

Juliana Mika Kato1; Eduardo Ferracioli Oda1; Thaisa Silveira Barbosa1; Flavia Rossi2; Andre Mario Doi2; Carolina dos Santos Lazari2; Tatiana Tanaka1; Joyce Hisae Yamamoto1
DOI: 10.5935/0004-2749.2023-0290
ABSTRACT
PURPOSE: The microbiology pattern of neonatal conjunctivitis has changed over time, and the incidence of gonococcal conjunctivitis is almost nil. This study aimed to determine the etiology of neonatal conjunctivitis cases referred to a tertiary health center in Brazil.
METHODS: From 2017 to 2020, conjunctival swabs were taken from neonates with clinical signs of conjunctivitis and tested with bacterial culture and polymerase chain reaction for Neisseria gonorrhoeae and Chlamydia trachomatis.
RESULTS: A total of 51 neonates were included in the 3-year study. Chlamydial conjunctivitis was diagnosed in 39 (76.5%) patients, and microbial growth was detected in 13 (25.5%) patients. The most isolated bacterium was Staphylococcus epidermidis (n=6, 11.8%), followed by other coagulase-negative Staphylococcus species (n=4, 7.8%) and S. aureus (n=2, 3.9%). One S. aureus isolate was resistant to oxacillin. There were no cases of gonococcal conjunctivitis. Ten (19.6%) patients showed polymerase chain reaction-negative C. trachomatis and negative bacterial culture test results.
CONCLUSION: Findings show that C. trachomatis is the most common pathogen causing neonatal conjunctivitis. The high prevalence of C. trachomatis infection highlights the importance of screening and treating pregnant woman.
Keywords: Conjunctivitis; Infant, newborn, diseases; Ophthalmia neonatorum; Chlamydia infections; Sexually transmitted diseases
INTRODUCTION
Neonatal conjunctivitis is defined as conjunctivitis occurring anytime during the first 30 days of life and is considered the most common infection during the neonatal period. Its incidence varies depending on the patient's sociodemographic conditions. Neonatal conjunctivitis has traditionally been associated with Neisseria gonorrhoeae and Chlamydia trachomatis infection. However, Credè's method of prophylaxis with a single drop of 2% silver nitrate solution immediately after birth has decreased the incidence of gonococcal conjunctivitis to almost nil(1). Recent studies have identified Staphylococcus aureus and S. epidermidis as the most common bacterial species causing neonatal conjunctivitis(2). Therefore, this study aimed to determine the etiology of neonatal conjunctivitis cases referred to a tertiary health center in São Paulo, Brazil.
METHODS
From 2017 to 2020, conjunctival swabs were taken from neonates with clinical signs of conjunctivitis referred to the Hospital das Clínicas, Faculdade de Medicina da Universidade de São Paulo (HC-FMUSP). Symptoms included ocular discharge, hyperemia, and swelling of the eyelids. We tested the samples for the presence of N. gonorrhoeae using bacterioscopy with Gram staining, chocolate agar, and Thayer-Martin agar cultures and for the presence of C. trachomatis with polymerase chain reaction (PCR) using the Abbott Real Time CT/NG Amplification Kit (Abbott Molecular Inc., IL, USA)(3). Epidemiological and clinical data were collected from the patients' medical records. The recommended treatment was intramuscular injection of ceftriaxone (a single dose of 50 mg/kg) and azithromycin oral syrup (20 mg/kg/day) once daily for 3 days(3). All cases were referred to the Pediatric Emergency Center of the HC-FMUSP for systemic evaluation.
This study was approved by the Institutional Ethics Committee of the HC-FMUSP.
