

Firdevs Ornek1; Damla Erginturk Acar2; Ugur Acar3
DOI: 10.5935/0004-2749.20180097
ABSTRACT
Purpose: To report demographic features and surgical outcomes of 320 children undergoing external dacryocystorhinostomy for dacryostenosis.
Methods: We performed a retrospective evaluation of the records of patients aged <16 years who underwent external dacryocystorhinostomy. Patient demographic features and success rates of the operations were analyzed from the data records. Children with <12-month follow-up were not enrolled in the study.
Results: We identified 326 operative records of 320 children (162 [50.6%] girls and 158 [49.4%] boys) who underwent external dacryocystorhinostomy with a mean follow-up of 26.03 ± 11.11 months. Overall, we evaluated 116 (35.6%) cases of congenital nasolacrimal duct obstruction. Our series demonstrated a 99.4% success rate for external dacryocystorhinostomy.
Conclusions: External dacryocystorhinostomy in children has a high success rate if performed by an experienced oculoplastic surgeon.
Keywords: Dacryocystorhinostomy; Nasolacrimal duct; Nasal obstruction; Treatment outcome in Humans; Child; Preschool Children; Adolescents
RESUMO
Objetivo: Relatar as características demográficas e os resultados cirúrgicos em 320 crianças submetidas à dacriocistorrinostomia externa para dacrioestenose.
Métodos: Foi realizada uma avaliação dos prontuários de pacientes com idade <16 anos submetidos à cirurgia de dacriocistorrinostomia externa. Características demográficas do paciente e taxa de sucesso das operações foram analisadas a partir dos registros de dados. Crianças com menos de 12 meses de acompanhamento não foram incluídas no estudo.
Resultados: Foram identificados 326 registros operatórios de 320 crianças (162 [50,6%] meninas e 158 [49,4%] meninos) que foram submetidas à dacriocistorrinostomia externa com um seguimento médio de 26,03 ± 11,11 meses. No geral, avaliamos 116 (35,6%) casos de obstrução congênita do ducto nasolacrimal. Nossa série demonstrou uma taxa de sucesso de 99,4% para a dacriocistorrinostomia externa.
Conclusão: A dacriocistorrinostomia externa em crianças tem uma alta taxa de sucesso se for realizada por um cirurgião oculoplástico experiente.
Descritores: Dacriocistorinostomia; Ducto nasolacrimal; Obstrução nasal; Resultado do tratamento em humanos; Criança; Pré-escolar; Adolescente
INTRODUCTION
Dacryostenosis is one of the most common diseases requiring surgical intervention in ophthalmology. It is well known that nasolacrimal duct obstruction (NLDO) is responsible for approximately two-thirds of the dacryostenosis cases in adults(1). In addition, obstructions of the punctum, canaliculus, and common canaliculus frequently occur. Failure of canalization at the distal end of the nasolacrimal duct with a membrane at the valve of Hasner results in congenital NLDO affecting approximately 20% of neonates(2). Nasolacrimal sac compression ensures a high recovery rate within the first 12 months without surgery in most cases(2-4). Children who are refractory to nasolacrimal massage may require probing, silicone tube implantation, or external dacryocystorhinostomy (ext-DCR).
In 1904, Toti described Ext-DCR as a surgical approach for dacryostenosis(5). Success rates were considerably lower (15%) since there was no mucosal flap created with his method. Afterward, in 1920, Dupuy-Dutemps and Bourguet described a modified ext-DCR technique using flaps of the lacrimal sac and nasal mucosa(6). This technique established the basis of the modern ext-DCR procedure in use today.
Patients with dacryostenosis typically present with epiphora, copious discharge, swelling, pain, and redness over the sac and regurgitation of mucopurulent secretion when pressure is applied over the lacrimal sac area(2).
Although many studies(1,7-19) have reported on demographic features and treatment modalities in adult dacryostenosis patients, information regarding children with dacryostenosis is relatively limited(4,20-26). In this study, we aimed to report the demographic features and surgical outcomes of 320 children who were operated for dacryostenosis by an experienced oculoplastic surgeon (F.O.).
