and Plateau iris treated with combined phacoemulsification, goniotomy, and TSCPC(5). No reports of DA-TSCPC followed by phacoemulsification were found. This case presents a strategy for managing uncontrolled ACG and Plateau iris configuration, offering insights into the benefits and considerations of a staged surgical approach.
CASE REPORT
A healthy 58-year-old White female was referred due to uncontrolled ACG, on three glaucoma medications (brinzolamide plus timolol maleate, and latanoprost in both eyes – OU), treated for 9 years. Her ocular history included only laser peripheral iridotomy (LPI) in OU.
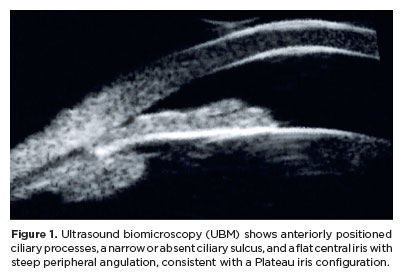
Best-corrected visual acuity (BCVA) was 20/25 in OU, with mild hyperopia (+1.50 -0.75 × 135 in the right eye – OD; +1.25 -0.50 × 160 in the left eye – OS). IOP was 25 mmHg in OD and 17 mmHg in OS. Biomicroscopy revealed mild cataracts, a shallow peripheral anterior chamber (AC), and a relatively deep central AC in OU. Gonioscopy showed occludable angles with the double hump sign during indentation, extensive peripheral anterior synechiae (PAS) in OD, and appositional angle closure with localized PAS in OS. Fundus examination showed enlarged disc cupping, more pronounced in OD (cup-to-disc ratio of 0.85 OD and 0.7 OS), with neuroretinal rim thinning confirmed by structural and functional tests (Mean Deviation: -11.82 and -4.11, OD and OS, respectively). Ultrasound biomicroscopy revealed a Plateau iris configuration in OU (Figure 1).
Given the findings, different approaches were used for each eye. For OS, which had lower IOP and fewer PAS, phacoemulsification with intraocular lens (IOL) implantation was performed. For OD, which had higher IOP, extensive PAS, and more advanced disease, a two-step approach was used: DA-TSCPC(4) followed by phacoemulsification with IOL implantation 2 months later.
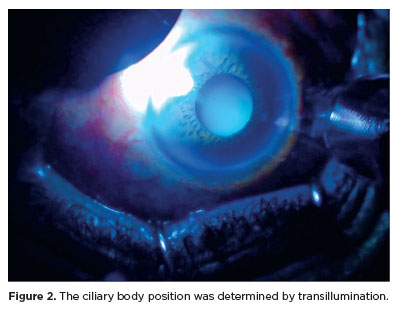
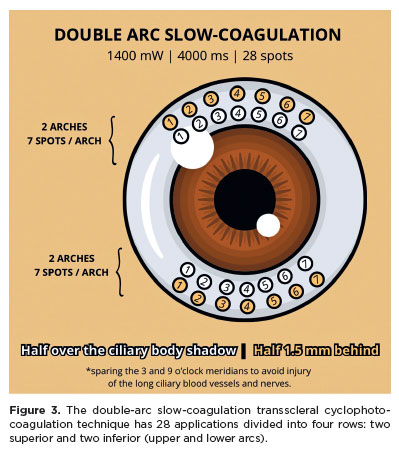
DA-TSCPC was performed under peribulbar anesthesia using a transillumination microscope (Figure 2) and a conventional 810 nm diode laser with a laser probe (Lightmed Corporation, San Clemente, CA, USA). The settings were 1400 mW and 4000 ms. A total of 28 applications were applied in four rows: upper and lower arcs (Figure 3). For each arc, 7 spots were placed over the ciliary body shadow (perilimbal dark band) and 7 spots 1.5 mm behind, sparing the 3 and 9 o’clock meridians. No “POP sound” indicative of ciliary body explosion was heard. The patient was prescribed 0.1% nepafenac 4 times/day for 15 days and 1% prednisolone acetate 4 times/day, tapered by removing one dose each week.
