

Andreia Soares; Fernando Faria-Correia; Nuno Franqueira; Sara Ribeiro
DOI: 10.5935/0004-2749.20180094
ABSTRACT
Purpose: To evaluate the effect of superior blepharoplasty on the tear film using the corneal topographer Keratograph 5M.
Methods: A prospective study was performed of 27 eyes of 14 patients with superior dermatochalasis who underwent superior blepharoplasty between May and June 2016. Conservative upper eyelid blepharoplasty was performed by an en bloc resection of anterior lamellar tissue that included skin, subcutaneous tissue, and the orbicularis oculi muscle. All the eyes were imaged using the noninvasive tear breakup time tools of the Keratograph 5M. The following parameters were recorded in each patient before and 6 weeks after surgery: first noninvasive Keratograph 5M tear breakup time (the time at which the first breakup of tears occurs) and average noninvasive Keratograph 5M tear breakup time (the average time of all breakup incidents). The exclusion criteria were ophthalmological pathology, previous eyelid surgery, use of eye drops, systemic pathology, and medication that interferes with lacrimal tears.
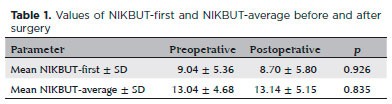
Results: The mean age of the patients was 65.1 years (range, 51-84); 86% were female. Student’s t-test was used to compare the values of first and average noninvasive Keratograph 5M tear breakup times before and after surgery. The values for first noninvasive Keratograph 5M tear breakup time evaluated before and after surgery were not significantly different (9.04 and 8.71, respectively; p=0.926). The values for average noninvasive Keratograph 5M tear breakup time evaluated before and after surgery were also not significantly different (13.01 seconds and 13.14 seconds, respectively; p=0.835).
Conclusions: The results of this pilot study suggest that upper blepharoplasty does not affect tear breakup time according to the objective evaluation of breakup time with the Keratograph 5M.
Keywords: Blepharoplasty; Dry eye syndrome; Tears; Optometry/ instrumentation
RESUMO
Objetivos: Avaliar o efeito da blefaroplastia superior no filme lacrimal, utilizando o topógrafo de córnea Keratograph 5M.
Métodos: Foi realizado estudo prospectivo de 27 olhos de 14 pacientes com dermatocálase superior submetidos à blefaroplastia superior entre maio e junho de 2016. A blefaroplastia palpebral superior conservadora foi realizada por ressecção em bloco de tecido lamelar anterior que incluiu pele, tecido subcutâneo e músculo orbicular do olho. Todos os olhos foram fotografados usando as ferramentas não-invasivas de tempo de ruptura do lacrimal do Keratograph 5M. Os seguintes parâmetros foram registrados em cada paciente antes e 6 semanas após a cirurgia: primeiro tempo não-invasivo de ruptura lacrimal de Keratograph 5M (o tempo em que ocorre o primeiro rompimento dos rasgos) e média não-invasiva do tempo de ruptura lacrimal (tempo médio de todos os incidentes de ruptura). Os critérios de exclusão foram: patologia oftalmológica, cirurgia anterior das pálpebras, uso de colírio, patologia sistêmica e medicação que interfere na ruptura lacrimal.
Resultados: A idade média de idade dos pacientes foi de 65,1 anos (variação entre 51-84); 86% eram do sexo feminino. O teste t de Student foi usado para comparar os valores não-invasivos do tempo de ruptura lacrimal do Keratograph 5M e do tempo de ruptura lacrimal não invasivo do mesmo antes e após a cirurgia. Os valores não-invasivos do tempo de ruptura lacrimal do Keratograph 5M avaliados antes e após a cirurgia não foram significativamente diferentes (9,04 e 8,71, respectivamente; p=0,926). Os valores do tempo médio de ruptura lacrimal do Keratograph 5M avaliados antes e após a cirurgia, também não foram significativamente diferentes (13,01 e 13,14 segundos, respectivamente; p=0,835).
Conclusão: Os resultados deste estudo piloto sugerem que a blefaroplastia superior não afeta o tempo de ruptura lacrimal de acordo com a avaliação objetiva do tempo de ruptura com o Keratograph 5M.
Descritores: Blefaroplastia; Síndromes do olho seco; Lágrimas; Optometria/instrumentação
INTRODUCTION
Superior dermatochalasis is defined as excessive folds of anterior lamellar tissue in the upper eyelids. The etiology can be involutional, familial, or both. Patients complain about difficulty in eyelid elevation, superior visual field reduction, and periorbital discomfort due to excessive use of the frontal and orbicular muscles(1). The method of choice to restore the cosmetic appearance and function of the eyelid is superior blepharoplasty. This surgery can produce changes in the palpebral fissure and can modify ocular physiology, resulting in dry eye syndrome(1,2). Some studies have analyzed the effect of this surgery on lacrimal function(1).
