

Luiz Formentin; Yandely Chihuantito Choquechambi; Natalia Pereira Felix de Araujo; Samantha de Albuquerque Mori Miyazawa; Helena Maria Costa Oliveira; Rodrigo Teixeira Santos
DOI: 10.5935/0004-2749.2023-0332
ABSTRACT
PURPOSE: This study aimed to modify scleral contact lenses to achieve a desired compression standard and to evaluate the effectiveness and reliability of the adjustments.
METHODS: In this nonrandomized, noncomparative, and partially masked study Scleral contact lens fittings were analyzed in 20 eyes of 12 patients (50% women, 50% men) diagnosed with keratoconus. Participants were selected based on their need for scleral contact lenses (SCLs), which was determined in complete ophthalmological examinations. Patients were tested with Zenlens scleral contact lenses (Bausch & Lomb, Vaughan, Ontario, Canada). We evaluated compression in the lens support area after one hour of use, excluding cases of peripheral lifting. Photos of the adaptations were sent to five experts for analysis of the quadrants (nasal, temporal, superior, and inferior). We used Fisher's exact test for statistical analysis.
RESULTS: The proposed adjustment was highly effective (93.5% correct) in lens delivery (BL=0), with the interrater agreement between doctors ranging from 68.8% to 80.9%.
CONCLUSION: The clinical parameters proposed for scleral contact lenses adjustment proved useful and reproducible, enabling their practical application to scleral lens adaptation.
Keywords: Contact lenses; Lifting; Keratoconus; Rehabilitation
INTRODUCTION
There have been numerous technological advances in scleral contact lenses (SCLs), including improved covering materials, designs, and manufacturing techniques. SCLs have seen a marked resurgence after nearly a century of relative dormancy(1,2).
In 1983, Ezekiel published the first description of lenses made from materials with greater gas permeability (rigid gas permeable [RGP]), which significantly reduced the risk of hypoxic complications of daily SCL use(3) seen with polymethylmethacrylate (PMMA) lenses. This caused renewed interest in the potential use of SCLs(4-6).
Further improvements built on this lens model, and the evolution of computerized lathes allowed highly complex designs. Among the most significant advances to which this has led are the development of prolate and oblate lens profiles, and the ability to make lens adjustments to sagittal height (SAG), limbal curve height, and the support area. Studies have identified a high prevalence of scleral asymmetry, and this can have a significant impact on proper lens fit. Precise alignment of the scleral lens support with the ocular surface is extremely important for properly fitting lenses(7).
Furthermore, there are several variations of the corneoscleral transition. Barnett et al. have found significant differences in the corneoscleral junction (CSJ), which is greater along the horizontal than the vertical meridian. CSJ angles vary between the four quadrants, being the most pronounced in the nasal, followed by the inferior, superior, and temporal quadrants. The flatter scleral curvature seen in the latter may explain the clinically observed temporal decentering of lenses(8).
Adjustments to the support area are fundamental to patient comfort and this increases lens wear time, as it is estimated that approximately 10% of SCL wearers discontinue their use due to discomfort(9). This discomfort can be attributed to several causes, including poor scleral landing zone fit. Wearing spherical SCLs can cause patients to squint, decentering the lens to a specific area, usually the quadrant in which the lens does not align properly with the sclera(10).
To deepen our understanding of the optimum adjustment requirements for SCLs, the main objective of this study was to evaluate the landing zone areas of SCL wearers for compression and identify possible SCL corrections. In so doing, we hoped to identify adjustment patterns that could be easily found using slit-lamp analysis.
METHODS
This was a nonrandomized, noncomparative, and partially masked study. SCL fittings were evaluated in 20 eyes of 12 patients, including 6 women (50%) and 6 men (50%). All of the patients had keratoconus. After undergoing a complete ophthalmological examination, each participant was advised to wear contact lenses. Each patient underwent a scleral lens adaptation test due to a clear indication for SCLs, an ocular surface disease, or the failure of rigid gas permeable (RGP) corneal contact lenses to meet their optical needs.
This study was conducted in accordance with the tenets of the 2013 revision of the Declaration of Helsinki and approved by the Ethics Commission for Analysis of Research Projects CEP/UNIFESP (1340/2017; CAAE: 79411117.8.0000.5505). All patients were fully informed of the study aims and procedures and gave informed consent to participation.
The tests were performed using Zenlens scleral lenses (Bausch & Lomb, Vaughan, Ontario, Canada). These are SCLs with a multicurve design that allows personalized but standardized adjustments to the anterior and posterior surfaces of the lens. Possible modifications include adjustments to the anterior toricity, the limbal release curve (LCC), the flexion control, the microvault, and the advanced peripheral system(11).
Patients were initially left wearing new SCLs for an hour and then each eye quadrant was evaluated to determine the levels of compression at 0, 1, 2, 3, and 4. Previous research has shown that the ideal waiting time before the initial evaluation of SCLs is 30 to 40 minutes. We chose to wait 60 minutes to ensure the fullest adaptation(12). There were some cases in which, instead of compression, there was lifting of the periphery; however, as these were exceptions, we did not include these cases in this study. For each level of compression, a specific adjustment was made, as shown in Table 1(13).