METHODS
Ethical committee approval was received from the Review Board of our institution. All local laws and principles of the Declaration of Helsinki were followed throughout the protocols of this retrospective cross-sectional study.
All children aged ≤16 years who underwent ext-DCR with or without bicanalicular silicone tube intubation (BSTI) and were followed-up for a minimum of 12 months were enrolled in the study. Performance of the ext-DCR procedure is described in detail in a previous study(8). In brief, a vertical paranasal skin incision is made approximately 15-mm long. Next, the entire bony surface is exposed, and lateral retraction of the soft structures from the lacrimal fossa is performed using a periosteal elevator, and a large osteotomy is created with a dental drill. The next step is to make the anterior and posterior flaps of the lacrimal sac and nasal mucosa with a no. 11 blade. The posterior and anterior mucosal flaps are sutured using three interrupted 6-0 vicryl sutures. If necessary, BSTI is performed following posterior mucosal flap suturing. Finally, the surgical skin wound is closed with several interrupted 6-0 vicryl sutures.
Demographic features such as age at initial presentation and operation time, sex, laterality, operation type (with or without BSTI), and success rate of the operation were analyzed from the patients’ records. Surgical success was defined as “outcome of the open nasolacrimal irrigation test or negative fluorescein dye disappearance test” with “complete recovery of complaints of epiphora and discharge.”
Statistical analysis
Data analyses were performed using IBM SPSS Statistics for Windows, version 21. All variables are presented as mean ± standard deviation.
RESULTS
Overall, we identified 326 operating records of 320 children who underwent ext-DCR for dacryostenosis with a mean follow-up of 26.03 ± 11.11 months. The demographic features of children who underwent ext-DCR are summarized in table 1.
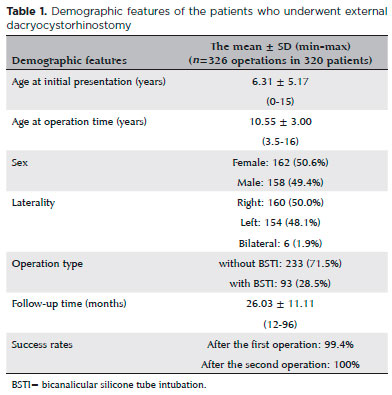
Congenital NLDO occurred in 116 (35.6%) children, whereas 8 (2.5%) had a history of a trauma affecting the lacrimal drainage system. All operations were performed under general anesthesia by the same experienced oculoplastic surgeon (F.O.). Overall, 233 (71.47%) children underwent ext-DCR without BSTI surgery whereas 93 (28.53%) underwent DCR plus BSTI surgery. The mean time of silicone tube removal was 2.51 ± 0.88 months (range, 2-6 months). Recurrence was observed in only two (0.61%) children after surgery. The success rate was 99.4% (324 of 326 operations) after the first operation. The two recurrences developed 3 and 4 months after the first operation, respectively, and both recurrences had a history of trauma 1 year prior to surgery. Both patients underwent DCR plus BSTI as the first operation and silicone tube removal 2 and 3 months after their operation, respectively. Both patients underwent reoperation 4 months after the first operation with a successful surgical outcome. The overall success rate reached 100% following the two operations.
DISCUSSION
The current study retrospectively assessed the demographic characteristics and surgical outcomes of children who underwent ext-DCR with or without BSTI. To the best of our knowledge, this cross-sectional study has the largest sample size among studies in the literature evaluating children who underwent ext-DCR.
Diagnosis of dacryostenosis is more difficult in children compared with adults. The nasolacrimal duct irrigation and fluorescein dye disappearance tests are not easy to perform in children. In order to verify the diagnosis, nasolacrimal duct irrigation is performed at the beginning of every ext-DCR surgery in our institute.
Ophthalmologists have been performing ext-DCR surgery with a high success rate for nearly 100 years following Dupuy-Dutemps and Bourguet’s modified technique. Success rates of ext-DCR are >90% in almost every study in the literature. Woog observed the highest 5-year success rate (100%) in patients with a history of acute dacryocystitis using the conventional DCR technique and the lowest success rate (66.6%) in those who underwent conjunctival DCR with Jones tube placement(1). In his study, 22% of patients with NLDO were admitted to the hospital with acute dacryocystitis.