Conventional quantitative evaluation methods are measurement of tear breakup time (TBUT) and the Schirmer test. Conventional TBUT, first introduced in 1969, remains the most frequently used diagnostic test for dry eye syndrome. The fluorescein used in TBUT stimulates reflex tearing, thus, reducing the stability of the tear film. This limitation led to the development of new noninvasive methods that avoid the problems of conventional TBUT. The Schirmer test measures the quantity of tear secretion. The use of dyes such as rose Bengal and lissamine green allows the visualization of changes in the ocular surface. New techniques such as videotopography and meniscometry depend on subjective evaluation by the examiner(1,3-6).
The Keratograph 5M enables noninvasive measurements of the first TBUT (NIKBUT-first) and the average time of all breakup incidents (NIKBUT-average). In addition, it provides a tear map showing the locations and sizes of the tear-break regions(3,7-9). The purpose of this study was to evaluate the effect of superior blepharoplasty on tear film with the use of the Keratograph 5M.
METHODS
This was a prospective study of 27 eyes of 14 patients with superior dermatochalasis who underwent superior blepharoplasty in the Ophthalmology Department of the Hospital de Braga, Portugal, between May and July 2016. The patients had superior dermatochalasis, with no prolapsed fat and well-positioned lacrimal glands. No inferior dermatochalasis was diagnosed in the study group. The exclusion criteria were the presence of ophthalmological pathologies, previous eyelid surgery, use of eye drops, and the presence of other systemic pathologies or medications that affect the tear film. The surgical plan was en bloc resection of the anterior lamellar tissues (skin, subcutaneous tissue, and a small amount of preseptal orbicular muscle).
The patients were instructed to apply cold compresses to the eyes for 2 days after surgery and to use an ointment containing chloramphenicol (10 mg/g) and dexamethasone (2.5 mg/g) two times per day for one month. The eyelid swelling resolved during the first 6 weeks after the procedure. All the surgeries were performed by the same surgeon, and there were no complications. There were no hypercorrections or dry eye symptoms after surgery.
The patients underwent a complete ophthalmological examination before and 6 weeks after surgery, with slit-lamp evaluation, searching for signs of dry eye. At the time of these examinations, objective noninvasive examination of the tear film was performed with the use of the Keratograph 5M. To avoid the effect of fluorescein on the tear film, the evaluations with the Keratograph 5M were performed before the conventional ophthalmological examinations.
The patients were seated at the Keratograph 5M in a darkened room. After three or four blinks, the patient was asked to keep his or her eyes open as long as possible and to focus on a central target. The reflected projection surface was observed closely. Irregularities in the reflected image indicated places on the cornea where the tear film was losing stability or breaking up. The Keratograph 5M provides a tear map showing the locations and sizes of the tear-break regions and generates two measures of NIKBUT: the time when the first breakup of tear film occurs, which is the time between the last complete blink and the first perturbation of the Placido rings projected onto the surface of the cornea (NIKBUT-first), and the average time of all breakup incidents (NIKBUT-average).
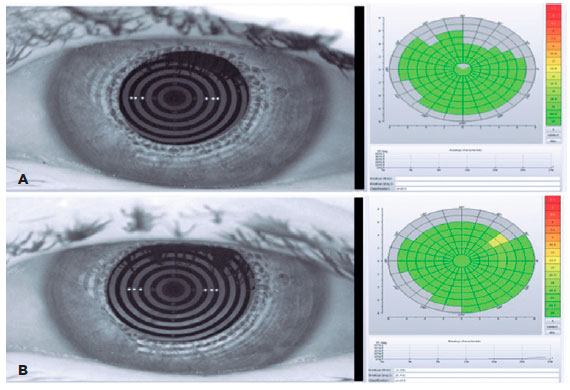
Figure 1 shows a representative output of NIKBUT. The tear film assessment software divides the 360o ocular surface into 24 bands and subdivides each band into eight small rectangles (with longitude numbers 1-8), each of which serves as a basic breakup unit. The color of the unit in a particular location represents the TBUT of this unit, which changes in color from red to yellow to green as TBUT increases.
Each eye was evaluated three times for 5 minutes at a time. All the measurements were performed by the same trained ophthalmologist.