RESULTS
A total of 64 neonates were admitted to the Ophthalmology Emergency Center of the HC-FMUSP during the 3-year study period. Of these, 13 (20.3%) patients were excluded due to insufficient microbiological data. The main findings of the remaining 51 (79.7%) patients are presented in table 1. The patients' mean age at presentation was 17.6 (range 7-33) days, and the average duration of symptoms was 8.9 (range 1-24) days. Most cases were vaginal deliveries (n=39, 76.5%), and the majority of the mothers (n=30, 58.8%) reported some complications during pregnancy, including urinary tract infections, premature rupture of membranes, or vaginal discharge.
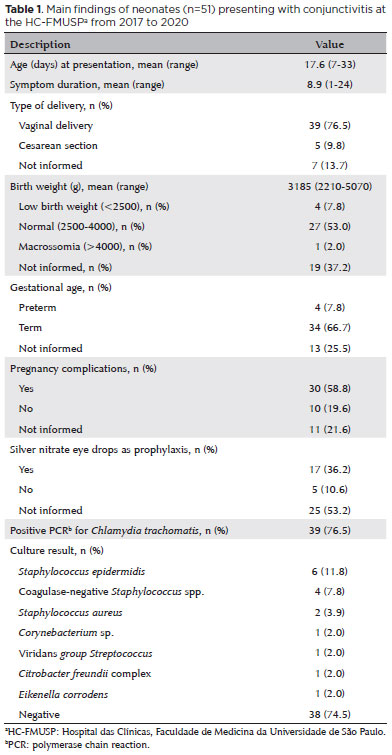
Chlamydial conjunctivitis was diagnosed with PCR in 39 (76.5%) patients, and microbial growth was detected in 13 (25.5%) patients. The most isolated bacterium was S. epidermidis (n=6, 11.8%), followed by other coagulase-negative Staphylococcus species (n=4, 7.8%) and S. aureus (n=2, 3.9%). One S. aureus isolate was resistant to oxacillin (methicillin-resistant Staphylococcus aureus [MRSA]). There were no cases of gonococcal conjunctivitis. In addition, 12 (23.5%) patients showed PCR-positive C. trachomatis and also positive bacterial culture results, including 3 (25.0%) multibacterial cases, while 10 (19.2%) patients showed PCR-negative C. trachomatis and negative bacterial culture results.
DISCUSSION
In this study, C. trachomatis was the most common pathogen found to cause neonatal conjunctivitis, accounting for 76.5% of the cases. This prevalence markedly surpasses the reported range of 0%-46% in the literature(4,5). Studies investigating C. trachomatis infection among women in Brazil have reported a prevalence of 12%-31%(6). The HC-FMUSP, however, is a tertiary referral center and receives patients with high-risk pregnancies and a greater risk of complications compared to most other institutes.
Since C. trachomatis infection is associated with pregnancy complications, such as premature rupture of membranes, preterm delivery, growth restrictions, and fetal loss, the estimated prevalence is understandable but alarming. Previous studies have used widely different methods of identifying C. trachomatis in neonatal conjunctivitis cases or did not even test for it. Detecting the etiological agent may have been difficult due to the unavailability of current technologies, such as PCR.
Studies on the microbiology of neonatal conjunctivitis have reported varying rates of culture positivity, ranging from 0% to 83%, as well as the prevalence of other coagulase-negative Staphylococcus species and S. aureus(4,5). In this study, microbial growth was detected in 25.0% of the patients. These microorganisms, however, may be part of the normal ocular flora and might not be directly related to neonatal conjunctivitis. Distinguishing between a colonizing agent and a true pathogen is a challenge from a microbiological perspective, especially given the difficulty in sterile specimen collection from an unwilling newborn. The high rate of positive bacterial culture results in this study may also be related to the higher frequency of vaginal deliveries compared to cesarian deliveries.
Of the 51 cases, 19.6% tested negative for C. trachomatis and other bacteria. These cases could be due to viral pathogens, chemical irritants, or nasolacrimal duct obstruction. However, viral PCR is not routinely performed at the HC-FMUSP.