Different novel surgical techniques are being tested to shorten operating time and further increase the success rate. Sarda et al. claimed that the success rate of ext-DCR was highly associated with proper apposition of the two flaps(8). However, Sharma et al. achieved a 92.9% success rate after 6-month follow-up in 56 patients with primary NLDO by performing anastomosis only between the anterior lacrimal and nasal mucosal flaps with a mean operating time of 36 min(17). Several researchers compared the two different ext-DCR techniques (with and without suturing the posterior mucosal flaps), and they did not find any statistically significant differences between the two procedures(11-17). Furthermore, several studies in the literature indicate a statistically insignificant higher success rate with an easier technique involving excision of the posterior flaps(12-14). Baldeschi et al. demonstrated a 100% success rate with their simplified ext-DCR procedure in 45 patients with dacryostenosis following a mean follow-up of 17 months(10). Anterior flaps of the lacrimal sac and nasal mucosa were easily sutured because they are large and mobile, and posterior flaps were not sutured. Their mean operating time was only 28 min. Caglar et al. evaluated the outcomes of another modified ext-DCR technique in 118 patients with NLDO. They created a U-shaped single anterior flap anastomosis and fixed it to the orbicularis muscle with BSTI(19) reporting success rates of 94.9% and 97.4% following the first and second operations, respectively. All operations were performed using the conventional external technique. Although some surgeons prefer to implant silicone tubes in every dacryostenosis case in order to increase the success rate, we place it in recurrent cases and in those suspected of canalicular stenosis and/or cases with a history of trauma. We do not believe that silicone tube intubation ensures an additional benefit in uncomplicated cases. Silicone tubes were required in 93 (28%) of 326 ext-DCR operations and removed after approximately 2.5 months. If the silicone tubes had been left in place for a longer period, the symptoms would not have recurred. There is no consensus in the literature regarding the duration time of silicone tube placement. Although Shrestha et al. placed silicone tubes in all of their patients and removed them 6 weeks after the operations, their success rate (97%) was not higher than ours(26).
Adult women have a higher incidence of all forms of dacryostenosis than adult men. Although the precise reason for the predisposition of women is unknown, nasolacrimal ducts of women may be more narrow compared with those of men. Woog assessed the demographic features of 587 patients aged >5 years with symptomatic acquired lacrimal outflow obstruction in Olmsted County, Minnesota(1). In this case series, which is the largest sample size in the literature, among 397 patients with NLDO, 73% were female and 27% were male. The data for studies in children with dacryostenosis are controversial. Although sex predisposition was not noted in most of the studies(4,25) of the pediatric age group, Shrestha et al. found that of the 38 children who underwent ext-DCR for dacryostenosis, 61% were female(26). Nowinski et al., Hakin et al., and Barnes et al. identified a male predominance with a ratio of 2:1, 3:2, and 3:2, respectively(21,23,24).
It is well known that patients with Down syndrome have a tendency toward NLDO because of their narrow nasolacrimal ducts and hypertrophic nasal mucosa(27); hence, a simple probing procedure is often unsuccessful in these children(27,28). Our series included one patient with Down syndrome with bilateral NLDO.
The most common reason that children undergo a DCR operation is due to unresolved congenital NLDO. We recommend that parents massage the nasolacrimal sac in their babies with congenital NLDO until 1 year of age because it has a high spontaneous recovery rate. We perform probing at least two times in children who are refractory to medical treatment. If probing fails, silicone tube implantation is performed. Children who are refractory to the above treatment modalities undergo ext-DCR after reaching 3 years of age. Nowinski et al. and Hakin et al. determined that unresolved congenital NLDO was the reason for dacryostenosis in approximately half of the patients in their series(21,23). Welham and Hughes reported a rate of 34.5% in children with congenital NLDO, which is similar to the rate in the present series (35.6%)(24). Other reasons for dacryostenosis in childhood may include punctal/canalicular dysgenesis, lacrimal drainage fistula, and post-inflammatory or post-traumatic lacrimal system obstruction(21-25).