RESULTS
The study included 27 eyes of 14 patients (12 women and 2 men), with a mean age of 65.1 years (range, 51-84). Table 1 shows the mean values of NIKBUT-first and NIKBUT-average before and after surgery obtained with the Keratograph 5M. Student’s t-test was performed to compare the means of NIKBUT-first and NIKBUT-average before and after surgery. The mean values of NIKBUT-first before and after surgery were 9.04 ± 5.36 and 8.70 ± 5.80, respectively. The mean values of NIKBUT-average before and after surgery were 13.04 ± 4.68 and 13.14 ± 5.15, respectively. There were no significant differences between the values before and after surgery (Table 1). Figure 1 shows the output of the Keratograph 5M before and after blepharoplasty, and figure 2 shows photographs of the patient before and after blepharoplasty. The patients were evaluated before and after surgery with slit-lamp examination, and there were no signs of keratitis or other signs of dry eye.

DISCUSSION
Dry eye syndrome is a disease that can be associated with excessive evaporation or a deficit in tear production, resulting in ocular surface lesions in the palpebral fissure(4). No exact correlations have been described between blepharoplasty and changes in conventional examination of tear films (TBUT and Schirmer test)(4).
Previous studies have shown that some anatomical characteristics of the orbital and periorbital structures, such as proptosis, sagging of the lower eyelid, malar hypoplasia, and presence of visible sclera, are associated with dry eye syndrome after blepharoplasty(1,10). Our study found no patients with these characteristics.
Our results are in agreement with those obtained with conventional tear film evaluation after blepharoplasty in a previous study. This study concluded that there were no significant changes in TBUT and Schirmer test values after surgery(4). However, our results disagree with those of other studies that report an increased incidence of dry eye syndrome after blepharoplasty(2,10). Perhaps this difference is related to different characteristics of the patients in these studies that make them more susceptible to complications. This is the first study to analyze lacrimal function in patients undergoing blepharoplasty with the use of the Keratograph 5M, which produces objective and noninvasive (not fluorescein-dependent) data. The parameters evaluated with this instrument (NIKBUT-first and NIKBUT-average) did not show statistically significant changes after surgery.
This study has some limitations, such as the very small number of patients included and the absence of interpalpebral fissure evaluation before and after the procedure. Conventional tests for assessment of lacrimal unit function, such as the Schirmer test, were not performed.
In conclusion, objective and noninvasive evaluation of TBUT with the Keratograph 5M shows that superior blepharoplasty does not affect the tear film.
REFERENCES
1. Lima CG, Siqueira GB, Cardoso IH, Sant’Anna AE, Osaki MH. [Evaluation of dry eye in before and after blepharoplasty]. Arq Bras Oftalmol. 2006;69(2):227-32. Portuguese.
2. Abell KM, Cowen DE, Baker RS, Porter JD. Eyelid kinematics following blepharoplasty. Ophthal Plast Reconstr Surg. 1999;15(4):236-42.
3. Abdelfattah NS, Dastiridou A, Sadda RS, Lee OL. Noninvasive imaging of tear film dynamics in eyes with ocular surface disease. Cornea. 2015;34(Suppl 10):S48-52.
4. Floegel I, Horwath-Winter J, Muellner K, Haller-Schober EM. A conservative blepharoplasty may be a means of alleviating dry eye symptoms. Acta Ophthalmol Scand. 2003;81(3):230-2.
5. Jiang Y, Ye H, Xu J, Lu Y. Noninvasive keratograph assessment of tear film break-up time and location in patients with age-related cataracts and dry eye syndrome. J Int Med Res. 2014;42(2):494-502.
6. Sweeney DF, Millar TJ, Raju SR. Tear film stability: a review. Exp Eye Res. 2013;117:28-38.
7. Best N, Drury L, Wolffsohn JS. Clinical evaluation of the Oculus Keratograph. Cont Lens Anterior Eye. 2012;35(4):171-4.
8. Bhandari V, Reddy JK, Relekar K, Ingawale A, Shah N. Non-invasive assessment of tear film stability with a novel corneal topographer in Indian subjects. Int Ophthalmol. 2016;36(6):781-90.
9. Tian L, Qu j, Zhang X, Sun X. Repeatability and reproducibility of noninvasive keratograph 5m measurements in patients with dry eye disease. J Ophthalmol. 2016; 2016:8013621.
10. Lessa SF, Elena EH, Araújo MR, Pitanguy I. Modificações anatómicas da fenda palpebral após blefaroplastia. Rev Bras Cir. 1997;87(4): 179-88.
Submitted for publication:
December 1, 2017.
Accepted for publication:
March 13, 2018.
Funding: No specific financial support was provided for this study.
Disclosure of potential conflicts of interest: None of the authors have any potential conflicts of interest to disclose
Approved by the following research ethics committee: Hospital de Braga (# 057/2016)