As neonates with untreated mothers have a 50% chance of developing conjunctivitis and up to a 20% chance of developing pneumonia, screening of pregnant women is strongly recommended. Silver nitrate solution does not prevent chlamydial conjunctivitis, and the evidence of antibiotic ointments decreasing the incidence of chlamydial conjunctivitis is sparse(7).
The findings of this single-center study conducted in São Paulo, Brazil, may offer insights into chlamydial conjunctivitis infection among the broader Brazilian population. We strongly advocate for routine screening and treatment of pregnant women during prenatal care in order to prevent both pregnancy-related and neonatal complications.
AUTHORS' CONTRIBUTIONS:
Significant contribution to conception and design: Eduardo Ferracioli Oda, Joyce Hisae Yamamoto. Data acquisition: Juliana Mika Kato, Eduardo Ferracioli Oda, Thaisa Silveira Barbosa. Data analysis and interpretation: Juliana Mika Kato, Tatiana Tanaka, Joyce Hisae Yamamoto, Andre Mario Doi, Carolina dos Santos Lazari. Manuscript drafting: Juliana Mika Kato. Significant intellectual content revision of the manuscript: Joyce Hisae Yamamoto. Final approval of the submitted manuscript: Juliana Mika Kato, Eduardo Ferracioli Oda, Thaisa Silveira Barbosa, Flavia Rossi, Andre Mario Doi, Carolina dos Santos Lazari, Tatiana Tanaka, Joyce Hisae Yamamoto. Statistical analysis: Juliana Mika Kato. Obtaining funding: not applicable. Supervision of administrative, technical, or material support: Flavia Rossi, Joyce Hisae Yamamoto. Research group leadership: Joyce Hisae Yamamoto.
REFERENCES
1. US Preventive Services Task Force; Curry SJ, Krist AH, Owens DK, Barry MJ, Caughey AB, Davidson KW, Doubeni CA, Epling JW Jr, Kemper AR, Kubik M, Landefeld CS, Mangione CM, Silverstein M, Simon MA, Tseng CW, Wong JB. Ocular Prophylaxis for Gonococcal Ophthalmia Neonatorum: US Preventive Services Task Force Reaffirmation Recommendation Statement. JAMA. 2019;321(4):394-8.
2. Pak KY, Kim SI, Lee JS. Neonatal Bacterial Conjunctivitis in Korea in the 21st Century. Cornea. 2017;36(4):415-8.
3. Oda EF, Kato JM, Barbosa TS, Rossi, F, Doi AM, Tanaka T, et al. Neonatal conjunctivitis at a Brazilian tertiary center: the current relevance of Chlamydia trachomatis. Arq Bras Oftalmol. 2022;85(4 Supl): 7-30.
4. Gildea D, Goetz R, Drew R, Chamney S. Ophthalmia neonatorum in a tertiary referral children's hospital: A retrospective study. Eur J Ophthalmol. 2022;32(1):587-91.
5. Honkila M, Renko M, Ikäheimo I, Pokka T, Uhari M, Tapiainen T. Aetiology of neonatal conjunctivitis evaluated in a population-based setting. Acta Paediatr. 2018;107(5):774-9.
6. Machado MS, Costa e Silva BF, Gomes IL, Santana IU, Grassi MF. Prevalence of cervical Chlamydia trachomatis infection in sexually active adolescents from Salvador, Brazil. Braz J Infect Dis. 2012; 16(2):188-91.
7. Smith-Norowitz TA, Ukaegbu C, Kohlhoff S, Hammerschlag MR. Neonatal prophylaxis with antibiotic containing ointments does not reduce incidence of chlamydial conjunctivitis in newborns. BMC Infect Dis. 2021;21(1):270.
Submitted for publication:
June 6, 2024.
Accepted for publication:
June 26, 2024.
Approved by the following research ethics committee: Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo - USP (CAAE: 82678218.5.0000.0068).
Funding: This study received no specific financial support.
Disclosure of potential conflicts of interest: The authors declare no potential conflicts of interest.