

Weimin Zhang1; Shujuan Wang1; Yingcheng Lin2; Min Zhou2,3
DOI: 10.5935/0004-2749.2024-0128
An 11-year-old girl presented to our clinic with a fractured lens in her right eye following two years of orthokeratology lens wear. The central area of the lens appeared feathery, indicating damage, while the surrounding area was unaffected. Fluorescence staining confirmed the corneal integrity, indicating that the damage was the result of the negative pressure generated when using a tool to remove the lens from the central region. This highlights the importance of proper care and handling during the fitting and maintenance of orthokeratology lenses(1). Contact lens users are predisposed to complications such as bacterial colonization(2), corneal abrasions(3), and suboptimal outcomes. Therefore, proper lens maintenance and adherence to careful application and removal techniques are crucial. The lens should be removed from the periphery to avoid generating excessive negative pressure at the center, thereby preventing corneal adhesions and potential damage(4).
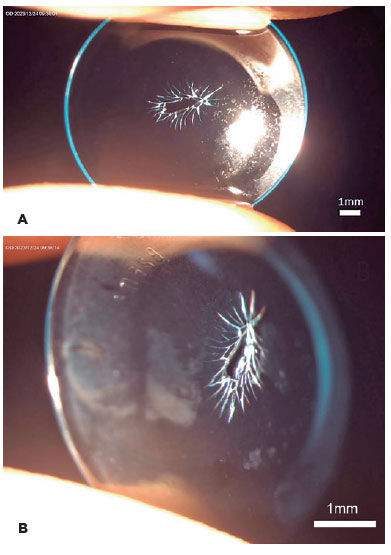
The image shows the significant damage at the center of the orthokeratology lens, with a feathery appearance on the anterior (side A) and lateral (side B) views. The lens features a corneal refractive therapy (CRT) design(5) that is characterized by a treatment curve radius of 8.2 mm, return zone depth of 600 µm, and landing zone angle of 32º.
AUTHOR CONTRIBUTIONS:
Significant contribution to conception and design: Weimin Zhang. Data Acquisition: Shujuan Wang. Data Analysis and Interpretation: Yingcheng Lin. Manuscript Drafting: Min Zhou. Significant intellectual content revision of the manuscript: Min Zhou. Final approval of the submitted manuscript: Weimin Zhang, Min Zhou, Shujuan Wang, Yingcheng Lin. Statistical analysis: Not applicable. Obtaining funding: Not applicable. Supervision of administrative, technical, or material support: Not applicable. Research group leadership: Not applicable.
ACKNOWLEDGMENTS
We thank the patient for granting permission to publish this information.
REFERENCES
1. Jun J, Zhiwen B, Feifu W, Lili L, Fan L. Level of compliance in orthokeratology. Eye Contact Lens. 2018;44(5):330-4.
2. Zhang J, Lu X, Cheng Z, Zou D, Shi W, Wang T. Alterations of conjunctival microbiota associated with orthokeratology lens wearing in myopic children. BMC Microbiol [Internet]. 2023;23(1):397. Available from: https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-023-03042-1
3. Tao Z, Wang J, Zhu M, Lin Z, Zhao J, Tang Y, et al. Does orthokeratology wearing affect the tear quality of children? Front Pediatr [Internet]. 2021;9:773484. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8804288/
4. Wan K, Cheung SW, Wolffsohn JS, Orr JB, Cho P. Role of corneal biomechanical properties in predicting of speed of myopic progression in children wearing orthokeratology lenses or single-vision spectacles. BMJ Open Ophthalmol [Internet]. 2018;3(1):e000204. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6326267/
5. Lu W, Ning R, Diao K, Chen R, Zhou L, Lian Y, et al. Comparison of two main orthokeratology lens designs in efficacy and safety for myopia control. Front Med (Lausanne) [Internet]. 2022;9:798314. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9010613/
Submitted for publication:
April 26, 2024.
Accepted for publication:
May 12, 2024.
Funding: This study received no specific financial support.
Disclosure of potential conflicts of interest: None of the authors have any potential conflicts of interest to disclose.