

Vinicius Targa Villas Bôas1; Gildásio Castello de Almeida Júnior1; Margarete Teresa Gottardo de Almeida2; Maicon Santos Gonçalves3; Leandro Fernandes Coelho1
DOI: 10.5935/0004-2749.20180074
ABSTRACT
Purpose: The aim of this study was to analyze the bacterial and fungal microbiota found in contact lens cases among two groups of patients to correlate the data on the habits of contact lens users and to evaluate whether there is a difference in the culture results between users of ridged and nonridged contact lens cases.
Methods: Two groups (35 patients per group) were included, consisting of hospital workers and those who had not visited a hospital in the past 30 days, and a questionnaire regarding epidemiological data and habits related to contact lens and lens case use was administered. In addition, 140 samples collected from the right and left compartments of each lens case by swabbing the bottom of the wells were tested using bacterioscopy as well as fungal and bacterial cultures via computerized identification of the species.
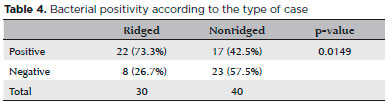
Results: No fungal growth was identified in any of the 70 contact lens cases; however, bacteria were found in 39 cases, and there was no statistical difference between the groups. Most bacteria (>85%) were gram-negative bacilli. Contamination inone compartment of the contact lens case elevated the risk of contamination of the other side (>80%). Moreover, contamination was statistically higher in the ridged cases than in nonridged cases (p=0.0149).
Conclusion: The types of bacteria contaminating the cases are generally not seen in eye diseases associated with contact lens use, suggesting that other decisive variables are involved in eye infection from a contaminated lens or case. Fungal contamination of contact lens cases appears to be an exception. Ridged cases are commonly used by contact lens wearers and present a potential risk to eye health. In addition, the results of bacterial tests between hospital workers and those who did not visit a hospital were not significantly different.
Keywords: Contact lenses; Keratitis; Hospital; Microbiota
RESUMO
Objetivo: O objetivo deste trabalho foi analisar a microbiota bacteriana e fúngica encontrada em estojos de lentes de contato em dois grupos, correlacionar os dados sobre os hábitos de uso de lentes de contato e avaliar se há diferença na positividade das culturas entre os usuários estojos de lentes de contato com ranhuras e sem ranhuras.
Métodos: Dois grupos foram formados, trabalhadores do hospital e pessoas que não visitaram o hospital (35 indivíduos por grupo), e um questionário foi aplicado sobre dados epidemiológicos e hábitos relacionados ao uso de lentes de contato e estojos de lentes. Além disso, 140 amostras, coletadas do compartimento direito e esquerdo de cada estojo de lente, esfregando o fundo dos mesmos, foram testadas por bacterioscopia e por culturas de fungos e bactérias, com identificação computadorizada da espécie.
Resultados: Não houve crescimento fúngico em nenhum dos 70 estojos de lentes de contato, porém bactérias foram encontradas em 39; não houve diferença estatística entre os grupos. A maioria das bactérias (>85%) eram bacilos gram-negativos. Quando um compartimento estava contaminado, o risco de contaminação do outro compartimento era elevado (>80%). A contaminação foi estatisticamente maior nos estojos com ranhuras (p=0,0149).
Conclusão: A contaminação dos estojos parece ocorrer por bactérias que, em geral, não são encontradas em doenças oculares associadas ao uso de lentes de contato, sugerindo que existem outras variáveis decisivas nas infecções oculares de uma lente ou estojo contaminado. Contaminação de estojos de lentes de contato com fungos parece ser uma exceção. O uso de estojos com ranhuras é uma prática comum e apresenta um risco potencial à saúde ocular. Não foram encontradas diferenças significativas nos resultados dos testes bacterianos entre trabalhadores hospitalares e pessoas que não visitaram o hospital.
Descritores: Lentes de contato; Ceratite; Hospital; Microbiota
INTRODUCTION
The use of contact lenses is an important risk factor for the development of eye diseases, particularly infectious keratitis(1,2). It is estimated that 25%-30% of corneal ulcers are associated with contact lens use(3).