Six weeks after surgery in OS, IOP was 14 mmHg with two topical medications. Six weeks after DA-TSCPC in OD, IOP was 13 mmHg with three topical medications. Following phacoemulsification in OD, one medication was discontinued. After six months, BCVA was 20/20 in OU (refraction: +0.50 -0.50 × 145 and +0.25 -0.50 × 150, OD and OS, respectively), and medications remained unchanged (brinzolamide plus timolol maleate in OU), with IOP at 14 and 12 mmHg. No significant postoperative pupillary diameter changes were observed in OU.
DISCUSSION
This case highlights the complexity of managing ACG, particularly in eyes with Plateau iris. Although many cases can be managed with phacoemulsification(2), eyes with uncontrolled IOP and advanced damage often require a combined procedure, such as phacoemulsification and trabeculectomy(3).
However, combined procedures can be challenging, especially in the presence of Plateau iris, a risk factor for postoperative malignant glaucoma(6). This underscores the need to explore surgical techniques that improve patient safety in such cases.
In this case, a two-step approach was used for OD instead of the conventional combined procedure. We believe this strategy offers advantages, particularly in eyes with good visual potential(4). Dividing the treatment simplifies each step, reduces aggressiveness, improves postoperative inflammation control, and potentially lowers the risk of complications associated with combined phacoemulsification and cyclophotocoagulation (CPC). It also allows for more straightforward postoperative management(7).
Additionally, performing CPC before cataract surgery enhances predictability in pressure control, which enables more precise surgical planning(4). It also offers flexibility to repeat CPC or adjust the technique if the initial outcome is suboptimal(8). However, this approach requires two visits to the surgical center under anesthesia.
Diode laser TSCPC has been successfully used to treat chronic ACG, with a one-year success rate over 80%(9). In this case, it eliminated the need for a filtering procedure and reduced the risk of ocular decompression in OD. Evidence also suggests that laser application to the ciliary body may deepen the AC, potentially making phacoemulsification easier and refractive outcomes more predictable(10).
While potential complications of TSCPC include prolonged inflammation and hypotony, our one-year safety profile of DA-TSCPC showed that complications were infrequent and transient, especially in eyes with better visual prognosis(4).
In summary, this case demonstrates the potential of TSCPC as a preparatory step before phacoemulsification in eyes with uncontrolled ACG and Plateau iris. This approach may provide a safer and more effective alternative to traditional combined procedures. The case is part of an ongoing prospective study, with one-year results pending publication. However, studies with larger sample sizes and longer follow-up are needed to confirm the safety and efficacy of this two-step approach.
ACKNOWLEDGEMENTS
Lightmed Corporation provided cyclophotocoagulation probes for an ongoing prospective study related to the described case. The Lightmed Corporation did not interfere with the study design, data collection, analysis, and interpretation, writing of the report, and submission of the article for publication.
AUTHORS’ CONTRIBUTIONS:
Significant contribution to conception and design: Tiago Santos Prata, Isabella Cristina Tristão Pinto Resende, Daniela Mauricio Ribeiro, Fábio Nishimura Kanadani, Izabela Negrão Frota de Almeida. Data Acquisition: Tiago Santos Prata. Data Analysis and Interpretation: Tiago Santos Prata, Isabella Cristina Tristão Pinto Resende, Daniela Mauricio Ribeiro, Fábio Nishimura Kanadani, Izabela Negrão Frota de Almeida. Manuscript Drafting: Tiago Santos Prata, Isabella Cristina Tristão Pinto Resende, Daniela Mauricio Ribeiro, Fábio Nishimura Kanadani, Izabela Negrão Frota de Almeida. Significant intellectual content revision of the manuscript: Tiago Santos Prata, Isabella Cristina Tristão Pinto Resende, Daniela Mauricio Ribeiro, Fábio Nishimura Kanadani, Izabela Negrão Frota de Almeida. Final approval of the submitted manuscript: Tiago Santos Prata, Isabella Cristina Tristão Pinto Resende, Daniela Mauricio Ribeiro, Fábio Nishimura Kanadani, Izabela Negrão Frota de Almeida. Statistical analysis: not applicable. Obtaining funding: not applicable. Supervision of administrative, technical, or material support: Tiago Santos Prata. Research group leadership: Tiago Santos Prata.
