

Leonardo Provetti Cunha1,2,3; Luciana Virgínia Ferreira Costa-Cunha2; Carolina Ferreira Costa2; Mário Luiz Ribeiro Monteiro3
DOI: 10.5935/0004-2749.20190099
ABSTRACT
Vitreopapillary traction is an uncommon condition characterized by strong adhesion and the traction of the posterior hyaloid onto the optic disc and peripapillary retina, leading to optic disc elevation and visual loss. An 85-year-old man presented with a 6-month history of slow, progressive visual loss in the left eye along with optic disc edema. Swept-source optical coherence tomography B-scans revealed circumpapillary anterior-posterior persistent traction of dense vitreous strands onto the optic disc. Visual field examination demonstrated mild, generalized, diffuse sensitivity loss and blind-spot enlargement. A 25-gauge posterior vitrectomy was performed with posterior hyaloid separation from the optic disc, resulting in significant anatomical and visual improvement. In conclusion, swept-source optical coherence tomography aids in understanding the mechanism underlying visual loss in vitreopapillary traction. Moreover, posterior vitrectomy can effectively promote anatomical and visual improvements in these cases.
RESUMO
A tração vitreopapilar é uma condição incomum caracterizada por forte adesão e tração da hialoide posterior no disco óptico e retina peripapilar, levando à elevação do disco óptico e à perda visual. Um homem de 85 anos apresentou uma história de 6 meses de perda visual lenta e progressiva no olho esquerdo, juntamente com edema do disco óptico. A tomografia de coerência óptica por fonte de varredura revelou tração persistente ântero-posterior peripapilar com traves vítreas densas sobre o disco óptico. Exame de campo visual demonstrou perda de sensibilidade difusa, generalizada, leve e aumento do ponto cego. Uma vitrectomia posterior de calibre 25 foi realizada com separação hialóide posterior do disco óptico, resultando em melhora anatômica e visual significativa. Em conclusão, a tomografia de coerência óptica por fonte de varredura auxilia na compreensão do mecanismo subjacente à perda visual na síndrome de tração vitreopapilar. Além disso, a vitrectomia posterior pode efetivamente promover melhorias visuais e anatômicas nesses casos.
Descritores: Corpo vítreo; Tomografia de coerência óptica; Papiledema; Membrana epirretiniana; Humanos; Relatos de casos
INTRODUCTION
Vitreopapillary traction (VPT) is a rare and underdiagnosed disease that is characterized by strong adhesion of the posterior hyaloid onto the optic disc and peripapillary area1. This condition can lead to optic disc elevation, often misdiagnosed as optic disc edema, and the distortion of optic disc vessels and peripapillary inner retina, resulting in axonal impairment and visual loss. VPT is caused by an incomplete and anomalous posterior vitreous detachment (PVD).
VPT can be clinically assessed by fundus examination and also using optical coherence tomography (OCT)2. Recent advances in OCT have enabled detailed analyses of the macular and optic disc areas. Particularly, swept-sour ce OCT (SS-OCT) can help in such detailed analyses owing to its higher resolution, deeper penetration, and faster acquisition time. Moreover, SS-OCT is capable of visualizing the retina, choroid, and vitreous in a more detailed manner3. Previous studies have demonstrated the ability of SS-OCT to detect the vitreous interface anomalies4; however, to the best of our knowledge, no studies have described its applicability in VPT. Posterior vitrectomy (PV) for the release of VPT seems to be effective in promoting anatomical and functional improvement; however, till date, only few reports have addressed this issue2,5-7.
Thus, this study aims to describe ultrastructural changes detected using SS-OCT in a case with severe VPT. Moreover, it aims to discuss the possible mechanisms underlying visual loss, in addition to the anatomical and functional improvement after PV.
CASE REPORT
An 85-year-old man presented with progressive vi sual loss in the left eye (OS) since 6 months. Five years ago, he had undergone an uncomplicated cataract surgery in both the eyes (OU).