We then sent photos to five experts of each quadrant (nasal, temporal, superior, and inferior) of each eye before and after the adaptations. Photos corresponding to the compression classifications were collected in a spreadsheet. Figure 1 shows photos of eyes classified as A to E according to compression level. It is important to highlight that the experts were blinded as to whether each photo was taken before or after lens adaptation, which photos corresponded to which patient, or whether each photo was of a left or right eye.
Statistical methodology
Comparisons of the distribution of correct classifications (a classification equal to zero at lens delivery [BL]) were carried out using Fisher's exact tests (more than 20% of cells in a contingency table with expected values lower than five).
For all statistical tests, p-values <0.05 were considered significant. Analyses were performed using SPSS Statistics for Windows, version 20.0 (IBM Corp, Armonk, NY, USA) and STATA, version 17 (StataCorp. LLC, College Station, TX, USA) software.
RESULTS
Our statistical analyses addressed two main points: the effectiveness of the adjustment proposal and the level of agreement between doctors using the proposal.
As can be seen in Table 2, 93.5% of the 77 postadjustment photographs (three of 80 photos were discarded due to poor quality), had a BL equal to zero, indicating that the correct adjustment had been made. This result was not heterogeneous according to the classifications initially assigned (p=0.072). Additionally, it was found that, among the cases in which no adjustment was required or made, only one (20%) showed no reduction in compression severity (and corresponding classification) at the initial assessment (test=1 and BL=1). Attached (attachments 1, 2, 3, and 4) are some examples of the support relationship observed in the test of eyes with adjusted lenses. With both the trial lenses and the customized lenses, the following parameters were used: diameter, 16 and 17 mm; deep sagittal, 4,500 up 6.100 microns; back curve, 6.4 up 9.0 mm; prolate and oblate design; landing zone up to +300 microns in each quadrant.
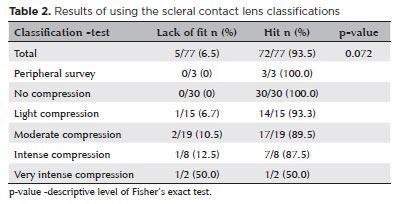
Table 3 presents the percentages of correct answers per assessing doctor in relation to the classifications of the referring doctor. Only cases with a BL equal to zero were considered, excluding the "peripheral survey" category. In the expert evaluations, classifications that agreed with our own or differed by just 1 level (above or below) were considered acceptable. Using these criteria, the percentages of correct answers ranged from 68.8%-80.9%, indicating good accuracy.
Figure 2 compares the pre- and postadjustment clinical outcomes in the area covered by the SCL landing zone.
DISCUSSION
The use of SCLs can change a patient's life, reestablishing the vision necessary for their work and leisure activities, either by improving visual acuity or by protecting the cornea in ocular surface diseases. Naturally, the longer the duration for which a patient can wear their lenses, the better, and this depends on lens safety and comfort(8,9).
Barnett et al. have demonstrated that quadrant-specific lenses provide improved fit, reducing the number of patients reporting a need to remove their lenses during the day. This discovery shows the importance of using lenses with specific support areas for better patient-specific adaptation and comfort(8). Ritzmann et al. found that scleral asymmetry begins at the limbus, which is the most symmetrical area, and increases toward the extraocular muscles. Asymmetrical variation can influence the fit and stability of SCLs, as each lens must be adapted to the individual scleral curvature. Understanding these scleral characteristics and their variations is essential for adequate adaptation that ensures the comfort and effectiveness of each lens(14). To increase success with SCLs, adjustments to the support zone should be as accurate as possible. Although there are now devices able to approximate the scleral anatomy of the cornea(15), they are costly and the perfect fit still depends on slit-lamp analysis. To our knowledge, this is the first study to relate clinical presentation to the degree of adjustment required per quadrant.
To perform this study, we observed the reactions of blood vessels to the SCL landing zone. We observed five stages: 1) no pressure; 2) light pressure with a difference in color between the free conjunctiva and sub-SCL; 3) moderate pressure, as for stage 2 plus obstruction of small vessels; 4) intense pressure, as for stage 2 plus obstruction of medium vessels; 5) very intense pressure, obstruction of medium vessels and an acute pattern.
Based on our compression classifications, we adjusted the support zone to establish the optimal resistance of the part of the SLC facing the sclera based on the importance of good lens support in the conjunctiva/sclera. By adjusting the symmetry and landing zone of the SCL we established the corrections most suited to each classification. The SCL customizations were successful in around 90% of cases. We then considered whether the system was viable for use by other ophthalmologists. At this point, we mashed up photos of the landing zone (support area) before sending them to five ophthalmologists for evaluation. For each lens, we obtained four photos, one for each quadrant. There were two lenses used with each eye, a trial lens and a custom lens, amounting to eight photos per eye. As we treated 20 eyes, we obtained 160 photos. After these were merged, they were sent to five ophthalmologists for compression level classification to determine the level of agreement with our own classifications and the practical validity of these classifications and customizations. The interrater agreement levels were good, indicating that our system offers a feasible approach to improved SCL fitting.
