

Burak Bilgin1; Ayse Sevgi Karadag2
DOI: 10.5935/0004-2749.20180093
ABSTRACT
Purpose: This study reports the effects of combined use of oral doxycycline and topical cyclosporine on ocular signs, symptoms, and tear film parameters in rosacea patients.
Methods: Fifty-four right eyes of 54 patients were included in this study. All patients underwent full ophthalmologic examination-including best corrected visual acuity measurement, slit-lamp anterior segment and fundus examination, tear film break-up time, and Schirmer test-before treatment and six months post-treatment. Patients were divided into two treatment groups. The first group was treated with oral doxycycline 100 mg twice daily for the first month and once daily for the following two months. The second group received topical 0.05% cyclosporine emulsion drops twice daily for six months in addition to the oral doxycycline treatment regimen. All patients received preservative-free artificial tear drops, warm compress, eyelash cleaning, and topical corticosteroid drops three times daily for one month.
Results: A significant improvement in ocular signs and symptoms was recorded for all patients in groups 1 and 2 after treatment. There was not a significant difference in terms of itching, burning, meibomian gland inspissation, corneal neovascularization, and conjunctival hyperemia score changes between groups 1 and 2. The increases in Schirmer test and break-up time scores were significantly higher in group 2 than in group 1.
Conclusions: Our results support the finding that topical cyclosporine in addition to the standard regimen improves tear function, as shown by Schirmer test and break-up time scores, in ocular rosacea patients.
Keywords: Rosacea/drug therapy; Tears; Doxycycline/therapeutic use; Cyclosporine/therapeutic use; Administration, oral; Drug therapy, combination
RESUMO
Objetivo: Este estudo relata os efeitos do uso combinado de doxiciclina oral e ciclosporina tópica sobre sinais e sintomas oculares e sobre parâmetros do filme lacrimal em pacientes com rosácea.
Métodos: Cinquenta e quatro olhos direitos de 54 pacientes foram incluídos no estudo. Todos os pacientes foram submetidos a exame oftalmológico completo - incluindo a melhor medida da acuidade visual corrigida, segmento anterior em lâmpada de fenda e exame de fundo de olho, tempo de ruptura do filme lacrimal e teste de Schirmer - antes do tratamento e após seis meses de tratamento. O primeiro grupo foi tratado com doxiciclina oral 100 mg duas vezes ao dia no primeiro mês e uma vez ao dia nos dois meses seguintes. O segundo grupo recebeu gotas tópicas de emulsão de ciclosporina a 0,05% duas vezes ao dia por seis meses, além do tratamento com doxiciclina por via oral. Todos os pacientes receberam gotas de lágrima artificial sem conservantes, compressas mormas, limpeza de cílios e gotas de corticosteróide tópico três vezes ao dia durante um mês.
Resultados: Uma melhora significativa nos sinais e sintomas oculares foi registrada para todos os pacientes do grupo 1 e 2 após o tratamento. Não houve diferença significativa em termos de prurido, queimação, inspeção da glândula meibomiana, neovascularização da córnea e alterações na pontuação da hiperemia conjuntival entre os grupos 1 e 2. O teste de Schirmer e o aumento do tempo de ruptura no grupo 2 foram significativamente maiores do que no grupo 1.
Conclusões: Os autores concluíram que os resultados apoiam a descoberta de que a ciclosporina tópica, além do tratamento padrão, melhora a função lacrimal como demonstrado pelo teste de Schirmer e o tempo de ruptura em pacientes com rosácea ocular.
Descritores: Rosácea/quimioterapia; Lágrimas; Doxiciclina/uso terapêutico; Cilosporina/uso terapêutico; Admınıstração oral; Quimioterapia combinada
INTRODUCTION
Rosacea is a chronic inflammatory disease primarily affecting blood vessels and sebaceous glands in the central facial skin. While the clinical presentation and severity of the disease may vary, the most common clinical features are recurrent erythema, telangiectasias, papules, and pustules(1-5). Rosacea typically affects the skin, but about 58%-72% of patients develop ocular manifestations caused by eyelid and ocular surface inflammation(5). Ocular symptoms are present prior to dermatological symptoms in 20% of rosacea patients(3-5). Signs of ocular rosacea may range from foreign body sensation, light sensitivity, dryness, itching, burning, and similar minor irritations to severe corneal vascularization and ulcerations that may eventually cause loss of vision(1,6-8). The precise etiology of rosacea remains unknown, although there is evidence of immune system dysfunction, genetic predisposition, sunlight, vascular anomalies, and parasitic infestations as potential causative factors(4,5). Rosacea most commonly affects individuals between the ages of 40 and 59 years old(9) and is rarely found in pediatric populations(10-12). Although rosacea is a common disease, it is underdiagnosed in clinical practice(13). Possible reasons for this underdiagnosis are that patients with mild symptoms do not complain about the disease, patients with skin symptoms may not mention ocular symptoms in dermatology clinics, and patients with ocular symptoms are not examined for skin manifestations in ophthalmology clinics(5). A multidisciplinary approach involving dermatological and opthamological assessment is thus crucial for early diagnosis and adequate treatment of rosacea. Due to the chronic nature of rosacea, the various treatments are often only satisfactory for ocular symptoms and do not cure the disease. Eyelid hygiene, lubricating agents, topical steroids, antibiotic eye drops, oral tetracyclines, and topical use of cyclosporine drops are some of the most common treatment methods for ocular rosacea symptoms(7,8,14-17). The efficacy of oral doxycycline and topical cyclosporine treatment in the management of ocular rosacea have been reported in the literature(18-24). Studies comparing oral doxycycline and topical cyclosporine treatments for ocular rosacea are also available(25). However, combination treatment strategies have not been assessed. In this study, we aimed to examine the effects of combined use of oral doxycycline and topical cyclosporine on ocular signs, symptoms, and tear film parameters in rosacea patients.