One of the risk factors for eye disease in contact lens users is the introducing pathogens into the eye, as microorganisms can adhere and multiply in this environment. Another risk factor of wearing contacts is corneal hypoxia, which compromises the integrity of the epithelium and creates an entry point for microorganisms(4).
Contact lens contamination and eye infections often occur as a result of not following the standard care proceduresrecommended by ophthalmologists, which include a series of steps for properly cleaning the lenses. Factors known to increase the risk of eye infections include the use of contaminated solutions and cases, improper handling of the lens, using tap water to rinse the lens, prolonged use, reuse, and poor hygiene(2,5-7).
When contact lenses become contaminated, the contact lens case then becomes a potential source of pathogens, especially when it is not being properly cleaned and disinfected. Thus, even cleaning and sterilizing contact lenses does not imply an innocuous environment since the source could be a contaminated case. This has been confirmed in studies showing that microorganisms isolated from contact lenses that are associated with infectious eye diseases are identical to those isolated from the corresponding contact lens cases(8-10).
Fungi are a major global cause of infectious keratitis, especially in tropical regions involving the genera Fusarium, Aspergillus, Curvularia, Bipolaris, and Candida(11). In this scenario, the risk factors for eye infection are misuse of steroidal anti-inflammatory drugs, prolonged antimicrobial therapy, eye injury, pre-existing corneal disease, and the use of contact lenses(12).
The use of contact lenses is the primary risk factor for the development of bacterial keratitis, which in turn increases the risk of infectious keratitis by 10-to 15-fold when contact lenses are used for a limited number of hours per day when compared to extended wear(13). About 90% of cases of bacterial keratitis are caused by organisms of one of the following groups: Micrococcaceae (Staphylococcus, Micrococcus), Streptococcus, Pseudomonassp. and Enterobacteriaceae (Citrobacter, Klebsiella, Enterobacter, Serratia, and Proteus). Frequently found organisms include Pseudomonas spp., Staphylococcus spp., Streptococcus sp., and Proteus sp.(13). The primary organism isolated from infectious keratitis in contact lenses users is P. aeruginosa(1-2).
Hospital microflora is known to differ from that found outside the hospital, making the hospital a different environment regarding the prevalence and virulence of different types of microorganisms. These differences may be clinically important in ophthalmology, especially because, in many cases, nosocomial pathogens have greater variation in antimicrobial resistance(14).
The aim of this work was to analyze the bacterial and fungal microbiota found in contact lens cases. Two groups were studied, hospital workersand people who did not visit a hospital, to correlate data on the habits of contact lens use and evaluate whether there is a difference in culture positivity between ridged versus nonridged contact lens cases.
METHODS
Overall, 35 samples were collected from each of the two compartments ofcontact lenscases belonging to workersat Hospital de Base in São José do Rio Preto (Group1) and from both compartments of cases of 35 individuals who did not visit a hospital (Group2 [nonvisitors]), totaling 140 samples from 70 cases.
The term hospital workers (Group 1) was defined as those workers who worked in the hospital at least three times a week for a minimum of 3 hours per day; this group was formed by physicians, nurses, and medical students. Individuals in 2 had not visited any hospital in the 30 days prior to sample collection.
A questionnaire was administered to the groups regarding demographic and epidemiological data including questions related to factors possibly affecting microbiological contamination, for which data were collected on age, sex, place of residence, length of time contact lenses and cases were in use, frequency of use, type of use, contact lens type, and cleaning the contact lenses and cases. Furthermore, the frequency of hospital visits and lengths of stay were evaluated in the hospital workers (average, 5.71 days per week and 7.8 hours per day).
After informed consent forms were signed, the contact lens cases were collected and sent to the microbiology laboratory of FAMERP, and the cases were analyzed for bacterial and fungal growth.
