

Juan Carlos Montalt1; Esteban Porcar1; Enrique España-Gregori2; Cristina Peris-Martínez3
DOI: 10.5935/0004-2749.20180061
ABSTRACT
Purpose: We aimed to describe the outcomes of corneoscleral contact lens fitting with multi-aspherical geometry designs in patients with irregular corneas after laser-assisted in situ keratomileusis (LASIK).
Methods: This was a retrospective series of 18 patients (age, 26-38 years) selected from an eye clinic database. Participants were required to have unsatisfactory visual acuity with their current contact lenses or spectacles after LASIK for myopia correction. All patients were fitted with corneoscleral contact lenses designed to correct corneal surface irregularities. A diagnostic trial set was used for fitting, and assessments were performed according to a standardized methodology. Subjective comfort, visual acuity, central corneal thickness, endothelial cell count, and corneal-compensated intraocular pressure were evaluated. The follow-up period was one year.
Results: Contact lens use was discontinued in 3 patients, thus leaving 24 eyes from 8 females and 7 males for analysis. The fitting characteristics were optimal in terms of lens position and movement. Statistically significant improvements were found in the best spectacle-corrected vision from before fitting to the visual acuity after fitting (p<0.001). Moreover, the patients reported high subjective comfort ratings and usage times (12.98 ± 2.3 hours/day). After one year of wear, visual acuity, subjective comfort, and usage time were maintained. No statistically significant adverse changes developed in the corneas over this period.
Conclusion: Corneoscleral contact lenses with a multi-aspherical geometry design provide optimal visual acuity, improved comfort, and prolonged usage times in patients with irregular corneas after LASIK.
Keywords: Contact lenses; Corneal surgery, laser; Corneal pachymetry; Corneal endothelial cell loss; Intraocular pressure
RESUMO
Objetivo: Descrever os resultados do ajuste de lentes de contato corneoesclerais com geometria multiasférica em pacientes com córneas irregulares após cirurgia de ceratomileuse in situ assistida por laser (LASIK).
Métodos: Esta foi uma série retrospectiva de 18 pacientes (idade, 26-38 anos) selecionados a partir de um banco de dados de uma clínica oftalmológica. Os participantes foram escolhidos ao manifestaram acuidade visual insatisfatória com suas lentes de contato ou óculos atuais depois de terem sido submetidos à LASIK para correção de miopia. Todos os pacientes receberam lentes de contato corneoesclerais projetadas para corrigir irregularidades na superficie da córnea. Um conjunto diagnóstico de prova foi usado para a adaptação e as avaliações foram feitas de acordo com uma metodologia padronizada. O conforto subjetivo, a acuidade visual, a espessura central da córnea, a contagem de células endoteliais e a pressão intraocular compensada da córnea foram avaliados. O período de acompanhamento foi de um ano.
Resultados: O uso de lentes de contato foi descontinuado em 3 pacientes, deixando 24 olhos de 8 mulheres e 7 homens para análise. As características de adaptação foram ótimas em termos de posição e movimento da lente. Melhorias estatisticamente significativas foram encontradas na melhoria da visão corrigida por óculos antes de se ajustar a acuidade visual após a adaptação (p<0,001). Além disso, os pacientes relataram altos índices subjetivos de conforto e tempo de uso (12,98 ± 2,3 horas/dia). Após um ano de uso, a acuidade visual, o conforto subjetivo e o tempo de uso foram mantidos. Não houve alterações adversas estatisticamente significativas nas córneas ao longo deste período.
Conclusão: As lentes de contato corneoesclerais com projeto geométrico multiasférico proporcionam acuidade visual ideal, maior conforto e tempo de uso prolongado em pacientes com córneas irregulares após o LASIK.