METHODS
This retrospective study was carried out at an ophthalmology department at a tertiary hospital. All procedures complied with the guidelines of the Declaration of Helsinki and written informed consent was obtained from all patients. The study was approved by the Adıyaman University (# 2018/2-27).
The records of 54 patients with ocular rosacea who attended our ophthalmology department between 2013 and 2016 were retrospectively analyzed. Fifty-four right eyes of 54 patients were included in the study. The only inclusion criterion was a diagnosis of ocular rosacea based on signs and symptoms stated by the American National Rosacea Society Expert Committee(26). Exclusion criteria were: any active infection or inflammation of the eye; systemic diseases such as diabetes; rheumatologic and auto-immune eye diseases; allergic conjunctivitis; eyelid deformity or abnormal eyelid movement disorder; contact lens wear; history of ocular surgery within the past six months; history of smoking; and use of medications that may affect ocular tear film quality. At each visit, the patients underwent a full ophthalmologic examination performed in the following order: best corrected visual acuity measurement; slit-lamp anterior segment and fundus examination; tear film break-up time (BUT); and Schirmer test. BUT was measured after instillation of a drop of 2% fluorescein solution under the cobalt blue filter of the biomicroscope. After blinking a few times to stabilize the tear film, the time taken from the last blink to the appearance of the first dry spot on the corneal surface was recorded using a stopwatch. The Schirmer test was performed with a drop of topical anesthetic agent (0.5% proparacaine hydrochloride, Alcaine, Alcon Inc., Forth Worth, TX, USA) by placing a standard paper strip on the temporal side of the lower fornix. After 5 min, the amount of wetness of the paper strip was measured in millimeters and recorded. Itching, burning, and conjunctival hyperemia were scored on a scale from 0 to 4 based on severity. Corneal neovascularization was scored 0-4 considering the quadrants of neovascularization. To assess obstruction of the meibomian gland orifices, digital pressure was applied to the lower tarsus and the quality of the meibum was scored. Patients were divided into two treatment groups. The first group was treated with oral doxycycline 100 mg twice daily for the first month and once daily for the following two months. The second group received topical 0.05% cyclosporine emulsion drops (Restasis, Allergan Inc., Irvine, CA, USA) twice daily for six months in addition to the oral doxycycline treatment regimen same as the first group. All patients received preservative-free artificial tear drops (Tears Naturale Free, Alcon Inc., Forth Worth, TX, USA), warm compress, eyelash cleaning, and topical corticosteroid drops (loteprednol etabonate, Lotemax, Bausch-Lomb Inc., FL, USA) three times daily for one month. The patients’ symptoms and signs were recorded prior to treatment and six months post-treatment and were scored from 0 to 4 points on the panel shown in table 1. The panel included itching, burning, meibomian gland inspissation, corneal neovascularization, and conjunctival hyperemia. A decrease in the score after treatment indicated improvement in symptoms and signs.
The normality of the distributions of quantitative variables of each parameter before and after treatment was assessed by the Shapiro-Wilk test. As the distributions were significantly different from normal distributions, non-parametric tests were used for the statistical analyses. The Wilcoxon signed-rank test was used to evaluate the variables before and after treatment. The Mann-Whitney U-test was used to compare changes in variables between groups. A p-value lower than 0.05 was considered statistically significant.
RESULTS
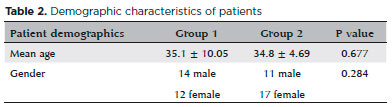
Fifty-four right eyes of 54 patients (29 women, 25 men) with a mean age of 34.96 ± 7.67 years were included in this study. The first group consisted of 26 patients (12 women, 14 men) and the second group consisted of 28 patients (17 women, 11 men). The mean age of the first and second groups was 35.1 ± 10.05 and 34.8 ± 4.69, respectively. The groups were not significantly different in terms of sex and age. The demographic characteristics are presented in table 2.