REFERENCES
1. Junqueira DL, Prado VG, Lopes FS, Biteli LG, Dorairaj S, Prata TS. Non-pupillary block angle-closure mechanisms: a comprehensive analysis of their prevalence and treatment outcomes. Arq Bras Oftalmol. 2014;77(6):360-3.
2. Azuara-Blanco A, Burr J, Ramsay C, Cooper D, Foster PJ, Friedman DS, et al.; EAGLE study group. Effectiveness of early lens extraction for the treatment of primary angle-closure glaucoma (EAGLE): a randomised controlled trial. Lancet. 2016;388(10052):1389-97. Comment in: Arch Soc Esp Oftalmol. 2017;92(8):401-2; Natl Med J India. 2017;30(2):78-9. Comment on: Lancet. 2016;388(10052):1349; Lancet. 2016;388(10052):1352-4.
3. Tham CC, Kwong YY, Leung DY, Lam SW, Li FC, Chiu TY, et al. Phacoemulsification versus combined phacotrabeculectomy in medically uncontrolled chronic angle closure glaucoma with cataracts. Ophthalmology. 2009;116(4):725-31. Comment in: Ophthalmology. 2009;116(12):2478;author reply 2478-9. Ophthalmology. 2009; 116(12):2479; author reply 2479-80.
4. Almeida IN, Resende IC, Magalhães LM, Oliveira HK, Kanadani FN, Prata TS. Double-Arc slow-coagulation transscleral cyclophotocoagulation laser protocol: one-year effectiveness and safety outcomes. Ophthalmol Glaucoma. 2024;7(6):580-6.
5. Laroche D, Rickford K, Sakkari S. Case report: cataract extraction/lensectomy, excisional goniotomy, and transscleral cyclophotocoagulation: affordable combination MIGS for plateau iris glaucoma. J Natl Med Assoc. 2022;114(1):38-41.
6. Prata TS, Dorairaj S, De Moraes CG, Mehta S, Sbeity Z, Tello C, et al. Is preoperative ciliary body and iris anatomical configuration a predictor of malignant glaucoma development? Clin Exp Ophthalmol. 2013;41(6):541-5.
7. Nirappel A, Klug E, Neeson C, Chachanidze M, El Helwe H, Hall N, et al. Transscleral vs endoscopic cyclophotocoagulation: safety and efficacy when combined with phacoemulsification. BMC Ophthalmol. 2023;23(1):129.
8. Khodeiry MM, Sheheitli H, Sayed MS, Persad PJ, Feuer WJ, Lee RK. Treatment outcomes of slow coagulation transscleral cyclophotocoagulation in pseudophakic patients with medically uncontrolled glaucoma. Am J Ophthalmol. 2021;229:90-9.
9. Lai JS, Tham CC, Chan JC, Lam DS. Diode laser transscleral cyclophotocoagulation in the treatment of chronic angle-closure glaucoma: a preliminary study. J Glaucoma. 2003;12(4):360-4.
10. Shi Y, Oatts J, Tian J, Qiao C, Zhang Q, Han Y, et al. Low-dose transscleral cyclophotocoagulation with subsequent phacoemulsification in the treatment of prolonged acute primary angle closure. Br J Ophthalmol. 2023;107(2):221-6.
Submitted for publication:
February 4, 2025.
Accepted for publication:
June 27, 2025.
Approval of the Institutional Review Board: UNIFESP–Hospital São Paulo–Hospital Universitário da Universidade Federal de São Paulo–HSP/UNIFESP (CAAE: 14016619.3.0000.5505).
Data Availability Statement: The datasets generated and/or analyzed during the current study are included in the manuscript.
Edited by
Editor-in-Chief: Newton Kara-Júnior
Associate Editor: Heloisa Russ
Funding: This study received no specific financial support.
Disclosure of potential conflicts of interest: The authors declare no potential conflicts of interest.