Descritores: Lentes de contato; Cirurgia da córnea a laser; Paquimetria corneana; Perda de células endoteliais da córnea; Pressão intraocular
INTRODUCTION
Despite considerable advances in procedures for refractive surgery, some people still need spectacles or contact lenses to achieve optimal visual acuity after a procedure(1). Suboptimal visual quality after laser-assisted in situ keratomileusis (LASIK) can be caused by flap complications or laser correction errors, such as irregular ablation or improper centering of the ablation pattern on the eye. In such cases, problems with visual acuity may present as a consequence of corneal surface irregularities(2-4).
Different types of contact lenses may be used after LASIK surgery, including soft lenses, piggyback systems, hybrid lenses, and rigid gas-permeable (RGP) lenses (e.g., corneal, corneoscleral, or scleral contact lenses)(2). However, when corneal surface irregularities are marked, corneal RGP lenses provide the most effective masking option(5). When an abrupt transition zone exists between the flattened central zone and the peripheral cornea, these lenses can be manufactured using reverse geometry designs(6). In some instances, when neither corneal RGP nor other contact lenses can be well tolerated or when the resulting visual quality is inadequate, corneoscleral lenses (that rest partly on both the cornea and sclera) or scleral contact lenses (that rest entirely on the sclera) could prove viable options(7-9). Reports of scleral contact lenses being fitted on irregular corneas are common in the literature (e.g., for keratoconus, postintracorneal ring segment implantation, and postpenetrating keratoplasty). However, only a few studies have analyzed the fitting of corneoscleral contact lenses on eyes with corneal surface irregularities following surgery to correct refractive disorders(10-12).
In this study, we aimed to describe the outcomes after fitting corneoscleral contact lenses with multi-aspherical geometry designs (CScL-MAGD) to the eyes of patients with corneal surface irregularities after LASIK surgery.
METHODS
Study design
This was a retrospective study based on a small case series. We assessed visual acuity, subjective comfort, usage time, and corneal integrity after CScL-MAGD fitting in patients with corneal surface irregularities after LASIK surgery. The study design complied with the ethical requirements set by the University of Valencia and was conducted in accordance with the tenets of the Declaration of Helsinki. Only patients who consented to the use of clinical data for research purposes were included in the study.
Participants
We selected participants from a database of patients evaluated for wearing CScL-MAGD at FISABIO Oftalmología Médica between June 1, 2012, and January 30, 2014. Patients were included if they were Caucasian, older than 18 years, presented with unsatisfactory visual acuity when wearing contact lenses or spectacles after undergoing LASIK surgery for myopia correction, and had high levels of corneal surface irregularities. They were also required to have evidence of refractive problems either because of myopic regression or because their LASIK procedure was not completely successful. Patients were excluded if they had ocular surface disease or iatrogenic corneal ectasia. The minimum permitted time from LASIK surgery to CScL-MAGD fitting was six months.
Eye examinations
Contact lens wearers discontinued their use at least 15 days before fitting the CScL-MAGD. Thereafter, each patient underwent comprehensive eye examination, including best spectacle-corrected visual acuity, anterior eye biomicroscopy, ocular fundus examination, and corneal topographic analysis, including central corneal thickness (CCT), by using a Pentacam® HR Eye Scanner (Oculus Inc., Wetzlar, Germany). Furthermore, we measured corneal-compensate intraocular pressure (IOPcc) with an ocular response analyzer (Reichert Ophthalmic Instruments, Depew, NY) and measured the endothelial cell count (ECC) with a specular microscope (SP-3000P, Topcon Medical Systems Inc., Japan). These parameters were assessed again after one year of wearing CScL-MAGD.
Contact lens fitting
Following the first eye examination, patients were fitted with the CScL-MAGD (Scleracon, Lenticon, Madrid, Spain). These contact lenses were made of fluorosilicone acrylate (Optimum extreme, Contamac Ltd, Saffron Walden, UK), a highly gas-permeable material with an oxygen permeability (ISO) of 125 × 10-11 (cm2/s) (mLO2/(mL × mmHg)). They are based on a multi-aspherical geometry design with a base curve, an intermediate curve, and a peripheral curve. The average central thicknesses of the lenses used were 0.27 mm, and the ranges for the diameter, base curves, peripheral curves, and power were 12.60-13.50 mm, 5.80-9.20 mm (0.05 mm steps), 5.60-11.4 mm (0.10 mm increments), and +20.00 to -25.00 D (0.25 D increments), respectively. A plasma treatment was performed when these lenses were manufactured.