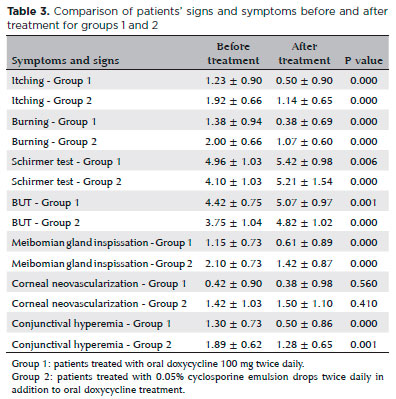
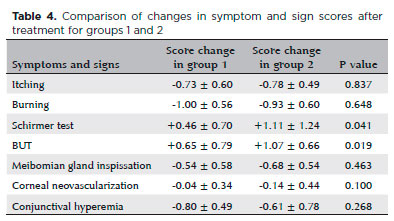
After treatment, significant improvement in ocular signs and symptoms was recorded for all patients in groups 1 and 2. Patients’ mean scores before and after treatment are presented in table 3. There was not a statistically significant difference between group 1 and 2 in terms of itching, burning, meibomian gland inspissation, corneal neovascularization, and conjunctival hyperemia score changes. The Schirmer test and BUT increase in group 2 were significantly higher than in group 1. Comparisons of changes in symptoms and signs between groups 1 and 2 after treatment are shown in table 4.
DISCUSSION
Rosacea is a chronic inflammatory disease characterized by recurrent erythema, telangiectasias, papules, and pustules and may also include ocular symptoms(1-5). In this study, instead of comparing oral doxycycline and topical cyclosporine treatments, we aimed to show benefits of topical cyclosporine drops in combination with an oral doxycycline treatment regimen.
Tetracyclines have been used for a long time in the treatment of rosacea and were approved by the US Food and Drug Administration in 2006 for this purpose(23,24). It has been shown that doxycycline has fewer adverse effects than other tetracyclines(15). Doxycycline is an antibiotic agent, but its anti-inflammatory and anti-angiogenic effects make it stand out from the other tetracyclines. Its effects on neutrophil chemotaxis, lymphocyte proliferation, and matrix metalloproteinase activity have been shown in several studies(17,27). Since doxycycline is highly lipophilic it easily penetrates tissue such as eyelid skin(28). The use of doxycycline in rosacea treatment aims to improve signs and symptoms caused by pathophysiological mechanisms that are not fully understood.
In our study, the second group received 0.05% topical cyclosporine drops in addition to oral doxycycline treatment. Cyclosporine is an immunosuppressive agent that inhibits T lymphocytes(29). Topical cyclosporine A has anti-inflammatory effects and has been successfully used for the treatment of meibomitis and dry eyes in rosacea cases(16,29). A significant improvement in ocular signs and symptoms was shown for both groups after treatment, and the efficacy of the two treatments was comparable except for the Schirmer test and BUT results. The increase in Schirmer test and BUT scores in group 2 was significantly higher than in group 1, which is in accordance with the literature(9,29,30). Dry eyes in ocular rosacea is caused by meibomian gland dysfunction due to meibomitis(1,30). Topical cyclosporine A prevents inflammation of the meibomian glands by inhibiting active T lymphocytes and increasing tear production. Thus, it has a two-fold effect by reducing evaporation as well as increasing tear production.
The limitations of this study should be noted. Due to its retrospective nature, in this study we were unable to perform further tests including tear osmolality measurement and meibography and goblet cell density evaluation.
In summary, our results suggest that topical cyclosporine in addition to the standard regimen improves tear function, as shown by Schirmer test and BUT scores, in ocular rosacea patients. Prospective studies that include additional tests may contribute further information to the literature on ocular rosacea.
REFERENCES
1. Vieira AC, Hofling-Lima AL, Mannis MJ. Ocular rosacea: a review. Arq Bras Oftalmol. 2012;75(5):363-9.
2. Buechner SA. Rosacea: an update. Dermatology. 2005;210(2):100-8.
3. Stone DU, Chodosh J. Ocular rosacea: an update on pathogenesis and therapy. Curr Opin Ophthalmol. 2004;15(6):499-502.
4. Crawford GH, Pelle MT, James WD. Rosacea: I. Etiology, pathogenesis and subtype classification. J Am Acad Dermatol 2004;51(3): 327-41; quiz 342-4.
5. Ghanem VC, Mehra N, Wong S, Mannis MJ. The prevalence of ocular signs in acne rosacea: comparing patients from ophthalmology and dermatology clinics. Cornea. 2003;22(3):230-3.