Microbiological analysis
The wells of each case were wiped using a sterile cotton swab that was moistened with distilled water and swiped in a circular motion, ensuring that the entire inside of the compartment was swabbed. The swab was immediately placed in a nutrient-rich broth (Tryptic Soy Broth®, DIFCO) and incubated at 37°C for 24-48 hours. Subsequently, 0.1 mL of the broth was inoculated indifferent dishes containing blood agar, MacConkey agar, chocolate agar, or Sabouraud dextrose agar, all of which were acquired from DIFCO®. The dishes were incubated at 37°C for 24-48 hours to isolate the bacteria and for 15 days to isolate the fungi. The VITEK® SYSTEM was used to identify the isolated bacterial colonies.
Statistics tests were performed to determine whether there were any statistically significant differences between the groups using the D’Agostino-Pearson normality test, Shapiro-Wilk normality test, Kolmogorov-Smirnov normality test, Fisher exact test, Mann-Whitney U test, and Koopman asymptotic score.
This research was approved by the Research Ethics Committee of the Medical School of São José do Rio Preto (FAMERP - #12425513.5.0000.5415).
RESULTS
The groups
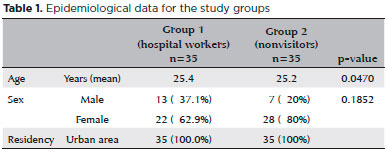
Data obtained from the questionnaire for each group related to demographic characteristics of subjects and their contact lens use are shown in tables 1 and 2, respectively.
The microbiota
No fungal growth was identified in any of the samples collected despite the use of rigorous methodology.
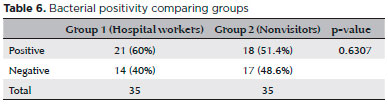
The bacterial cultures were positive in 60% of contact lens cases in Group 1 and 51.4% in Group 2. Of the compartments, 55.7% in Group 1 and 47.1% in Group 2 were positive for bacteria. In the majority of cases, when one compartment was contaminated, the other had a high likelihood of being contaminated (85.7% in Group 1 vs. 83.3% in Group 2 and 61.1% in Group 1. 66.7% in Group 2 by the same bacterium.
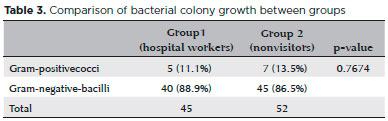
Of the 45 colonies isolated in Group 1, 88.9% were gram-negative bacilli and the remaining 11.1% were gram-positive cocci, and this was similar to the results in Group 2, where 52 colonies were isolated, and86.5% were gram-negative bacilli while the remaining 13.5% were gram-positive cocci (Table 3).
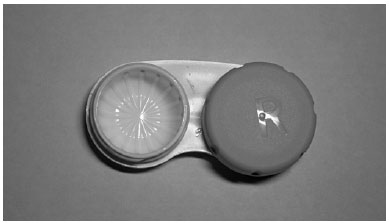
Of the 70 contact lens cases, 30 were ridged inside (Figure 1). The ridged cases had a higher number of positive cultures when compared to the nonridged cases (Table 4).
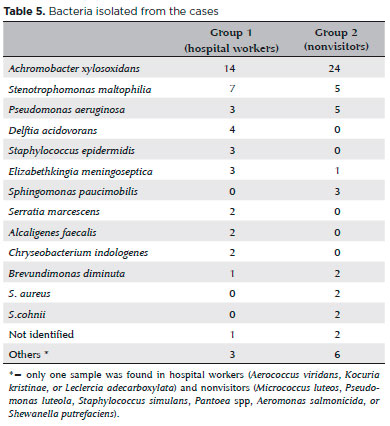
The most prevalent bacterium in both groups was Achromobacter xylosoxidans at 31.1% of the total in Group 1 and 46.1% in Group 2. The second most prevalent bacterium in Group 1 was Stenotrophomonas maltophilia (15.5% of all cases), whereas S. maltophilia had the same incidence as P. aeruginosa (9.6% each) in Group 2. The other bacteria found in the cases are shown in table 5.