All contact lenses were fitted by a trial lens method. Two steps were needed to determine the appropriate lens (the base curve then the peripheral curve), following the manufacturer’s instructions. The fit was checked for good lens position, optimum lens movement (0.5 mm), and good tear exchange. At this stage, the fit had to show a slight alignment to minimal apical corneal clearance between the posterior surface of the contact lens and the anterior corneal surface, with no compression of the limbus and conjunctiva. The number of lenses ordered for each eye and the number of visits required to complete the fitting process were recorded for each patient.
Once the appropriate CScL-MAGD was determined, patients were instructed in lens care and handling. They were advised to increase lens wear times by one hour each day for a week, after which lens fit and visual acuity were rechecked. Follow-up assessments were performed at 1, 6, and 12 months. At these assessments, patients also reported their contact lens wear time (as hours/day) and subjective comfort (Likert scale: 1, very uncomfortable; 2, uncomfortable; 3, neither uncomfortable nor comfortable; 4, comfortable; 5, very comfortable).
Statistical analysis
Statistical analysis was performed using SPSS 15.0 software (SPSS Inc., Chicago, IL, USA). The nonparametric Wilcoxon signed-rank test was used to analyze the differences in visual acuity between the best spectacle-corrected value before CScL-MAGD fitting and the best visual acuity after fitting. Differences were analyzed in the same way for changes in CCT, ECC, and IOPcc from before wearing CScL-MAGD to one year after wearing CScL-MAGD. All visual acuity values were converted to a logMAR scale (logarithm of the minimum angle of resolution) for the statistical analysis. The threshold for statistical significance was taken as p<0.05. Data are reported as mean ± standard deviation or as absolute numbers unless otherwise stated.
RESULTS
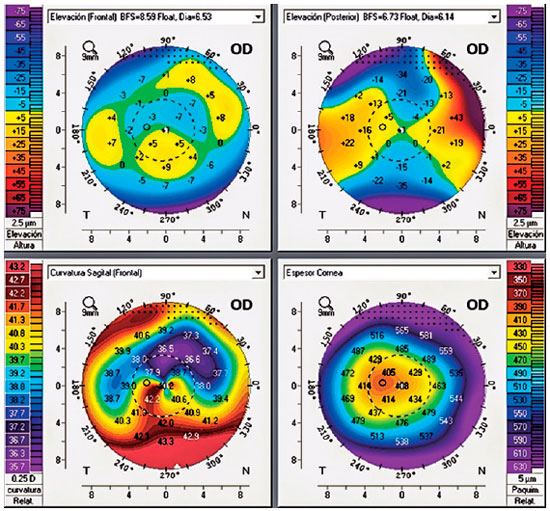
We identified 18 patients who met the inclusion criteria. Their mean age was 32 ± 4 years (range, 26-38 years), and all had unsatisfactory visual acuities after LASIK surgery when using either contact lenses (7 patients used soft toric lenses, and 5 patients used conventional corneal RGP contact lenses) or spectacles (6 patients). Corneal surface irregularities included irregularly irregular corneas (10 patients), decentered ablations (6 patients; Figure 1), and presence of a central island (2 patients). Unfortunately, three patients discontinued their CScL-MAGD use before completing the one-year follow-up period. The reasons were failure of improvement in vision (one case) and discomfort when wearing these contact lenses for more than 8 hours (two cases). Therefore, we only analyzed the outcomes for 24 eyes from 15 patients (8 females and 7 males).
Prior to CScL-MAGD fitting, the mean spherical equivalent with spectacles and the best spectacle-corrected visual acuity were -4.46 ± 2 D (range, -0.75 to -8.50 D) and 0.16 ± 0.05 logMAR (range, 0.3 to 0.1 logMAR), respectively. Furthermore, the mean CCT, ECC, and IOPcc values were 489.95 ± 17.69 µm (range, 420-510 µm), 2973.95 ± 144.32 cells/mm2 (range, 2700-3250 cells/mm2), and 16.73 ± 1.15 mmHg (range, 13.40-18.60 mmHg), respectively.
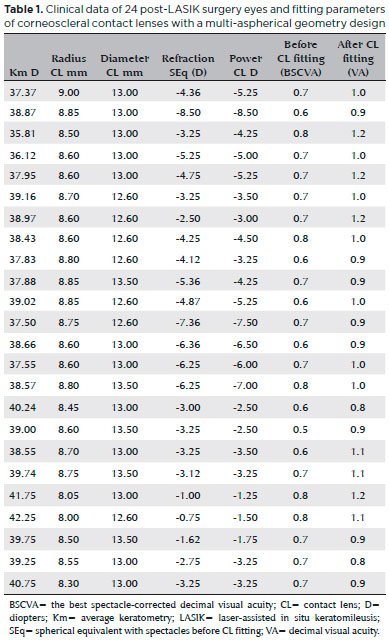
Table 1 shows the mean base curve, diameter, and power at CScL-MAGD fitting, which were 8.65 ± 0.24 mm (range, 8-9 mm), 12.9 ± 0.3 mm (range, 12.60-13.5 mm), and -4.69 ± 2 D (range, -1.25 to -8.50 D), respectively. Visual acuity improved to a statistically significant degree after CScL-MAGD fitting (0.01 ± 0.07; p<0.001). It should be noted that 16 eyes improved between 5 and 3 lines in decimal visual acuity and another 8 eyes between 2 and 1 lines.
An average of 2.9 visits (range, 2-4) was needed for successful CScL-MAGD fitting, and 18 eyes were fitted with the first lens that was ordered. All participants had optimal fitting outcomes in terms of lens position and lens movement. They also reported high subjective comfort ratings (17 patients rated lens use as comfortable or very comfortable) and prolonged usage times (12.98 ± 2.3 hours/day; range 10-17 hours).
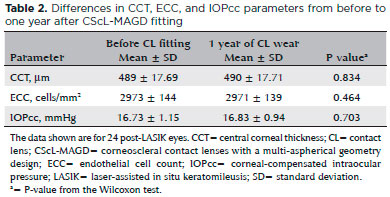
After one year of wearing CScL-MAGD, there were no statistically significant changes in the CCT, ECC, or IOPcc from before CScL-MAGD fitting (Table 2). Furthermore, visual acuity, subjective comfort, and usage times were maintained, and no adverse effects were found on the cornea.
DISCUSSION
After LASIK procedures, the patients had marked corneal surface irregularities with irregular topographic patterns; this finding is consistent with that of a previous study(4). These corneal surface irregularities can cause unsatisfactory vision because of decreased night vision, glare, halos, monocular diplopia, and ghosting, which in turn are associated with higher-order aberrations(4). In these cases, achieving optimal vision usually requires the use of corneal RGP lenses. The tear layer between the posterior surface of corneal RGP lenses and the anterior surface of the cornea plays an important role in compensating for corneal surface irregularities and irregular astigmatism(5).
In our study, patients were fitted with corneoscleral contact lenses because these lenses offer several advantages, including excellent comfort, centration, and stability, compared with corneal RGP lenses(7). Fitting corneoscleral or scleral lenses may be an appropriate option when corneal RGP lenses are poorly tolerated or unable to provide optimal visual quality(2,7,8). Factors such as lens flexure, excessive lens movement, decentered lenses, or reduced precorneal tear films can increase higher-order aberrations(13,14). Therefore, to improve visual quality, we offered CScL-MAGD fitting to patients reporting unsatisfactory visual acuity with their current contact lenses or spectacles.