6. Starr PA, McDonald A. Oculocutaneous aspects of rosacea. Proc R Soc Med. 1969;62(1):9-11.
7. Akpek EK, Merchant A, Pinar V, Foster CS. Ocular rosacea: patient characteristics and follow-up. Ophthalmology. 1997;104(11):1863-7.
8. Fallen RS, Gooderham M. Rosacea: update on management and emerging therapies. Skin Therapy Lett. 2012;17(10):1-4.
9. Spoendlin J, Voegel JJ, Jick SS, Meier CR. A study on the epidemiology of rosacea in the U.K. Br J Dermatol. 2012;167(3):598-605.
10. Oltz M, Check J. Rosacea and its ocular manifestations. Optometry. 2011;82(2):92-103.
11. Çetinkaya A, Okova YA. Pediatric ocular acne rosacea: long term treatment with systemic antibiotics. Am J Ophthalmol. 2006;142(5): 816-21.
12. Donaldson KE, Karp CL, Dunbar MT. Evaluation and treatment of children with ocular rosacea. Cornea. 2007;26(1):42-6.
13. Blount BW, Pelletier AL. Rosacea: a common, yet commonly overlooked, condition. Am Fam Physician. 2002;66(3):435-40.
14. Two AM, Del Rosso JQ. Kallikrein 5-mediated inflammation in rosacea: clinically relevant correlations with acute and chronic manifestations in rosacea and how individual treatments may provide therapeutic benefit. J Clin Aesthet Dermatol. 2014;7(1):20-5.
15. Sobolewska B, Doycheva D, Deuter C, Pfeffer I, Schaller M, Zierhut M. Treatment of ocular rosacea with once-daily low-dose doxycycline. Cornea. 2014;33(3):257-60.
16. Schechter BA, Katz RS, Friedman LS. Efficacy of topical cyclosporine for the treatment of ocular rosacea. Adv Ther. 2009;26(6):651-9.
17. Frucht-Pery J, Sagi E, Hemo I, Ever-Hadani P. Efficacy of doxycycline and tetracycline in ocular rosacea. Am J Ophthalmol. 1993; 116(1):88-92.
18. Eiseman AS. The ocular manifestations of atopic dermatitis and rosacea. Curr Allergy Asthma Rep. 2006;6(4):292-8
19. Gupta AK, Chaudhry MM. Rosacea and its management: an overview. Eur Acad Dermatol Venereol. 2005;19(3):273-85.
20. Bikowski JB. Subantimicrobial dose doxycycline for acne and rosacea. Skinmed. 2003;2(4):234-45.
21. Shimazaki J, Den S, Omoto M, Satake Y, Shimmura S, Tsubota K. Prospective, randomized study of the efficacy of systemic cyclosporine in high-risk corneal transplantation. Am J Ophthalmol. 2011; 152(1):33-9.
22. Utine CA, Stern M, Akpek EK. Clinical review: topical ophthalmic use of cyclosporin A. Ocul Immunol Inflamm. 2010;18(5):352-61.
23. Pelle MT, Crawford GH, James WD. Rosacea: II. Therapy. J Am Acad Dermatol. 2004;51(4):499-512; quiz 513-4.
24. Sneddon IB. A clinical trial of tetracycline in rosacea. Br J Dermatol. 1966;78(12):649-52.
25. Arman A, Demirseren DD, Takmaz T. Treatment of ocular rosacea: comparative study of topical cyclosporine and oral doxycycline. Int J Ophthalmol. 2015;8(3):544-9.
26. Wilkin J, Dahl M, Detmar M, Drake L, Liang MH, Odom R, Powell F; National Rosacea Society Expert Committee. Standard grading system for rosacea: report of the National Rosacea Society Expert Committee on the classification and staging of rosacea. J Am Acad Dermatol. 2004;50(6):907-12. Comment in: J Am Acad Dermatol. 2005;52(3 Pt 1):539-40.
27. Souchier M, Joffre C, Gregoire S, Bretillon L, Muselier A, Acar N, et al. Changes in meibomian fatty acids and clinical signs in patients with meibomian gland dysfunction after minocycline treatment. Br J Ophthalmol. 2008;92(6):819-22.
28. Jonas M, Cunha BA. Review minocycline. Ther Drug Monit. 1982; 4(2):137-45.
29. Arman A, Demirseren DD, Takmaz T. Treatment of ocular rosacea: comparative study of topical cyclosporine and oral doxycycline. Int J Ophthalmol. 2015;8(3):544-9.
30. Müftüoğlu İK, Akova Y. Clinical findings, follow up and treatment results in patients with ocular rosacea. Turk J Ophthalmol. 2016; 46(1):1-6.
Submitted for publication:
November 28, 2018.
Accepted for publication:
March 20, 2018.
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose
Approved by the following research ethics committee: Adıyaman University (# 2018/2-27)