

José Lorenzo Romero-Trevejo; Navin Rachwani-Parshotam; María Josefa Morillo-Sánchez
DOI: 10.5935/0004-2749.20180049
ABSTRACT
A 44-year-old man was referred for evaluation of pain and temporal floaters after receiving a rebounded bullet impact to his right eye. Typical funduscopic findings, together with the confirmed presence of an intraorbital metallic foreign body, led to the diagnosis of chorioretinitis sclopetaria. Conservative management was performed as no severe symptoms were observed. The favorable clinical outcome was confirmed in subsequent reviews. Chorioretinitis sclopetaria is characterized by a proliferative chorioretinal inflammation as a consequence of the expansive wave caused by the entrance of a bullet between the eyeball and the orbit.
Keywords: Chorioretinitis; Chorioretinitis sclopetaria; Orbit; Eye foreign bodies; Trauma; Conservative treatment
RESUMO
Um homem de 44 anos foi encaminhado para avaliação de dor e flutuadores temporais após receber um impacto de bala ressaltado em seu olho direito. Achados fundoscópicos típicos, juntamente com a presença confirmada de um corpo estranho metálico intraorbitário, levaram ao diagnóstico de coriorretinite esclopetária. O manejo conservador foi realizado, pois não foram observados sintomas graves. O desfecho clínico favorável foi confirmado em revisões subsequentes. A coriorretinite esclopetária é caracterizada por uma inflamação coriorretiniana proliferativa como consequência da onda expansiva causada pela entrada de uma bala entre o globo ocular e a órbita.
Descritores: Coriorretinite; Coriorretinite esclopetária; Órbita; Corpos estranhos no olho; Trauma; Tratamento conservador
INTRODUCTION
First described by Goldzieher in 1901(1), chorioretinitis sclopetaria is an infrequent, specific, irreversible, and posttraumatic process characterized by proliferative chorioretinal inflammation as a consequence of the expansive wave and released energy after the entrance of a foreign body, usually a bullet, between the eyeball and the orbit. Rupture of the retina and choroid may be observed, while the sclera remains unaffected(2,3). We present a case of chorioretinitis sclopetaria caused by an intraorbital metallic foreign body, which is very infrequent in our environment, for which conservative management was performed.
CASE REPORT
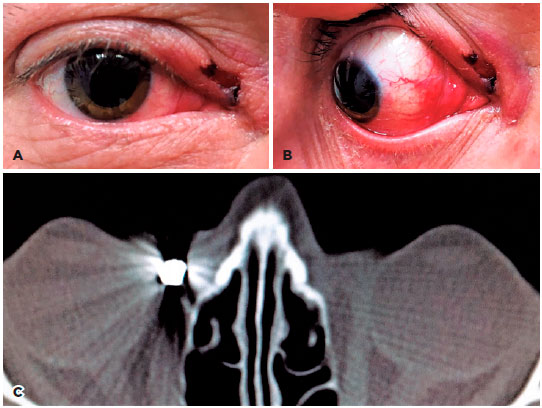
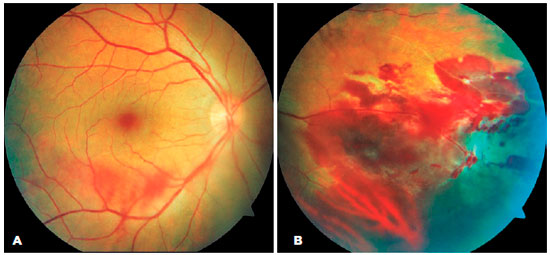
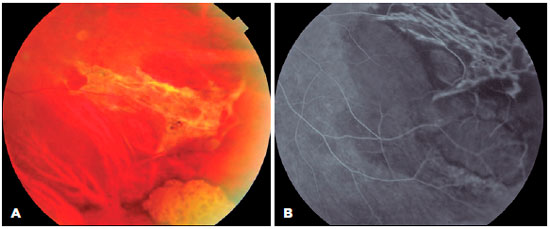
A 44-year-old man was referred for evaluation after receiving a rebounded bullet impact to his right eye an hour earlier. The patient complained of slight pain and temporal floaters. Examination showed a best corrected visual acuity of 20/20, an intraocular pressure of 22 mm Hg, and an isochoric and normoreactive pupil. The affected eye preserved extraocular movements, and no diplopia was observed. Slit-lamp examination revealed the presence of a 3-mm-long incised wound located in the internal cantus and parallel to the upper lid margin. The lacrimal canaliculus was not affected (Figure 1A). In addition, bulbar conjunctival hyperemia in the nasal quadrant and chemosis of the caruncle were detected (Figure 1B). Funduscopic examination revealed a normal macula and dispersed preretinal hemorrhages in the lower vascular arch (Figure 2A). Peripheral contusive edema, preretinal and subretinal hemorrhages in the nasal and inferonasal regions, and vitreous hemorrhage were also observed (Figure 2B). Optical coherence tomography did not show any pathological findings in the macula or optic nerve. Computed tomography of the orbit detected the presence of a 4-mm-long intraorbital, extraocular, and extraconal metallic foreign body adjacent to the medial eyeball side and to the insertion of the internal rectus. The size and morphology of both eyeballs were conserved (Figure 1C). The patient was admitted to the Maxillofacial Surgery Department for evaluation, where conservative management was recommended. This included a 2-week course of oral amoxicillin-clavulanic acid and a 1-month tapering dose of topical tobramycin-dexamethasone. Subsequent reviews after 1, 2, and 4 weeks confirmed the complete disappearance of the symptoms. A progressive decrease in size of the funduscopic lesions was observed. Campimetry and fluorescein angiography (Figure 3A, B) were performed after 2 months, and the results demonstrated good morphological and functional evolution of the healing process.