Ext-DCR in children is similar to that in adults. In children, the surgeon should be more attentive to a narrower surgical field. Welham and Hughes achieved a 90% success rate in 142 children who underwent lacrimal drainage surgery(22). Hakin et al. assessed 258 children who underwent ext-DCR(23), achieving a 96% success rate with ext-DCR without canalicular intubation in 177 children who did not have canalicular pathology and a 79% success rate in 70 cases that underwent DCR plus BSTI and 91% in 11 of 81 cases with canalicular pathology that underwent DCR plus Jones tube placement. Nemet et al. assessed 94 cases that underwent ext-DCR, reaching a 93.6% success rate in those undergoing a single operation(25). Moreover, Shrestha et al. evaluated 38 children (aged <15 years) who underwent ext-DCR with BSTI and were followed-up at least 3 months, reporting a 97% success rate(26).Contrary to other studies, Nowinski et al. demonstrated a lower success rate (83%) in the pediatric age group(21). In the present study, we operated on all patients with dacryostenosis using the conventional ext-DCR technique by performing anastomosis of both the anterior and posterior mucosal flaps, and we obtained a 99.4% success rate with a single operation after a mean follow-up of 26 months and a 100% overall success rate following the second operation in two children.
Barnes et al. evaluated 134 ext-DCR operations of 121 children with dacryostenosis(24) with seven (6%) undergoing simultaneous bilateral surgery and reaching a 96% success rate with no remarkable morbidity. However, we do not perform bilateral simultaneous surgery either in children or adults in our institution. Simultaneous bilateral ext-DCR is not preferred, especially in children, because they can be more sensitive to acute blood loss.
One of the limitations of our study is the retrospective nature. In addition, the operating time was not available in the surgical records. Another limitation is the bias probability in evaluating exact surgical success rates of pediatric patients. The pediatric population is difficult to evaluate clinically because of the difficulty in performing reliable nasolacrimal irrigation and fluorescein dye disappearance test. In our clinical practice, we try to perform nasolacrimal irrigation first. If the children or their parents do not allow us to perform it, we instill fluorescein drops into the inferior fornix without disturbing or upsetting the children. Next, we wait 5 min and observe whether the fluorescein disappears. The large sample size and long follow-up are positive aspects of our study. A greater number of patients with a longer follow-up period are needed to participate in controlled and prospective studies in this regard.
REFERENCES
1. Woog JJ. The incidence of symptomatic acquired lacrimal outflow obstruction among residents of Olmsted County, Minnesota, 1976-2000 (an American Ophthalmological Society thesis) Trans Am Ophthalmol Soc. 2007;105:649-66.
2. Kanski JJ, Bowling B. Clinical ophthalmology: a systematic approach. 7th ed. Philadelphia: Elsevier; 2011. p 56-78.
3. Gioacchini FM, Alicandri-Ciufelli M, Kaleci S, Re M. The outcomes of endoscopic dacryocystorhinostomy in children: A systematic review. Int J Pediatr Otorhinolaryngol. 2015;79(7):947-52.
4. Noda S, Hayasaka S, Setogawa T. Congenital nasolacrimal duct obstruction in Japanese infants: its incidence and treatment with massage. J Pediatr Ophthalmol Strabismus. 1991;28(1):20-2.
5. Toti A. [New radical cure conservative approach of chronic suppurations of the lacrimal sac (Dacryocystorhinostomy)]. Clin Mod Firenze 1904;10:385. Italian.
6. Dupuy-Dutemps MM, Bouguet ET. [Preliminary note on a dacryocystorhinostomy process]. Ann Ocul (Paris) 1920;157:445-7. French.
7. Stallard HB. Eye Surgery. 3rd ed. Bristol: Wright; 1958.
8. Sarda RP, Kulshrestha OP, Mathur RN. Dacryocystorhinostomy. Br J Ophthalmol. 1961;45(2):138-43.
9. Bolger WE, Parsons DS, Mair EA, Kuhn FA. Lacrimal drainage system injury in functional endoscopic sinus surgery. Incidence, analysis, and prevention. Arch Otolaryngol Head Neck Surg. 1992; 118(11):1179-84.
10. Baldeschi L, Nardi M, Hintschich CR, Koornneef L. Anterior suspended flaps: A modified approach for external dacryocystorhinostomy. Br J Ophthalmol. 1998;82(7):790-2.
11. Dareshani S, Niazi JH, Saeed M, Memon MS, Mehmood T. Dacryocystorhinostomy: Importance of anastomosis between anterior and posterior flaps. Pak J Ophthalmol. 1996;12(1):129-31.
12. Elwan S. A randomized study comparing DCR with and without excision of the posterior mucosal flap. Orbit. 2003;22(1):7-13. Comment in: Orbit. 2003;22(4):321; author reply 323.
13. Serin D, Alagoz G, Karsloglu S, Celebi S, Kükner S. External dacryocystorhinostomy: Double-flap anastomosis or excision of the posterior flaps? Ophthal Plast Reconstr Surg. 2007;23(1):28-31.
14. Kacaniku G, Begolli I. External dacryocystorhinostomy with and without suturing the posterior mucosal flaps. Med Arch. 2014; 68(1):54-6.
15. Khan FA, Yaqub MA, Fayyaz M. The importance of excising or suturing the posterior mucosal flaps in external dacryocystorhinostomy. Pak J Ophthalmol. 2010;26((1):69-73.
16. Katuwal S, Aujla JS, Limbu B, Saiju R, Ruit S. External dacryocystorhinostomy: do we really need to repair the posterior flap? Orbit. 2013;32(2):102-6.
17. Sharma HR, Sharma AK, Sharma R. Modified external dacryocystorhinostomy in primary acquired nasolacrimal duct obstruction. J Clin Diagn Res. 2015;9(10):NC01-5.
18. Ozer S, Ozer PA. Endoscopic vs external dacryocystorhinostomy-comparison from the patients’ aspect. Int J Ophthalmol. 2014; 7(4):689-96.
19. Caglar C, Yener HI, Gul A, Ozcimen M. The modified technique of external dacryocystorhinostomy in the management of complicated nasolacrimal duct obstruction. J Craniofac Surg. 2016;27(2): 416-9.
20. Guerry D 3rd, Kendig EL Jr. Occluded nasolacrimal ducts in infants. AMA Arch Ophthalmol. 1950;44(4):600-1.
21. Nowinski TS, Flanagan JC, Mauriello J. Pediatric dacryocystorhinostomy. Arch Ophthalmol. 1985;103(8):1226-8.
22. Welham RA, Hughes SM. Lacrimal surgery in children. AmJ Ophthalmol. 1985;99(1):27-34.
23. Hakin KN, Sullivan TJ, Sharma A, Welham RA. Pediatric dacryocystorhinostomy. Aust N Z J Ophthalmol. 1994;22(4):231-5.
24. Barnes EA, Abou-Rayyah Y, Rose GE. Pediatric dacryocystorhinostomy for nasolacrimal duct obstruction. Ophthalmology 2001;108(9):1562-4. Comment in: Ophthalmology. 2002;109(9):1587-8; author reply 1588.
25. Nemet AY, Fung A, Martin PA, Benger R, Kourt G, Danks JJ, et al. Lacrimal drainage obstruction and dacryocystorhinostomy in children. Eye (Lond). 2008;22(7):918-24.
26. Shrestha R, Sobti D, Chi SL, Saiju R, Richard M. Surgical outcome of pediatric dacryocystorhinostomy in Nepal. J AAPOS. 2014;18(4): 368-9.
27. Baran F, Kelly JP, Finn LS, Manning S, Herlihy E, Weiss AH. Evaluation and treatment of failed nasolacrimal duct probing in Down syndrome. J AAPOS. 2014;18(3):226-31.
28. Lueder GT. Treatment of nasolacrimal duct obstruction in children with trisomy 21. J AAPOS. 2000;4(4):230-2.
Submitted for publication:
February 6, 2018.
Accepted for publication:
April 10, 2018.
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflicts of interest to disclose
Approved by the following research ethics committee: Ankara Training and Research Hospital (#633/2016)