DISCUSSION
Overall, 31.43% of the users in both groups reported that they did not clean their contact lenses, with 28.6% in Group 1 and 25.72% in Group 2. The reason for this may be related to a poor doctor-patient relationship, a lack of clear instructions from the physician, the large number of participants using nonprescription contact lenses without medical supervision, or a lack of knowledge about the risks, all of which have been reported in previous studies(2,6). However, as reported in a previous article(4), bacterial positivity was similar regardless of whether the user reported cleaning the lenses or the case, and this was possibly due to the users’ lack of knowledge regarding the correct cleaning regimen.
Despite the difference between the groups (median 90 days vs. 180 days in Groups 1 and 2, respectively), no statistical difference was found in the length of time the cases were used (Table 6; p=0.6307), and both groups followed the guidelines in the literature recommending that cases be replaced every six months(5,10).
Four of five users of rigid permeable gas contact lenses used ridged cases, and 26 of 61 users of gelatinous contact lenses had ridged cases. This fact would not have been important if we had not noticed that the incidence of cases with positive cultures was much higher in those cases with ridges (Table 5; p=0.0149), which can be explained by the larger surface area generated by the ridges facilitating microbial adhesion and biofilm formation in addition to making cleaning difficult(10).
There was no sign of fungal growth in the two groups, which is in agreement with other studies showing a low prevalence of fungi in contact lens cases(1,3). In total, more than half of the cases in both groups were contaminated with bacterial growth, primarily with gram-negative bacilli, which has also been reported in the literature(3).We found that with contamination of one compartment of the contact lens case was a high likelihood of contamination of the other compartment (>80%), suggesting that contamination occurs due to the handling of the contact lenses and cases, which has also been discussed in other studies(15,16).
The microorganisms found in each group were similar. Bacteria isolated only in Group 1 included Serratia marcescens(17), Staphylococcus epidermidis(18), Chryseobacterium indologenes(19), Delftia acidovorans(20), Leclercia adecarboxylata(21), Kocuria kristinae(22), Aerococcus viridans(23), and Alcaligenes faecalis(24). With the exception of S.marcescens, these bacteria mostly have low virulence but may present high resistance to common antibiotics and may seriously affect immunosuppressed patients.
Although most cases of bacterial keratoconjunctivitis are caused by Micrococcaceae, Streptococcus, Pseudomonas sp., and Enterobacteriaceae(13), less than one-fourth of the total bacteria belonged to these genera. These findings suggest that there are multiple, decisive variants for contamination to become an infection.
The prevalence of Pseudomonas sp. was 6.66% vs. 9.61% in Groups 1and 2, respectively, which is alarming, as we know that this bacterium is known to cause high morbidity, especially in contact lens users.
In conclusion, contamination of contact lens cases appears to involve a range of bacteria that, in general, are not usually associated with eye diseases correlated to contact lens use, suggesting that other decisive variables are related to eye infections that are caused by contaminated lenses and cases. Fungal contamination of contact lens cases appears to be an exception. Contact lens cases with ridges are commonly used and considered potentially damaging to eye health compared to nonridged cases since they presented greater positivity of bacterial growth. There were no significant differences between the positive results of bacterial tests between hospital workers and individuals who did not enter the hospital environment.
REFERENCES
1. Silveira Moriyama A, Hofling-Lima AL. Contact lens-associated microbial keratitis. Arq Bras Oftalmol. 2008;71(6):32-6.
2. Abdelkader A. Cosmetic soft contact lens associated ulcerative keratitis in southern Saudi Arabia. Middle East Afr J Ophthalmol. 2014;21(3):232-5.
3. Velasco J, Bermudez J. Comparative study of the microbial flora on contact lenses, in lens cases, and in maintenance liquids. Int Contact Lens Clin. 1996;23(2):55-8.
4. Dart J. The inside story: why contact lens cases become contaminated. Contact Lens Anterior Eye. 1997;20(4):113-8.
5. Lipener C, Ray CBM. Sistemas atuais de cuidados e manutenção de lentes de contato. Arq Bras Oftalmol. 2008;71(6 SUPP):9-13.
6. Arlene G, Lui F, Netto AL. Avaliação do nível de conhecimento quanto ao uso de lentes de contato entre os estudantes de medicina da Faculdade de Medicina do ABC. Rev Bras Oftalmol. 2010; 69(6):361-6.
