

Mário Luiz Ribeiro Monteiro1; César Moreira Sampaio1
DOI: 10.1590/S0004-27492002000600015
ABSTRACT
Purpose: To report a case of Erdheim-Chester disease with bilateral orbital involvement and to inform ophthalmologists about this uncommon condition. Methods: Case report. A 41-year-old man presented with proptosis, lid xanthelasmas, disc edema and extraocular muscle restrictions. He was suspected of having a systemic lymphoma and had already been submitted to a retroperitoneal biopsy, however, the diagnosis was still uncertain. Results: The patient was evaluated by computed tomography and magnetic resonance imaging of the orbit. Orbital pseudotumor was suspected and a biopsy of the orbital lesion initially failed to provide the correct diagnosis which was only made after detailed analysis of the clinical and imaging findings, and review of the histopathologic studies. The systemic diagnosis was made after the orbital diagnosis although the patient had been extensively investigated for more than one year. Conclusions: Erdheim-Chester disease is a rare idiopathic systemic condition characterized by a xanthogranulomatous process involving retroperitoneum, heart, lungs, bone and other tissues. The condition is often fatal due to renal or cardiovascular complications. Ocular findings are rare but may be very helpful for the diagnosis. Therefore, ophthalmologists should be aware of the clinical manifestations and imaging findings of this rare disease in order to establish an early diagnosis.
Keywords: Langerhans-cell histiocytosis; Orbital diseases; Xanthomatosis; Orbit; X-ray computed tomography; Magnetic resonance imaging; Case report
RESUMO
Objetivo: Relatar um caso de doença de Erdheim-Chester com envolvimento orbital bilateral e informar os oftalmologistas a respeito dessa condição incomum. Métodos: Relato de caso. Paciente do sexo masculino, 41 anos de idade, apresentou com proptose, xantelasmas, edema do disco óptico e restrição dos músculos extraoculares. A suspeita diagnóstica era de linfoma com envolvimento sistêmico e já havia sido submetido à biópsia do retroperitônio, mas o diagnóstico ainda era inconclusivo. Resultados: O paciente foi submetido a exame de tomografia computadorizada e imagem por ressonância magnética da órbita. Foi feita a suspeita de pseudotumor orbitário e biópsia orbital foi realizada. Esta não revelou o diagnóstico correto que foi feito apenas após análise detalhada dos dados clínicos e de imagem e após revisão dos exames histopatológicos. O diagnóstico sistêmico só foi feito após o diagnóstico da afecção orbitária embora o paciente já estivesse sendo investigado do ponto de vista clínico por mais de um ano. Conclusão: A doença de Erdheim-Chester é condição sistêmica idiopática caracterizada por processo xantogranulomatoso envolvendo o retroperitônio, coração, pulmões, ossos e outros tecidos. A condição freqüentemente é fatal devido a complicações renais e cardiovasculares. Os achados oculares são incomuns e podem auxiliar no diagnóstico. Os oftalmologistas devem, portanto, conhecer as manifestações clínicas e os achados de imagem dessa doença e auxiliar no seu diagnóstico precoce.
Descritores: Histiocitose de células de Langerhans; Doenças orbitárias; Xantomatose; Órbita; Tomografia computadorizada por raios x; Imagem por ressonância magnética; Relato de caso
INTRODUCTION
Erdheim-Chester disease is a rare systemic xanthogranulomatosis, of unknown etiology, characterized by infiltration of the bones, heart, lungs, kidney, retroperitoneum and other tissues by xanthomatous histiocytes and multinucleated Touton giant cells. The condition is often fatal due to cardiac, pulmonary and renal insufficiency(1-2). Orbital involvement is extremely rare with only 25 previously reported cases in the literature(1-8).
The aim of this paper is to document one more case of orbital involvement in Erdheim-Chester disease emphasizing the clinical and imaging findings that can help to establish an early diagnosis.
METHODS
A 41-year-old male patient complained of proptosis and swelling of both eyes and intermittent double vision for one year. He had been admitted to a hospital 8 months earlier because of abdominal pain, urinary retention, pulmonary edema and cardiac decompensation of unknown origin. An extensive clinical and laboratory investigation showed marked splenomegaly but a search for lymphoma was negative. He was then submitted to an exploratory laparotomy with biopsy of abdominal ganglions and retroperitoneum which yielded a presumed diagnosis of lymphadenitis associated with peritonitis. Liver biopsy performed at the same time showed normal findings. He was submitted to periodic intramuscular injections of beclometasone in order to improve his abdominal pain. He denied any orbital pain.
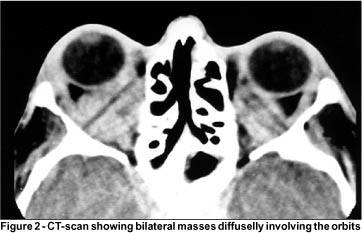
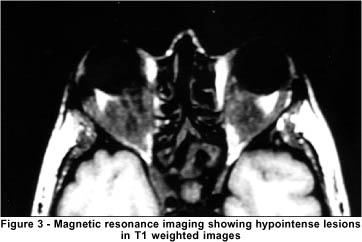
On examination, his best corrected visual acuity was 20/25 in the right eye (OD) and 20/20 in the left eye (OS). He had bilateral xanthelasmas in the superior and inferior eyelids and bilateral proptosis. Exophthalmometry (Hertel base 98) was 23 mm OD and 20 mm OS (Figure 1). The eyes were aligned in the primary position but there was marked restriction of elevation, adduction and abduction of both eyes. Slit lamp examination, pupillary reactions and intra-ocular pressure measurements were normal. Fundoscopy showed mild optic disc edema in OD. Computerized tomography (CT) of the orbits showed a hyperdense lesion diffusely involving the orbit (Figure 2). Magnetic resonance imaging disclosed diffuse infiltration of the orbits with a hypointense lesion in T1 (Figure 3) and T2 weighted images.
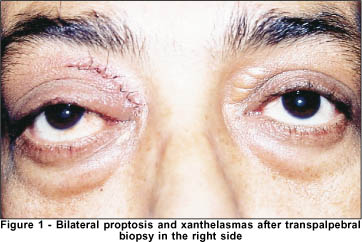
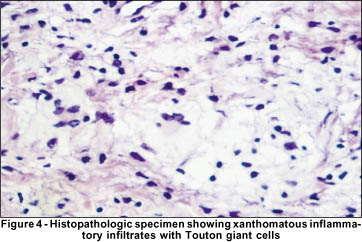
The patient was submitted to a biopsy of the orbital lesion in the right side, through an anterior orbitotomy with a lid incision. Infiltration of the orbital fat was observed at surgery. The initial diagnosis was of an atypical pseudotumor but there was no correlation with the clinical picture due to the lack of pain and inflammatory signs in the orbit as well as with the systemic involvement of the condition. After a literature search however, a suspicion of a xanthogranulomatosis was made and the pathologic studies both of the orbit as well as of the retroperitoneum were reviewed. Many lipid-laden hystiocytes forming groups of xanthomatous cells separated by fibrotic septa were found extending to the adipose tissue. There was also focal infiltration of lymphocytes, plasma cells and Touton giant cells throughout the tissue (Figure 4) confirming the diagnosis of Erdheim-Chester disease. The orbital lesion remained unchanged but the patient died of systemic complications a few months later.
DISCUSSION
Xanthogranulomas are granulomas formed by lipid-laden histiocytes, which impart a yellow coloration to superficial lesions, and gross examination of tissue specimens shows characteristically multinucleated Touton giant cells in the lesion. Xanthogranulomas are present in three conditions which affect the periocular area: juvenile xanthogranulomas, necrobiotic xanthogranulomas and Erdheim-Chester disease(9).
Erdheim-Chester disease is a condition termed by Jaffe in 1972 to describe a systemic disease first reported by Chester and Erdheim in 1930. It is now recognized to be an adult onset idiopathic systemic disorder with involvement of viscera, bone, subcutaneous tissues and by a sclerosing xanthogranulomatous process. The condition is often fatal due to renal or cardiovascular complications(2,4).
In 1983 Alper et al. described for the first time orbital involvement in two patients with Erdheim-Chester disease(1). Since this description 23 other patients have been reported in the literature(2-8). Orbital involvement is characterized by broad sheets of xanthoma cells with scattered foci of chronic inflammatory cells, mostly lymphocytes and plasma cells. There are also fibrosis and multinucleated giant cells in the xanthogranulomatous infiltration(2). Such involvement can lead to the clinical findings of proptosis, extraocular muscle restriction, disc edema, optic atrophy, retinal striae and yellowish infiltration of the lid skin.
The differential diagnosis of Erdheim-Chester disease in the orbit is extensive and includes dysthyroid orbitopathy, idiopathic orbital inflammation, lymphoma, metastatic carcinoma and Langerhans' cell histiocytosis. None of these conditions is typically associated with xanthelasmas and they all should be ruled out based on clinical, laboratory and histopathological findings. Imaging is also very important as auxiliary method for early diagnosis of orbital Erdheim-Chester disease, although to date, no specific pattern of involvement has been defined. CT scan usually shows a diffuse infiltration of the orbit and eyelids (Figure 2). The same finding can be observed on MRI that reveals hypointense lesions on T1 and T2 weighted images. Ultrasonography shows a lesion with medium to high internal reflectivity(4). These imaging findings can lead to confusion with nonspecific inflammation of the orbit. However, in most cases of Erdheim-Chester disease involvement of the orbit is very extensive and there is characteristically absence of pain and inflammatory signs, which helps in the differentiation of this condition from nonspecific orbital inflammation.
The prognosis for survival is usually poor and dependent on the extent of visceral involvement. Most patients die because of congestive heart failure, lung fibrosis or renal insufficiency. Treatment with corticosteroids, radiotherapy or chemotherapy is frequently not effective and the disease usually progresses (3). Failure to respond to these treatment modalities may be related to the fact that the majority of patients are diagnosed late in the course of the disease. For example, in our patient the diagnosis was not made until one year later despite being submitted to an exploratory laparotomy and abdominal biopsies. The delay in the diagnosis may have in some way contributed to his unfortunate outcome. The diagnosis was established only after the clinical suspicion, based on the presence of xanthelasmas, absence of orbital pain and relentless evolution, which led to a review of the pathologic specimens both from the orbit as well as from the retroperitoneum. Valmaggia et al.(3) recently reported one patient that who diagnosed early in the course of the disease with a much better outcome in a three-year follow-up period. Therefore it is possible that the timing for initiating appropriate therapy may be decisive for the course of the disease.
CONCLUSION
In conclusion, Erdheim-Chester disease is a rare systemic condition characterized by a xanthogranulomatous process involving retroperitoneum, heart, lungs, bone and other tissues. The condition is often fatal due to renal or cardiovascular complications. Ocular findings are rare but may be very helpful for the diagnosis. Therefore, ophthalmologists should be aware of the clinical manifestations and imaging findings of this rare disease in order to establish an early diagnosis.
RESUMO
Objetivo: Relatar um caso de doença de Erdheim-Chester com envolvimento orbital bilateral e informar os oftalmologistas a respeito dessa condição incomum. Métodos: Relato de caso. Paciente do sexo masculino, 41 anos de idade, apresentou com proptose, xantelasmas, edema do disco óptico e restrição dos músculos extraoculares. A suspeita diagnóstica era de linfoma com envolvimento sistêmico e já havia sido submetido à biópsia do retroperitônio, mas o diagnóstico ainda era inconclusivo. Resultados: O paciente foi submetido a exame de tomografia computadorizada e imagem por ressonância magnética da órbita. Foi feita a suspeita de pseudotumor orbitário e biópsia orbital foi realizada. Esta não revelou o diagnóstico correto que foi feito apenas após análise detalhada dos dados clínicos e de imagem e após revisão dos exames histopatológicos. O diagnóstico sistêmico só foi feito após o diagnóstico da afecção orbitária embora o paciente já estivesse sendo investigado do ponto de vista clínico por mais de um ano. Conclusão: A doença de Erdheim-Chester é condição sistêmica idiopática caracterizada por processo xantogranulomatoso envolvendo o retroperitônio, coração, pulmões, ossos e outros tecidos. A condição freqüentemente é fatal devido a complicações renais e cardiovasculares. Os achados oculares são incomuns e podem auxiliar no diagnóstico. Os oftalmologistas devem, portanto, conhecer as manifestações clínicas e os achados de imagem dessa doença e auxiliar no seu diagnóstico precoce.
Descritores: Histiocitose de células de Langerhans; Doenças orbitárias; Xantomatose; Órbita/radiografia; Tomografia computadorizada por raios x; Imagem por ressonância magnética; Relato de caso
REFERENCES
1. Alper MG, Zimmerman LE, Piana FG: Orbital manifestation of Erdheim-Chester disease. Trans Am Ophthalmol Soc 1983;81:64-85.
2. Shields JA, Karcioglu ZA, Shields CL, Eagle RC, Wong S. Orbital and eyelid involvement with Erdheim-Chester disease. A report of two cases. Arch Ophthalmol 1991;109:850-4.
3. Valmaggia C, Neuweiler J, Fretz C, Gottlob I. A case of Erdheim-Chester disease with orbital involvement. Arch Ophthalmol. 1997;115:1467-8.
4. Palma P, Ravalli L, Grisanti F, Rossi A, Marzola A, Nielsen I. Bilateral orbital involvement in Erdheim-Chester disease. Orbit 1998;17:97-105.
5. Sheidow TG, Nicolle DA, Heathcote JG. Erdheim-Chester disease: two cases of orbital involvement. Eye 2000; 14(Pt 4):606-12.
6. Chollet P, Eyremandi R, Lesueur L, Arne JL. La maladie d'Erdheim-Chester: une étiologie rare de tumeur retrobulbaire. J Fr Ophtalmol 1994;17:200-3.
7. Offret H, Hannouche D, Frau E, Doyon D, Quillard J, Schaison G. Maladie d'Erdheim-Chester orbitaire. J Fr Ophtalmol 1995;18:220-5.
8. Le Goff L, Berros P, Denis D, Ridings B: Bilateral exophthalmos diabetes insipidus: Erdheim-Chester disease. Clinical and radiological findings. J Fr Ophtalmol 2002;25:57-61.
9. Rose GE, Patel BC, Garner A, Wright JE. Orbital xanthogranuloma in adults. Br J Ophthalmol 1991;75:680-4.
1 From the division of Ophthalmology, Hospital das Clínicas of the University of São Paulo Medical School, São Paulo, Brazil.
Corresponding address: Av. Angélica 1757 conj. 61 - São Paulo (SP) CEP 01227-200.
E-mail: [email protected]
Recebido para publicação em 22.04.2002
Aceito para publicação em 14.08.2002