

Guilherme Eiichi da Silva Takitani; Alexandre Gomes Bortoloti de Azevedo; Fabiana Louise Motta; Sérgio Henrique Teixeira; Juliana Maria Ferraz Sallum; Roberto Murad Vessani
DOI: 10.5935/0004-2749.20180084
ABSTRACT
A 89-year-old Black female with a 6-year history of advanced open-angle glaucoma was referred to the Glaucoma Service of the Ophthalmology Department - Federal University of São Paulo (UNIFESP). Best-corrected visual acuity was 20/400 in the right eye and 20/60 in the left eye. Pseudoexfoliation material was observed at the iris border, angle, and the anterior lens surface. Anterior biomicroscopy revealed exfoliation material forming an evident peripheral zone and a central disc separated by a clear intermediate zone on the anterior lens surface OU. Gonioscopy showed an open-angle Sampaolesis’s line and whitish material deposits OU. Fundus examination revealed a cup-to-disc ratio of 1.0 OU with peripapillary atrophy. Genetic analysis for single nucleotide polymorphisms of the lysyl oxidase-like 1 gene linked to exfoliation syndrome identified two such single nucleotide polymorphisms, rs1048661 and rs216524.
Keywords: Exfoliation syndrome; African continental ancestry group; Exfoliation syndrome; Lysyl oxidase-like 1 gene; Brazil
RESUMO
Uma mulher negra de 89 anos com um histórico de seis anos de glaucoma avançado de ângulo aberto avançado foi encaminhada ao Serviço de Glaucoma do Departamento de Oftalmologia da Universidade Federal de São Paulo (UNIFESP). A acuidade visual melhor corrigida era 20/400 no olho direito e 20/60 no olho esquerdo. Material pseudo-exfoliativo foi observado na borda iriana, ângulo e superfície anterior do cristalino. A biomicroscopia de segmento anterior demonstrou material exfoliativo formando uma zona periférica evidente e um disco central separado por uma zona intermediária livre na cápsula anterior do cristalino. A gonioscopia mostrou uma linha de Sampaolesi de ângulo aberto e depósitos esbranquiçados. O exame de fundo de olho revelou disco óptico com escavação total em ambos os olhos com atrofia peripapilar. A análise genética para polimorfismos de nucleotídeo único do gene semelhante à lysyl oxidase-like 1 ligado à síndrome de esfoliação identificou dois desses polimorfismos de nucleotídeo único, rs1048661 e rs216524.
Descritores: Síndrome de exfoliação; Grupo com ancestrais do continente africano; Síndrome de exfoliação; Gene LOXL-1; Brasil
INTRODUCTION
Exfoliation syndrome (XFS) is the most identifiable cause of open-angle glaucoma(1) and its prevalence has been studied in many different countries around the world. However, there are no large population studies on XFS incidence or etiology in South America.
The syndrome is often regarded as predominant in Caucasians due to high prevalence in Scandinavia(2). There is strong evidence for a genetic predisposition to XFS based on associations with three single nucleotide polymorphisms (SNPs) of the lysyl oxidase-like 1 (LOXL-1) gene (15q24)(3): rs1048661 (c.422G>T; p.Arg141Leu), rs3825942 (c.458G>A; p.Gly153Asp), and rs2165241 (c.1102 + 1976T>C). The LOXL-1 enzyme promotes cross-linking of collagen and elastin in the extracellular matrix, but its exact role in XFS pathogenesis has not been established.
While strongly linked to Caucasian ancestry, recent studies have demonstrated XFS in Black populations, such as South Africans(4). Exfoliative syndrome and resulting exfoliative glaucoma (XFG) diagnosis may be under-diagnosed in the Black population because of low suspicion. This report describes the case of a 89-year-old Black female with advanced glaucoma, clear signs of pseudoexfoliative material, and XFS-linked SNPs of LOXL-1, thus confirming the presence of XFS in the South American Black population.
CASE REPORT
A 89-year-old Black female patient was admitted with a 6-year history of advanced open-angle glaucoma with progressive vision loss OU. She also had a history of trabeculectomy OS 2 years before her first consultation at our service. Best-corrected visual acuity was 20/400 OD and 20/60 OS. Intraocular pressure (IOP) was 16 OU (4 p.m.) under topical therapy (Timolol maleate 0.5% BID, Brimonidine tartrate 0.2% BID, and Travaprost 0.004% QD).
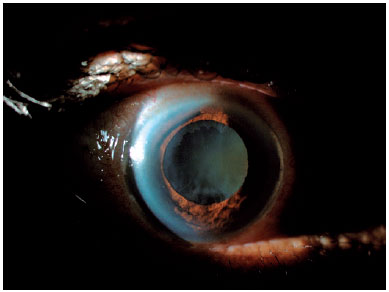
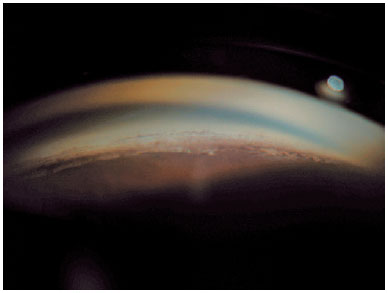
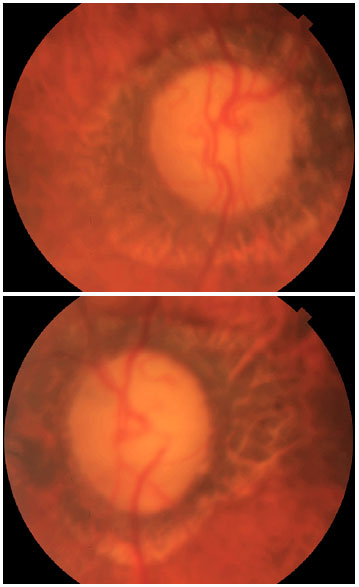
Anterior biomicroscopy revealed pseudoexfoliative material forming three zones on the anterior lens capsule OU (Figure 1). The patient also had 2+ nuclear cataracts OU. Gonioscopy revealed an open-angle Sampaolesis’s line and whitish material deposits (Figure 2) OU. Fundus examination showed a cup-to-disc ratio of 1.0 OU with peripapillary atrophy (Figure 3). Left eye achromatic automated perimetry demonstrated advanced visual field damage.
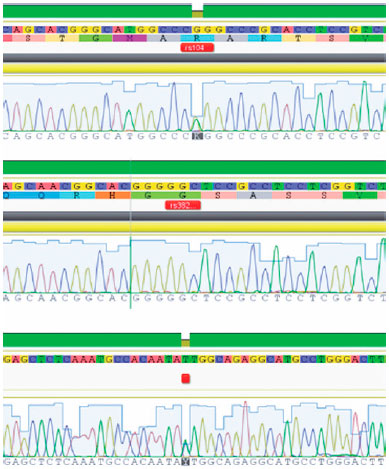
Given these typical findings of XFS, genetic molecular testing was conducted to evaluate the presence of three LOXL-1 SNPs linked to XFS. The test revealed the presence of rs1048661 and rs216524 in heterozygosis and absence of rs3825942 (Figure 4).
DISCUSSION
Exfoliation syndrome is a frequent cause of open-angle glaucoma, and has important implications for clinical management as XFS is associated with more severe glaucoma progression(5). Here we demonstrate the occurrence of XFS linked to LOXL-1 SNPs in a Black patient from South America, suggesting under-reported prevalence in this population.
Exfoliation syndrome is characterized by deposition of fibrilar material on the anterior segment of the eye, most prominently at the pupillary margin and the anterior lens capsule. Deposits at the trabecular meshwork may promote IOP elevation and glaucoma. Exfoliation syndrome is also accompanied by zonular weakness and poor dilatation with concomitant phacodonesis and iridodonesis. These conditions predispose individuals with XFS to complications such as zonular instability and vitreous loss during and after cataract surgery(6). In light of these risks, there are intensive efforts to understand the pathomechanisms of XFS in detail, and such studies have identified strong associations with SNPs of LOXL-1 (rs1048661, rs3825942, and rs2165241). However, the presence of these polymorphisms is not the only determinant of XFS expression. Prevalence varies widely among populations and it is known that the same allele that confers higher risk in one population can be protective in another. Environmental and behavioral factors also appear important for the genesis of XFS(7-9), such as higher altitude, caffeine consumption, low folate, and excessive sun exposure (i.e., outdoor activities and more numerous sunny days and longer daylight hours)(9-10).
Exfoliation material may be found in different visceral organs of patients with XFS(8), and XFS has been associated with cardiovascular and cerebrovascular diseases, elevated homocysteine levels(7), and deafness(8). Therefore, early diagnosis and management of both ocular and systemic conditions is critical. This makes the XFS a very complex disease associated with genetic and environmental factors contributing to the disease appearance and severity.
The current case patient was positive for two of the three SNPs previously linked to XFS, rs1048661 and rs216524 (Figure 4). She also presented with the typical findings of XFS. While originally described in Scandinavians, XFS and XFG have worldwide distribution, and recent studies have revealed considerable prevalence among Blacks. To our knowledge, however, this is the first case described in a Black patient from South America.
Diagnosis of XFS relies on careful examination and a high level of clinical suspicion. The possibility of XFS should be considered when examining older patients with glaucoma regardless of ethnicity.
REFERENCES
1. Ritch R, Schlötzer-Schrehardt U. Exfoliation syndrome. Surv Ophthalmol. 2001;45(4):265-315.
2. Ringvold A. Epidemiology of glaucoma in northern Europe [PMID: 8744847]. Eur J Ophthalmol. 1996;6(1):26-9.
3. Álvarez L, García M, González-Iglesias H, Escribano J, Rodríguez-Calvo PP, Fernández-Vega L, et al. LOXL1 gene variants and their association with pseudoexfoliation glaucoma (XFG) in Spanish patients. BMC Med Genet. 2015;16(1):72.
4. Rotchford AP, Kirwan JF, Johnson GJ, Roux P. Exfoliation syndrome in black South Africans. Arch Ophthalmol. 2003;121(6):863-70.
5. Ernest PJ, Schouten JS, Beckers HJ, Hendrikse F, Prins MH, Webers CA. An evidence-based review of prognostic factors for glaucomatous visual field progression. Ophthalmology. 2013;120(3):512-9.
6. Shingleton BJ, Crandall AS, Ahmed II. Pseudoexfoliation and the cataract surgeon: preoperative, intraoperative, and postoperative issues related to intraocular pressure, cataract, and intraocular lenses. J Cataract Refract Surg. 2009;35(6):1101-20. Review.
7. Vessani RM, Ritch R, Liebmann JM, Jofe M. Plasma homocysteine is elevated in patients with exfoliation syndrome. Am J Ophthalmol. 2003;136(1):41-6.
8. Ritch R. Ocular and systemic manifestations of exfoliation syndrome [PubMed]. J Glaucoma. 2014;23(8 Suppl 1):S1-8.
9. Kang JH, Wiggs JL, Pasquale LR. Relation between time spent outdoors and exfoliation glaucoma or exfoliation glaucoma suspect. Am J Ophthalmol. 2014;158(3):605-14.e1.
10. Nathan N, Kuchtey RW. Genetics, Diagnosis, and Monitoring of Pseudoexfoliation Glaucoma. Curr Ophthalmol Rep. 2016;4(4):206-12.
Submitted for publication:
April 13, 2018.
Accepted for publication:
May 27, 2018.
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflicts of interest to disclose