7. Lipener C, Parolin Ribeiro AL. Úlcera de córnea bilateral por pseudomonas em usuário de lente de contato descartável. Arq Bras Oftalmol. 1999;62(6):747-9.
8. Bharathi MJ, Sc M, Ph D. Ulcerative keratitis associated with contact lens wear. Indian J Ophthalmol. 2007;55(1):64-7.
9. Gray TB, Cursons RT, Sherwan JF, Rose PR. Acanthamoeba, bacterial, and fungal contamination of contact lens storage cases. Br J Ophthalmol. 1995;79(6):601-5.
10. Wu YTY, Willcox M, Zhu H, Stapleton F. Contact lens hygiene compliance and lens case contamination: a review. Contact Lens Anterior Eye. 2015;38(5):307-16.
11. Maharana PK, Sharma N, Nagpal R, Jhanji V, Das S, Vajpayee RB. Review Article Recent advances in diagnosis and management of Mycotic Keratitis. Indian J Opthalmol. 2016;64:346-57.
12. De Oliveira PR, Resende SM, De Oliveira FC, De Oliveira AC. Ceratite fúngica. Arq Bras Oftalmol. 2001;64(1):75-9.
13. Brasileira S, Lentes DECE, Soblec DEC. Úlcera de córnea bacteriana. Arq Bras Oftalmol. 2000;63(1):495-8.
14. Rubio FG, Oliveira VDC, Rangel RMC, Nogueira MCL, Almeida MTG. Trends in bacterial resistance in a tertiary university hospital over one decade. Braz J Infect Dis. 2013;17(4):480-2.
15. Mowrey-McKee MF, Monnat K, Sampson HJ, Smith CM, Davies GA, Mandt L, et al. Microbial contamination of hydrophilic contact lenses. Part I: Quantitation of microbes on patient worn-and-handled lenses. CLAO J. 1992;18(2):87-91.
16. Mowrey-McKee MF, Sampson HJ, Proskin HM. Microbial contamination of hydrophilic contact lenses. Part II: Quantitation of microbes after patient handling and after aseptic removal from the eye. CLAO J. 1992;18(4):240-4.
17. Chaidaroon W, Supalaset S. Corneal ring infiltrates caused by serratia marcescens in a patient with human immunodeficiency virus. Case Rep Ophthalmol. 2016;7(2):359-63.
18. Whist E, Hollenbach E, Dunlop A. Severe acute endogenous endophthalmitis with Staphylococcus epidermidis in a systemically well patient. Ophthalmol Eye Dis. 2011;3:25-8.
19. Caso RDE. Infecção por Chryseobacterium indologenes: relato de um caso. Rev Bras Ter Intensiva. 2010;22(1):96-8.
20. Ray M, Lim DK. A Rare Polymicrobial Keratitis Involving Chryseobacterium meningosepticum and Delftia acidovorans in a cosmetic contact lens wearer. Eye Contact Lens. 2013;39(2):192-3.
21. Anuradha M. Leclercia adecarboxylata isolation: Case reports and review. J Clin Diagnostic Res. 2014;8(12):DD03-DD04.
22. Domont F, Hamdad F, Brémond‐Gignac D, Le Flèche‐Matéos A. Kocuria dacryocystitis infection, caused by kocuria ocularis sp. Nov. JMM Case Reports. 2014;1(2):1-4.
23. Parrey AH, Sofi F, Ahmad M, Kuchay A. Aerococcus viridans infection presenting as cutaneous vasculitis in an immunocompetent patient. Reumatologia. 2016;54(6):318-20.
24. Khokhar DS, Sethi HS, Kumar H, Sudan R, Sharma N, Nayak N. Postkeratoplasty endophthalmitis by Alcaligenes faecalis: a case report. Cornea. 2002;21(2):232-3.
Submitted for publication:
June 13, 2017.
Accepted for publication:
March 13, 2018.
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflicts of interest to disclose
Approved by the following research ethics committee: Medical School of São José do Rio Preto (FAMERP - # 12425513.5.0000.5415)