Visual acuity improved significantly among the 15 patients who completed this study; this result is consistent with those of previous research(12,15). In a recent study with the same type of lenses, it was reported that the total number of higher-order aberrations decreased by approximately 78% (to normal levels) after CScL-MAGD fitting, thus implying significant improvement in the quality of vision when using these lenses. Gemoules et al.(12) fitted scleral contact lenses with reverse geometry designs on 17 eyes after postrefractive surgery. They reported that Snellen visual acuity improved from a mean of 20/25 (decimal equivalent 0.8) to 20/20 (decimal equivalent 1). These improvements in visual acuity were less than what we achieved, although it should be noted that the data cannot be compared like for like.
In this study, it was notable that patients reported high subjective comfort ratings and prolonged usage times and that these results were maintained during the follow-up period of one year. These favorable results could be due to several factors, including the lenses’ optimal fitting characteristics (in terms of centered position and stability) and the multi-aspherical geometry design (giving a more even distribution of the lens mass across the cornea).
Fitting a corneoscleral contact lens on an irregular cornea after LASIK surgery may prove challenging for eye practitioners. However, the process, number of visits, and number of lenses required for corneoscleral contact lens are comparable with those involved for corneal RGP contact lenses. Martin and Rodriguez(16) used 1.56 ± 0.53 corneal RGP lenses with a reverse geometry design to complete the fitting process for nine cases with irregular corneal surfaces after refractive eye surgery. Their data were in good agreement with ours, in which a mean of 1.26 ± 0.63 CScL-MAGD were requested. The base curve on average is 0.1 mm steeper than the mean obtained by keratometry (38.62 D, which is equivalent to a corneal radius of 8.75 mm and a mean base curve radius of 8.65 mm); this value is consistent with the manufacturer’s recommendations. Furthermore, we found a higher than expected minus power with the CScL-MAGDs induced by the lacrimal positive meniscus formed by the contact lenses (median spherical equivalent = -4.46 D; median lens power = -4.69 D). Overall, we determined that this was an efficient and effective process.
After one year of wearing CScL-MAGD, there were no statistically significant changes in corneal integrity (i.e., CCT or ECC values) or IOPcc from before CScL-MAGD fitting. These measurements were performed several minutes after removing the contact lenses such that potential problems, including corneal edema, could be detected immediately. Previous studies have suggested incorporating this procedure because most of the corneal edema tends to resolve in hours and cannot be detected if evaluation is delayed(17). Slit-lamp biomicroscopy also confirmed the lack of adverse ocular events, including hyperemia, vascularization, and corneal damage. The lack of complications may be related to the intrinsic lens characteristics, such as the high oxygen permeability of the material, the plasma treatment received (which increases lens wettability), and the use of small diameters compared with scleral lenses (which favor tear exchange)(18). Another advantage of the corneoscleral contact lenses used in this study was that they had even smaller diameters than other corneoscleral lenses, thus making them easy to handle. Furthermore, the corneoscleral contact lenses used in this study often did not require fluids for lens placement or a plunger for lens removal of the eye.
In summary, our results indicate that CScL-MAGD fitting on the irregular corneas of patients with persistent refractive errors after LASIK surgery can be a safe and effective alternative to glasses or other contact lens options. The method optimizes visual acuity, increases subjective comfort, and prolongs usage times. However, further studies with larger sample sizes are needed to confirm our results. It will also be interesting to determine the role of these lenses in other disorders associated with irregular corneas, such as keratoconus, penetrating keratoplasty, and corneal ring segment implantation.
REFERENCES
1. Food and Drug Administration (FDA). LASIK Quality of Life Collaboration Project (LQOLCP) [Internet]. FDA; 2014. [cited 2015 Jan 20]. Available from: http://www.fda.gov/downloads/MedicalDevices/ProductsandMedicalProcedures/SurgeryandLifeSupport/LASIK/UCM419443.pdf.