DISCUSSION
The decision to manage our patient conservatively was based on the location of the foreign body, the type of lesions found in the affected eye, and the absence of severe symptoms. Given the improvement obtained on subsequent reviews, this decision proved to be appropriate. Bullet impacts in the facial region are found predominantly in the maxillary, frontal, ethmoidal, and sphenoidal sinuses, in order of frequency. Impacts on the orbit, as in our patient, are infrequent(3). Due to both restriction of and direct damage to the extraocular muscles, such impacts may result in alterations of ocular motility(4). These effects were not observed in our patient. Surgical removal of the fragment would have been justified if they had been. When a foreign body is inaccessible, is located near any vital structure, or produces no symptoms, conservative management is recommended, including periodic monitoring. This approach was taken in our patient, since surgery could have produced undesired secondary alterations(3,5).
Chorioretinitis sclopetaria usually leads to the formation of fibrous scars and pigmentary alterations of the retina, which are the final findings in these cases(2-4). Acute retinal detachment is infrequent(3,4,6). However, in cases of macular involvement, the visual prognosis may be poor due to progressive scarring(7). In our patient, chorioretinal lesions were located in the nasal and inferonasal periphery, and the retina remained attached. These were the reasons for the intact visual acuity maintained up to the last review.
The damage caused by these processes depends on the type of projectile, the distance from which the shot is made(3-5), the initial velocity of the projectile, the existence of rebound, and the intention of the trigger(3,4). Projectiles frequently remain incarcerated in the orbit if their initial velocity was low, they were shot from a long distance, or there were intermediate impacts that slowed them down(3). In our patient, the impact occurred after the rebound of the bullet, which probably reduced its velocity and resulted in its superficial location between the eyeball and the medial wall of the orbit. This caused little extraocular damage and resulted in a better prognosis.
In conclusion, chorioretinitis sclopetaria is a process that requires a multidisciplinary approach to select the best treatment in each case(8). Retinal, neuroophthalmological, and oral and maxillofacial surgery specialists should be in charge of choosing between conservative management or a more aggressive treatment in order to achieve a better visual prognosis and to minimize the appearance of secondary complications in the long term.
REFERENCES
1. Goldzieher W. A study for the pathology of orbital gunshot traumas. Z Augenheilkd. 1901;6:227.
2. Igal V, Pikkel-Igal YS, Pikkel YY. Chorioretinitis sclopetaria: a case report. Case Rep Ophthalmol. 2017;8(1):137-40.
3. Clarós P, Fokouo JV, Clarós A. Intraorbital foreign body: A rifle bullet removed 20 years after the accident. Eur Ann Otorhinolaryngol Head Neck Dis. 2017;134(1):63-5.
4. Ramos IC, Santos DC, Soares I, Cerqueira V. Chorioretinitis sclopetaria. Rev Bras Oftalmol. 2015;74(3):178-82.
5. Al-Amry M, Al-Taweel H, Al-Enazi N, Alrobaian M, Al-Othaimeen S. Retained periorbital and intracranial air-gun pellets causing sclopetaria and visual loss. Saudi J Ophthalmol. 2014;28(3):228-33.
6. Fraser EJ, Haug SJ, McDonald HR. Clinical presentation of chorioretinitis sclopetaria. Retin Cases Brief Rep. 2014;8(4):257-9.
7. Papakostas TD, Yonekawa Y, Skondra D, Vavvas DG. Traumatic chorioretinal rupture (sclopetaria). Int Ophthalmol Clin. 2013; 53(4):119-25.
8. Mondino MA, Remis F, Magurno M. Coriorretinopatia esclopetaria: comunicación de un caso y revisión de la literatura. Oftalmol Clín Exp. 2008;2:113-5.
Submitted for publication:
March 13, 2018.
Accepted for publication:
March 20, 2018.
Funding: No specific financial support was available for this study
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose