

Tauanni Cândido1; Roberto Pineda2,3; Silvana Rossi1; Jéssica Véras Moura Lanza4; Newton Kara-Júnior1
DOI: 10.5935/0004-2749.2024-0084
ABSTRACT
PURPOSE: The OrbiTau surgical simulator is a synthetic eye model developed to enhance cataract surgical training. Herein, we aimed to describe the perspectives of Harvard’s Ophthalmology faculty and residents regarding the effectiveness of OrbiTau.
METHODS: A cross-sectional study was conducted in which 11 surgeons from the Massachusetts Eye and Ear Infirmary, with prior experience utilizing simulated phacoemulsification platforms, conducted cataract surgery with the OrbiTau. Subsequently, they completed a satisfaction questionnaire using the Likert scale.
RESULTS: Regarding the various OrbiTau components, 90.90% of the participants reported that the OrbiTau lens capsule was comparable to that of the human lens during capsulotomy. Furthermore, 72.72% of the participants found that the OrbiTau lens consistency was analogous to that of the human lens nucleus. Approximately 63.63% of the participants reported that the model’s posterior lens capsule resembled the native posterior capsule, and 72.72% of the participants noted that the model’s red reflex was similar to that of the dilated human pupil. Most participants believed that the OrbiTau was easier to use and more realistic than other commercially available simulators.
CONCLUSION: Our single-institution survey of the Orbitau demonstrated that this model realistically replicates ocular structures and may be a viable option for cataract surgery training.
Keywords: Cataract extraction/education; Simulation training/methods; Ophthalmology/education; Phacoemulsification/education; Ophthalmologists/education; Surgeons/education; High fidelity simulation training
INTRODUCTION
The use of synthetic tissue eye models has recently gained widespread acceptance in ophthalmic surgical education because of their replicability, potential for reuse, and cost-saving possibilities(1). The OrbiTau surgical simulator is a synthetic eye model designed to train ophthalmologists in phacoemulsification for cataracts. It is manufactured in Brazil and low in cost in comparison with other models such as Bioniko, SimulEye, Phake-I, Kitaro and Eyesi.
In this study, we aimed to elucidate the perspectives of faculty and residents of the University’s ophthalmology department with experience in performing simulated surgeries regarding the effectiveness of the OrbiTau artificial eye model in simulating phacoemulsification.
METHODS
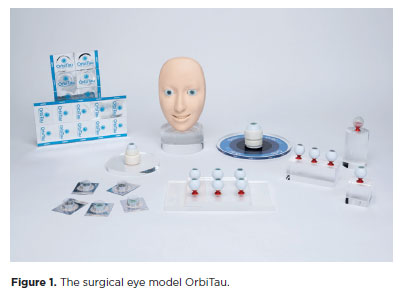
OrbiTau is an artificial eye model that can be used during surgical training to simulate the steps of cataract surgery. This synthetic eye model has a round, transparent upper structure with a convex anterior surface and a concave posterior surface. The dimensions, thickness, elasticity, mechanical resistance, texture, and malleability of the model are similar to those of the human cornea. The model’s anterior lens capsule is slightly elastic with low mechanical resistance and minimal resistance to rupture. The posterior capsule has similar characteristics and is slightly thinner than the anterior capsule. The iris is represented by a highly malleable laminar structure (Figure 1). The OrbiTau eye model allows for training in the steps of cataract surgery as well as the possible surgical complications such as rupture of the posterior capsule, anterior vitrectomy, and secondary implantation of an intraocular lens.
The study was conducted at the Massachusetts Eye and Ear Infirmary, Harvard Medical School. A wet lab was set up on a single day in July 2023, wherein 11 cataract surgeons who have used various commercially available simulators (e.g., Bioniko, SimulEye, Philips Eye, Kitaro, Phake-I and Eyesi) performed phacoemulsification using the OrbiTau simulator. The inclusion criterion was surgeons who have completed >15 h of surgical training using simulators or animal eyes.