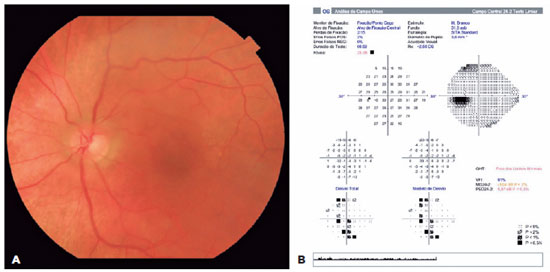
Best corrected visual acuity (VA) was 20/25 in the right eye (OD) and 20/60 in OS. Pupils were equal in size and normally reacted to light and near, with no afferent pupillary defect. Slit-lamp examination revealed no abnormal findings; intraocular lenses were topics with no signs of anterior inflammation or posterior capsule rupture OU. Intraocular pressure was 16 mmHg OU. Fundus examination revealed blurred optic disc margins and circumpapillary posterior vitreous adhesion in a ring shape around the optic disc and a thin macular epiretinal membrane (ERM; Figure 1A). Visual field (VF) examination using the Humphrey 24-2 SITA-Standard protocol showed a mild, generalized diffuse reduction of sensitivity and blind-spot enlargement (Figure 1B).
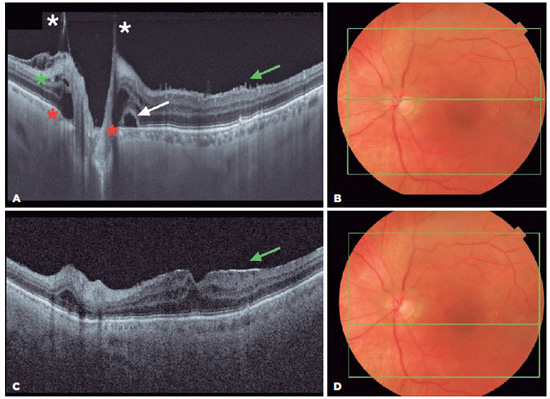
Horizontal SS-OCT (DRI OCT Triton; Topcon, Tokyo, Japan) B-scans passing through the optic disc and macula showed a circumpapillary anterior-posterior persistent traction of dense vitreous strands on the optic disc. Peripapillary inner retinal layers were anteriorly displaced, and cystic spaces in the inner nuclear layer and serous detachment of the retinal pigment epithelium (RPE) were observed (Figure 2). SS-OCT also revealed a thin ERM with mild macular edema.
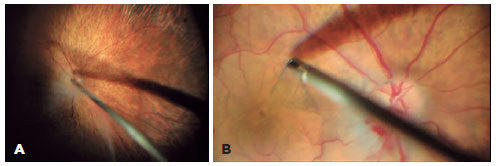
The patient then underwent 25-gauge PV, and the posterior hyaloid was separated from the optic disc by active suction and anterior displacement using a vitrectomy probe. The stained ERM and internal limiting membrane (ILM) was peeled using forceps (Figure 3).
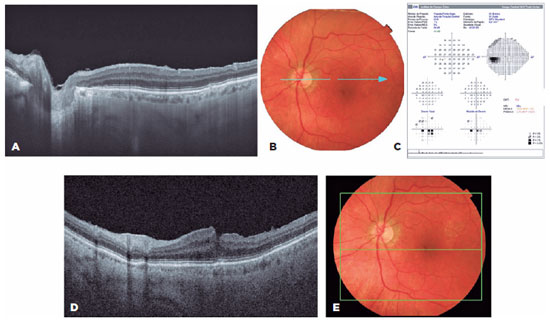
After 1 month, VA was 20/25 OS. SS-OCT B-scans showed the complete release of VPT, the resolution of peripapillary changes, and improved macular edema (Figure 4A) and VF parameters (Figure 4C).
DISCUSSION
Under normal aging conditions, the vitreous tends to detach from the posterior pole, thus increasing the incidence of PVD in elderly people8. However, the attachment of the vitreous to the optic disc margin may persist even if the vitreous is detached elsewhere. Such occurrence can be justified by cellular proliferation from the optic nerve head (ONH) with the formation of an epipapillary membrane. In our cause, we believe that this proliferation was associated with an anomalous PVD, resulting in vitreoschisis, a condition in which the posterior vitreous cortex splits with forward displacement of the anterior cor tex portion, leaving part of the posterior layer of the cor tex attached to the retina. Moreover, the remaining membranes adherent to the optic disc contract, resulting in anteroposterior traction onto ONH.
Transient or permanent visual loss is well recognized in cases of VPT1,2,7,9. Katz and Hoyt9 postulated that optic disc edema results from tension on the vitreopapillary interface from an incomplete PVD and that visual symptoms are caused by traction transmitted from the vitreous to the superficial nerve fibers of the peripapillary retina and optic disc. They further stated that these mechanical deformations of the retinal and optic disc structures could impair the generation and transmission of axonal discharge and block the neuroretinal sign, generating transient gaze-evoked amaurosis. In the present case, persistent adhesion of the posterior hyaloid onto the ONH may have induced mechanical changes, stret ching the optic nerve fiber, peripapillary retina, and the superficial vessels, which can lead to permanent axonal damage, resulting in a mixed model of injury comprising mechanical and ischemic injuries.
In the present case, SS-OCT demonstrated persistent vitreous bands pulling up on the optic disc and also on the peripapillary area, such as traction of the peripapillary retinal nerve fiber layer, cystic spaces within the outer plexiform layer, and serous detachment of RPE. This ultrastructural analysis, with involvement of internal and external retinal layers, may be crucial for understanding the mechanisms underlying visual loss in VPT. To the best of our knowledge, no previous study had demonstrated these specific ultrastructural changes in VPT, particularly with involvement of the outer retina.
Pars plana vitrectomy with the separation of the vitreous adhesion on the optic disc seems to be effective for cases with VPT2,7,10. Our patient demonstrated a significant postoperative visual and anatomical improvement. Moreover, we should consider that peeling of the ERM may have had some role in visual recovery. However, once ERM was subtle, its impact on visual loss definitely was less significant than that of VPT.
In conclusion, VPT syndrome can lead to significant visual loss. SS-OCT helps to understand the mechanism underlying this loss, and PV can be effective in promoting visual and anatomical improvements in these cases.
REFERENCES
1. Katz B, Hoyt WF. Intrapapillary and peripapillary hemorrhage in young patients with incomplete posterior vitreous detachment. Signs of vitreopapillary traction. Ophthalmology. 1995;102(2):349-54.
2. Hedges TR, Flattem NL, Bagga A. Vitreopapillary traction confirmed by optical coherence tomography. Arch Ophthalmol. 2006; 124(2):279-81.
3. Hirata M, Tsujikawa A, Matsumoto A, Hangai M, Ooto S, Yamashiro K, et al. Macular choroidal thickness and volume in normal subjects measured by swept-source optical coherence tomography. Invest Ophthalmol Vis Sci. 2011;52(8):4971-8.
4. Schaal KB, Pang CE, Pozzoni MC, Engelbert M. The premacular bursa's shape revealed in vivo by swept-source optical coherence tomography. Ophthalmology. 2014;121(5):1020-8.
5. De Bustros S, Thompson JT, Michels RG, Rice TA. Vitrectomy for progressive proliferative diabetic retinopathy. Arch Ophthalmol. 1987;105(2):196-9.
6. Small KW, McCuen BW 2nd, de Juan E Jr, Machemer R. Surgical management of retinal traction caused by toxocariasis. Am J Ophthalmol. 1989;108(1):10-4.
7. Meyer CH, Schmidt JC, Mannel S, Kroll P. Functional and anatomical results of vitreopapillary traction after vitrectomy. Acta Ophthalmol Scand. 2007;85(2):221-2.
8. Favre M, Goldmann H. Genesis of posterior vitreus body detachment. Ophthalmologica. 1956;132(2):87-97. German.
9. Katz B, Hoyt WF. Gaze-evoked amaurosis from vitreopapillary traction. Am J Ophthalmol. 2005;139(4):631-7.
10. Karatas M, Ramirez JA, Ophir A. Diabetic vitreopapillary traction and macular oedema. Eye (Lond). 2005;19(6):676-82.
Submitted for publication:
November 1, 2018.
Accepted for publication:
February 5, 2019.
Funding: This study received no specific financial support.
Disclosure of potential conflicts of interest: None of the authors have any potential conflicts of interest to disclose.