A limitation of this study was the small number of cases with intense compression. Also, a possible problem with the proposed approach is the difficulty of reproducing images from slit lamps. Agreement levels may be higher when the system is used in real-world situations.
All of the participants in this study had keratoconus and received the same SCL model as we were concerned only with the landing zone. Nevertheless, our findings may be applicable to other scleral lens models and patients with different corneal diseases such as pellucid marginal degeneration or postcorneal transplant adaptation, but further studies are needed to investigate this. The clinical parameters proposed for scleral support area adjustments proved useful and reproducible, supporting their future use in scleral lens fitting practices.
AUTHORS' CONTRIBUTION
Significant contribution to conception and design: Luiz Formentin, Yandely Chihuantito Choquechambi. Data acquisition: Yandely Chihuantito Choquechambi, Natalia Pereira Felix de Araujo, Samantha de Albuquerque Mori Miyazawa, Helena Maria Costa Oliveira, Rodrigo Teixeira Santos. Data analysis and interpretation: Luiz Formentin, Yandely Chihuantito Choquechambi. Manuscript drafting: Luiz Formentin, Yandely Chihuantito Choquechambi. Significant intellectual content revision of the manuscript: Samantha de Albuquerque Mori Miyazawa, Helena Maria Costa Oliveira, Rodrigo Teixeira Santos. Final approval of the submitted manuscript: Luiz Formentin, Yandely Chihuantito Choquechambi, Natalia Pereira Felix de Araujo, Samantha de Albuquerque Mori Miyazawa, Helena Maria Costa Oliveira, Rodrigo Teixeira Santos. Statistical analysis: Luiz Formentin. Supervision of administrative, technical, or material support: Luiz Formentin. Research group leadership: Luiz Formentin.
REFERENCES
1. Rosenthal P. The Boston Lens and the management of keratoconus. Int Ophthalmol Clin. 1986;26(1):101-9.
2. Romero-Rangel T, Stavrou P, Cotter J, Rosenthal P, Baltatzis S, Foster CS. Gas-permeable scleral contact lens therapy in ocular surface disease. Am J Ophthalmol. 2000 Jul;130(1):25-32.
3. Ezekiel D. Gas permeable haptic lenses J Br Contact Lens Assoc. 1983;6(4):158-61.
4. Ruben C, Benjamin W. Scleral contact lenses: preliminary report on oxygen-permeable materials. Contact Lens J. 1985;13:5-9.
5. Bleshoy H, Pullum KW. Corneal response to gas-permeable impression scleral lenses. J Br Contact Lens Assoc. 1988;11(2):31-4.
6. Giovedi Filho R, Giovedi M. Materiais, classificação e forma de uso das lentes de contato. Coral-Ghanem C, Kara José N, editors. Lentes de contato Rio de Janeiro: Cultura Médica. 2003. p.1-2.
7. Barnett M, Carrasquillo KG, Schornack MM. Clinical outcomes of scleral lens fitting with a data-driven, quadrant-specific design: multicenter review. Optom Vis Sci. 2020;97(9):761-5.
8. Barnett M, Fadel D. Scleral lenses: benefits of toric landing zones. Contact Lens Spectrum. 2017;32:36-41.
9. Consejo A, Behaegel J, Van Hoey M, Iskander DR, Rozema JJ. Scleral asymmetry as a potential predictor for scleral lens compression. Ophthalmic Physiol Opt. 2018;38(6):609-16.
10. Russell B. visual rehabilitation with contact lenses for irregular corneal astigmatism. Can J Optom. 2016;78 Suppl 1:4-17.
11. Lipener C, Rosa J. Clinical experience with adjustable scleral lenses. Arq Bras Oftalmol. 2023;86(1):38-45.
12. Barnett M. The right fit for the irregular cornea: smooth things over with scleral lenses: new scleral designs can help patients with irregular corneas stay happy and healthy in contact lenses. Rev Optom. 2017;154(8):46-53.
13. Esen F, Toker E. Influence of Apical Clearance on Mini-Scleral Lens Settling, Clinical Performance, and Corneal Thickness Changes. Eye Contact Lens. 2017;43(4):230-5.
14. Ritzmann M, Morrison S, Caroline P, Kinoshita B, Lampa M, Kojima R. Scleral shape and asymmetry as measured by OCT in 78 normal eyes. [Poster presented at the Global Specialty Lens Symposium. 2016; 2016.p. 21-4.]
15. DeNaeyer G, Sanders DR. sMap3D corneo-scleral topographer repeatability in scleral lens patients. Eye Contact Lens. 2018;44 Suppl 1:S259-64.
Submitted for publication:
March 4, 2024.
Accepted for publication:
September 11, 2024.
Approved by the following research ethics committee: Universidade Federal de São Paulo - UNIFESP (CAAE: 79411117.8.0000.5505).
Funding: This study received no specific financial support.
Disclosure of potential conflicts of interest: The authors declare no potential conflicts of interest.