To evaluate the effectiveness of the OrbiTau, a 5-point Likert scale(2) was used, which consisted of the following response options: 1, completely disagree or very dissatisfied; 2, disagree or dissatisfied; 3, neutral, 4, agree/satisfied; and 5, completely agree/very satisfied. The participants were allowed 4 h to perform phacoemulsification using the Orbitau simulator.
In this study, the CENTURION Vision System (Alcon, Fort Worth, TX, USA) was used to perform phacoemulsification. After the completion of the surgeries, each participant was asked to fill out a questionnaire regarding the OrbiTau’s usability, structure, similarity to the human eye, and differences from other simulators that they have used. To ensure participants were comfortably in expressing their opinions on the model, no personal information was collected in the questionnaire.
Ethical considerations
The study was approved by the institution’s Ethics Committee (CEP number: 5.959.616; date: March 23, 2023).
RESULTS
Approximately 90.90% of the participants reported that the OrbiTau lens capsule was similar to that of a human lens during capsulotomy. Furthermore, 72.72% of the participants found that the consistency of the OrbiTau lens was analogous to that of the human lens nucleus. Approximately 63.63% of the participants reported that the posterior lens capsule resembled the native posterior capsule, and 72.72% of the participants found that the model’s red reflex was similar to that of a dilated human pupil. Most participants agreed that the OrbiTau was easier to use and more realistic than other commercially available surgical eye simulators. The surgeons’ perspectives regarding the degree of similarity between the OrbiTau components and the human eye are presented in table 1. Most participating surgeons indicated that the OrbiTau eye model was highly similar to the human eye (Table 1).
The reproducibility of the surgical steps using the OrbiTau surgical simulator were evaluated. The incision, capsulorhexis, and phacoemulsification maneuvers stood out for their reproducibility, with satisfaction rates of 90.9%, 90.9%, and 72.72%, respectively. These results demonstrate the effectiveness of the simulator in replicating these surgical steps. Thus, OrbiTau provides a realistic and high-quality experience, especially in the challenging phases of the procedure such as capsulorhexis, fracture, and nucleus capture (Table 2).
Table 3 highlights the results obtained from the evaluation of the OrbiTau surgical simulator by the study participants. The completed questionnaires revealed a positive feedback and favorable responses regarding the model’s ease of use, representation of ocular structures, and ability to provide comprehensive training (Table 3).
Table 4 shows the advantages of the OrbiTau simulator over the other simulators according to the participants’ previous experiences. Approximately 72.72% of the respondents agreed that OrbiTau was superior to other previously used simulators (e.g., Bioniko, SimulEye, Phake-I, Kitaro, and Eyesi) in terms of usability and representation of ocular structures. Furthermore, they reported that OrbiTau provided a more realistic surgical training experience than the other simulators (Table 4).
DISCUSSION
Cataract is one of the major causes of blindness worldwide, affecting millions of people, especially those aged >60 years(3,4). Thus, the surgical training of ophthalmologists performing cataract surgeries is of significant social relevance. Cataract surgery requires dexterity on the part of the ophthalmic surgeon(3,5). Therefore, a significant number of ophthalmologists in Latin America abstain from performing cataract surgery, primarily due to concerns of insecurity and inadequate surgical training(4).
Several simulators have been evaluated for their effectiveness in surgical training(6-10). According to Belyea et al., residents who trained using a simulator exhibited shorter phacoemulsification times, a lower percentage of phaco energy delivered, fewer intraoperative complications, and a shorter learning curve(10). Dean et al.(11) also highlighted the advantages of using simulators. According to Raval et al.(12), the SimulEYE and Kitaro capsular excision models are similar to human capsular tissue. Studies have also found that training becomes more standardized using a simulated artificial eye than using a live surgical environment(11).
Lucas et al. concluded that training with the Eyesi® cataract surgery simulator significantly reduced the total number of intraoperative complications during the first 10 phacoemulsification surgeries performed by ophthalmology residents(8). Other studies have demonstrated that supervised training on simulators is efficient in providing surgeons with confidence during the learning curve(13).
In our study, most of the participating surgeons agreed that the OrbiTau cornea was similar to the human cornea (Table 1), which probably reflects the predominant perception that the incision maneuver was reproducible (Table 2). The same perspective was noted regarding the anterior lens capsule, capsulorhexis maneuver, consistency of the lens nucleus during phacoemulsification, and the nucleus fracture and disassembly steps, including the aspiration/emulsification of the fragments.
For a cataract surgery simulator to be effective, it should adequately replicate the steps of capsulorhexis and emulsification because they are considered the most difficult to learn and have the greatest potential for complications(13-16). In our study with the OrbiTau, the incision, capsulorhexis, and fracture and disassembly stages received a satisfaction level of 90.9%, 90.9%, and 72.72%, respectively, for simulated performance. The participants also expressed appreciation for the replication of the posterior lens capsule, red reflex intensity of the simulator’s retinal component, and the hydrodissection and nucleus rotation maneuvers (Table 2). Overall, the OrbiTau was considered favorably by the ophthalmology surgeons at Harvard (Table 3).
Table 4 shows the main factors that differentiate the OrbiTau surgical simulator from other existing simulators, and it is based on the participants’ previous experience with other surgical models. Among the study participants, 73.73% agreed that the OrbiTau simulator was easy to use, represented the ocular structures well, and allowed for comprehensive surgical training.
Although the study is limited by its small sample size, it is the first to be conducted using the OrbiTau simulator and demonstrates its potential utility in surgical training. Another limitation of the study is that comparisons between the OrbiTau simulator and other available models were based on the participants’ subjective perceptions. Future studies could benefit from a one-on-one comparison between the simulators.
In conclusion, using the OrbiTau simulator allows for safe, reproducible, and practical training in the critical steps of phacoemulsification. This highlights the simulator’s potential to meet the need for a safer and more efficient method of surgical training, especially in regions where access to hands-on training is limited.
AUTHORS’ CONTRIBUTION:
Significant contribution to conception and design: Tauanni Cândido, Newton Kara-Junior. Data analysis and interpretation: Tauanni Cândido, Roberto Pineda, Silvana Rossi, Jéssica Véras Moura Lanza, Newton Kara-Junior. Manuscript drafting: Tauanni Cândido, Silvana Rossi, Jéssica Véras Moura Lanza, Newton Kara-Junior. Significant intellectual content revision of the manuscript: Roberto Pineda, Newton Kara-Junior. Final approval of the submitted manuscript: Tauanni Cândido, Roberto Pineda; Silvana Rossi, Jéssica Véras Moura Lanza, Newton Kara-Junior. Statistical analysis: not applicable. Obtaining funding: not applicable. Supervision of administrative, technical, or material support: Newton Kara-Junior. Research group leadership: Newton Kara-Junior.
REFERENCES
1. Hu KS, Pettey J, Soohoo JR. The role of technology in ophthalmic surgical education during COVID-19. Curr Surg Rep [Internet]. 2022 [cited 2023 Dec 21];10(12):239-45. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC9662128/
2. Jebb AT, Ng V, Tay L. A review of key Likert scale development advances: 1995-2019. Front Psychol [Internet]. 2021 [cited 2023 Aug 24];12:637547. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC8129175/
3. Koch CR, Neves de F, Paredes RS, Siqueira AR, Kara-Junior N. Impact of cataract surgery on visual acuity and quality of life using the National Eye Institute visual function questionnaire 25 in a public teaching hospital in Brazil. Rev Bras Oftalmol [Internet]. 2022 [cited 2023 Nov 21];81:e0011. Available from: https://www.scielo.br/j/rbof/a/fgJ337dGWGP3KtmhtHN35zv/abstract/?lang=en