2. Steele C, Davidson J. Contact lens fitting post-laser-in situ keratomileusis (LASIK). Cont Lens Anterior. Eye (Lond). 2007;30(2):84-93.
3. Schallhorn SC, Amesbury EC, Tanzer DJ. Avoidance, recognition, and management of LASIK complications. Am J Ophthalmol. 2006; 141(4):733-9.
4. McCormick GJ, Porter J, Cox IG, MacRae S. Higher-order aberrations in eyes with irregular corneas after laser refractive surgery. Ophthalmology. 2005;112(10):1699-709.
5. Gemoules G. Therapeutic effects of contact lenses after refractive surgery. Eye Cont Lens. 2005;31(1):12-22
6. Tan G, Chen X, Xie RZ, He H, Liu Q, Guo Y, et al. Reverse geometry rigid gas permeable contact lens wear reduces high-order aberrations and the associated symptoms in post-LASIK patients. Curr Eye Res. 2010;35(1):9-16.
7. Van der Worp E, Bornman D, Ferreira DL, Faria-Ribeiro M, Garcia-Porta N, González-Meijome JM. Modern scleral contact lenses: A review. Cont Lens Anterior Eye. 2014;37(4):240-50.
8. Romero-Jiménez M, Flores-Rodríguez P. Utility of a semi-scleral contact lens design in the management of the irregular cornea. Cont Lens Anterior Eye. 2013;36(3):146-50.
9. The Scleral Lens Education Society. Scleral Lens Nomenclature [Internet]. The Scleral Lens Education Society; 2013. [cited 2015 Jan 16]. Available from: https://www.sclerallens.org/sites/default/files/files/SLS_Nomenclature_LtrHead06_26_2013.pdf.
10. Pecego M, Barnett M, Mannis MJ, Durbin-Johnson B. Jupiter scleral lenses: the UC Davis Eye Center experience. Eye Cont Lens. 2012; 38(3):179-82.
11. Severinsky B, Millodot M. Current applications and efficacy of scleral contact lenses - a retrospective study. J Optom. 2010;3(3): 158-63.
12. Gemoules G, Morris KM. Rigid gas-permeable contact lenses and severe higher-order aberrations in postsurgical corneas. Eye Contact Lens. 2007;33(6):304-7.
13. Choi J, Wee WR, Lee JH, Kim MK. Changes of ocular higher order aberration in on- and off-eye of rigid gas permeable contact lenses. Optom Vis Sci. 2007;84(1):42-51.
14. Efron S, Efron N, Morgan PB. Repeatability and reliability of ocular aberration measurements in contact lens wear. Cont Lens Anterior Eye. 2008;31(2):81-8.
15. Porcar E, España E, Montalt JC, Benlloch-Fornés JI, Peris-Martínez C. Post-LASIK Visual Quality With a Corneoscleral Contact Lens to Treat Irregular Corneas. Eye Contact Lens. 2017;43(1):46-50.
16. Martin R, Rodriguez G. Reverse geometry contact lens fitting after corneal refractive surgery. J Refract Surg. 2005;21(6):753-6.
17. Lu F, Xu S, Qu J, Shen M, Wang X, Fang H, Wang J. Central corneal thickness and corneal hysteresis during corneal swelling induced by contact lens wear with eye closure. Am J Ophthalmol. 2007; 143(4):616-22.
18. Michaud L, van der Worp E, Brazeau D, Warde R, Giasson CJ. Predicting estimates of oxygen transmissibility for scleral lenses. Cont Lens Anterior Eye. 2012;35(6):226-71.
Submitted for publication:
February 6, 2017.
Accepted for publication:
January 16, 2018.
Approved by the following research ethics committee: Universitat de Valencia (# H1445960985425)
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose