

Mehmet Can Özen1; Özlen Rodop Özgür2; Seyhan Kocabaş3
DOI: 10.5935/0004-2749.2023-0205
ABSTRACT
Mantle cell lymphoma of the ocular and periorbital regions is extremely rare but should be considered in the differential diagnosis of lesions affecting the periorbital tissues. In this study, we present a rare case of mantle cell lymphoma of the lacrimal sac in a 65-year-old male presenting with a mass in the lacrimal sac region and epiphora. After clinical examinations and imaging studies, the mucocele was misdiagnosed. Considering the unexpected findings during external dacryocystorhinostomy, a frozen biopsy was performed, which confirmed the diagnosis of lymphoma.
Keywords: Lymphoma, mantle cell; Nasolacrimal duct; Neoplasms; Neoplasm staging; Dacryocystorhinostomy; Diagnosis, differential
INTRODUCTION
Lacrimal system tumors are rare, and most have an epithelial origin (90%). Lacrimal sac lymphoma is a nonepithelial tumor that accounts for 6% of all lacrimal sac tumors. Most reported cases involve secondary involvement of systemic lymphoproliferative disease(1).
To date, only three studies on mantle cell lymphoma (MCL) in the lacrimal sac have been published(2-4). In this study, we aimed to present a case that was initially misdiagnosed as mucocele but was diagnosed as lymphoma via frozen biopsy that was performed during external dacryocystorhinostomy (DCR) due to its abnormal structure.
CASE REPORT
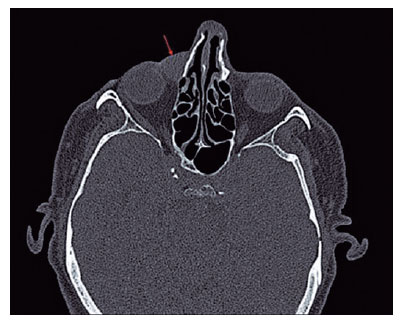
A 65-year-old male complained of epiphora and swelling in the right medial canthal region for approximately 3 months. After reviewing the patient’s medical records, a mass was recorded three months ago, but the lacrimal irrigation was patent. The patient did not undergo further examination. During the examination, a semimotile, nontender mass, measuring approximately 10 × 15 mm, was detected. Diagnostic lacrimal irrigation tests revealed a hard stop an obstruction. The patient’s best-corrected visual acuity was 20/20 in both eyes and the anterior and posterior segments were normal based on biomicroscopic examination. Orbital computed tomography (CT) revealed a well-circumscribed hypodense soft tissue mass in the right medial orbit (18 × 11 mm) that did not spread to the surrounding tissues (Figure 1).
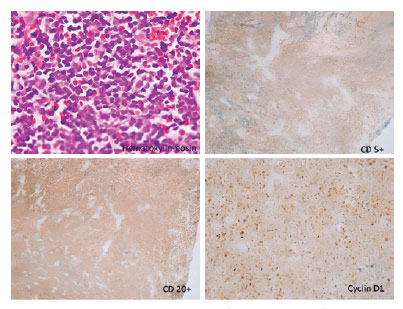
An external DCR was planned. During the surgery, a polypoidal lesion of approximately 2 × 3 mm was observed in the palpebral conjunctiva, and an excisional biopsy was performed on the mass. The lacrimal sac was filled with pink, lobulated tissue. Intraoperative frozen section revealed lymphoid cell proliferation with small round nuclei, absence of nucleoli, and scant cytoplasm with scattered and nodular patterns, which is highly suggestive of lymphoma. To confirm the histopathological results, the lacrimal sac and nasolacrimal duct were completely excised, bicanalicular silicone tube intubation was performed, and the nasal mucosal flap was sutured to subcutaneous tissue.
Histopathological and immunohistochemical findings revealed classical MCL (Figure 2). The patient was referred to the oncology department. Additional tests such as those for liver function, erythrocyte sedimentation rate, blood urea nitrogen level, creatinine level, β2 microglobulin level, lactate dehydrogenase level, leukocyte count, whole-body positron emission tomography (PET) (Figure 3), and bone marrow biopsy were performed.
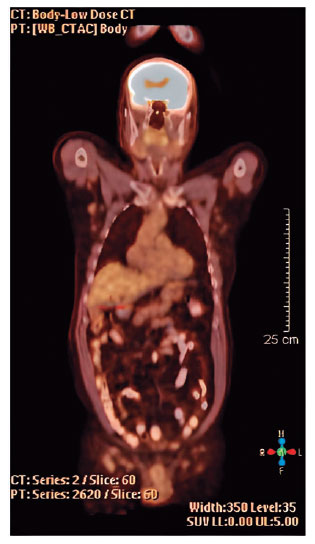
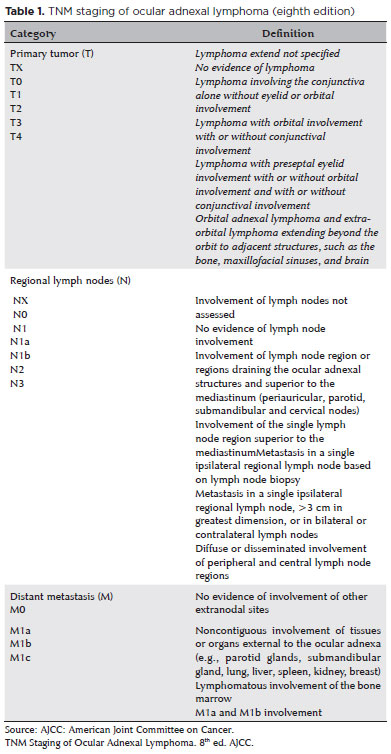
The PET scan revealed multiple lymphadenopathies in the mediastinum, axillary fossa, and infra- and supra-diaphragmatic paraaortic areas. Bone marrow examination revealed involvement of the bone marrow. The patient was classified as having T4N3M1c disease according to the TNM staging system for ocular adnexal lymphoma (Table 1).