4. Lee CM, Afshari NA. The global state of cataract blindness. Curr Opin Ophthalmol. 2017;28(1):98-103.
5. Kara-Junior N. Technology, teaching, and the future of ophthalmology and the ophthalmologist. Arq Bras Oftalmol [Internet]. 2018 [cited 2023 Nov 24];81(3):V-VI. Available from: https://www.scielo. br/j/abo/a/KQsBS4psN8Ywx93dP3tjyNR/?lang=en
6. Ferrara M, Romano V, Steel DH, Gupta R, Iovino C, van Dijk EH; OphthaTraining Group; Romano MR. Reshaping ophthalmology training after COVID-19 pandemic. Eye (Lond). 2020;34(11):2089-97. Comment in: Eye (Lond). 2021;35(8):2316-8. Eye (Lond). 2022; 36(7):1505-6.
7. Lee R, Raison N, Lau WY, Aydin A, Dasgupta P, Ahmed K, et al. A systematic review of simulation-based training tools for technical and non-technical skills in ophthalmology. Eye (Lond). 2020;34(10):1737-59. Comment in: Eye (Lond). 2021;35(7):2051-2. Eye (Lond). 2022;36(6):1333-4.
8. Lucas L, Schellini SA, Lotelli AC. Complications in the first 10 cataract surgeries using phacoemulsification with and without previous simulator training. Arq Bras Oftalmol [Internet]. 2019 [cited 2023 Jun 24];82(4):289-94. Available from: https://www.scielo.br/j/abo/a/xtQkH6jCGzn5QPgW7kfWkxF/?lang=en
9. Bisol T, Bisol R, Rezende F. Efficacy of Eyesi® surgical simulator training in improving high-tension capsules capsulorhexis performance. Rev Bras Oftalmol [Internet]. 2016 [cited 2023 Nov 20];75(5):376-9. Available from: https://www.scielo.br/j/rbof/a/5dmnc5L5ZtwKK4rhhVwhCqz/?lang=en
10. Belyea DA, Brown SE, Rajjoub LZ. Influence of surgery simulator training on ophthalmology resident phacoemulsification performance. J Cataract Refract Surg. 2011;37(10):1756-61.
11. Dean WH, Gichuhi S, Buchan JC, Makupa W, Mukome A, Otiti-Sengeri J, et al. Intense simulation-based surgical education for manual small-incision cataract surgery: the ophthalmic learning and improvement initiative in cataract surgery randomized clinical trial in Kenya, Tanzania, Uganda, and Zimbabwe. JAMA Ophthalmol. 2021;139(1):9-15. Comment in: JAMA Ophthalmol. 2021;139(1):16-7.
12. Raval N, Hawn V, Kim M, Xie X, Shrivastava A. Evaluation of ophthalmic surgical simulators for continuous curvilinear capsulorhexis training. J Cataract Refract Surg. 2022;48(5):611-5.
13. Mangan MS, Atalay E, Arıcı C, Tuncer İ, Bilgeç MD. Comparison of different types of complications in the phacoemulsification surgery learning curve according to the number of operations performed. Turk J Ophthalmol [Internet]. 2016 [cited 2023 Jun 21];46(1):7-10. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC5076311/
14. Rutar T, Porco TC, Naseri A. Risk factors for intraoperative complications in resident-performed phacoemulsification surgery. Ophthalmology. 2009;116(3):431-6.
15. Dooley IJ, O’Brien PD. Subjective difficulty of each stage of phacoemulsification cataract surgery performed by basic surgical trainees. J Cataract Refract Surg. 2006;32(4):604-8.
16. Woodfield AS, Gower EW, Cassard SD, Ramanthan S. Intraoperative phacoemulsification complication rates of second- and third-year ophthalmology residents: a 5-year comparison. Ophthalmology. 2011;118(5):954-8.
Submitted for publication:
July 19, 2024.
Accepted for publication:
October 31, 2024.
Approved by the following research ethics committee: Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo – HCFM/USP (CAAE: 67796223.4.0000.0068).
Funding: This study received no specific financial support.
Disclosure of potential conflicts of interest: Tauanni Cândido is the creator of Orbitau. The other authors declare that there are no conflicts of interest.