The patient was treated with six courses of rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) by the oncology department. Regression of systemic lesions after six cycles of chemotherapy was revealed in a PET re-evaluation. Written informed consent for publication was obtained from the patient.
DISCUSSION
Tumors arising in the lacrimal sac are extremely rare and usually occur during the fifth decade of life. They constitute 2.6% of all lacrimal system obstructions(4,5).
The most common presentation of lacrimal sac lymphomas is similar to that of nontumor cases of lacrimal system obstruction, which is epiphora and painless or painful medial canthal swelling(1,5). In 1956, Jones described the clinical symptoms of lacrimal tumors as epiphora, dacryocystitis, masses, and bleeding(6).
Up to 40% of lacrimal tumors are not suspected via medical examination and are diagnosed during DCR.(2) In our case, the diagnosis was made while performing DCR.
MCL represents only 3%–10% of all no Hodgkin’s lymphomas. It has been reported very rarely in the periocular region. However, periocular involvement is more common in the orbit and eyelids. It is usually observed in men over 60 years of age and is an aggressive tumor. One- to two-thirds of the patients had a history of lymphoma, and for the remainder, the diagnosis was made when the disease was already widespread(2).
In conclusion, malignancy should be considered in the differential diagnosis of patients presenting with a mass in the lacrimal sac region and epiphora. Moreover, rapid imaging and clinical and histopathological tests should be conducted to confirm the diagnosis, and patients should be referred to the oncology department for systemic evaluation and treatment. MCL with secondary involvement of the lacrimal sac is rare and usually has poor prognosis. Furthermore, early diagnosis and patient referral for systemic evaluation and treatment can prolong the survival rates.
REFERENCES
1. Ngah NSI, Ramli RR, Hussein A, Jaafar H. Primary non hodgin’s lymphoma of lacrimal sac presented as recurrent acute dacryocystitis. A case report. J Acute Dis. 2017;6(3):137-40.
2. Rasmussen PK. Diffuse large B-cell lymphoma and mantle cell lymphoma of the ocular adnexal region, and lymphoma of the lacrimal gland: An investigation of clinical and histopathological features. Acta Ophthalmol. 2013;91 Thesis 5:1-27.
3. Cruz AA, Gomes DM, Chahud F. Bilateral mantle cell lymphoma of the lacrimal sac and nasolacrimal duct. JAMA Ophthalmol. 2020;138(12):e202394.
4. Meng FX, Yue H, Yuan YQ, Zhang R, Yuan YF, Bi YW, Qian J. Lacrimal sac lymphoma: a case series and literature review. Int J Ophthalmol. 2022;15(10):1586-90.
5. Coloma-Gonzalez I, Flores-Preciado J, Ceriotto A, Corredor-Cases S, Salcedo-Casillas G. Lacrimal sac tumors presenting as lacrimal obstruction. Retrospective study in Mexican patients 2007-2012. Arch Soc Esp Oftalmol. 2014;89(6):222-5.
6.Jones IS. Tumors of the lacrimal sac. Am J Ophthalmol. 1956; 42:561-6.
AUTHORS’ CONTRIBUTION:
Significant contribution to conception and design: Mehmet Can Özen, Özlen Rodop Özgür. Data acquisition: Mehmet Can Özen, Özlen Rodop Özgür, Seyhan Kocabaş. Data analysis and interpretation: Mehmet Can Özen, Özlen Rodop Özgür. Manuscript drafting: Mehmet Can Özen, Özlen Rodop Özgür. Significant intellectual content revision of the manuscript: Mehmet Can Özen, Özlen Rodop Özgür. Final approval of the submitted manuscript: Mehmet Can Özen, Özlen Rodop Özgür, Seyhan Kocabaş. Statistical analysis: Mehmet Can Özen. Obtaining funding: None. Supervision of administrative, technical, or material support: Mehmet Can Özen. Research group leadership: Mehmet Can Özen, Özlen Rodop Özgür.
Informed consent was obtained from all patients included in this study.
Submitted for publication:
July 13, 2023.
Accepted for publication:
October 31, 2023.
Funding: This study received no specific financial support.
Disclosure of potential conflicts of interest: None of the authors have any potential conflicts of interest to disclose.