

Caner Kara; İkbal Seza Petriçli
DOI: 10.5935/0004-2749.20180034
ABSTRACT
During the routine ophthalmologic examination of a 38-day old female infant, indirect ophthalmoscopy revealed a dense hemorrhage on the fovea and a couple of superficial hemorrhages in the nasal retina of the left eye. No hemorrhage was observed in the right eye. A hand-held spectral domain optical coherence tomography (SD-OCT) was used at the time of diagnosis. The hemorrhage at the nasal retina resolved in the first week of follow-up, and the foveal hemorrhage resolved 12 weeks after birth. Spectral domain optical coherence tomography was repeated once the foveal hemorrhage had resorbed, and it showed that the foveal contour had reformed without any sequelae. This case suggests that birth-related foveal hemorrhages do not cause any disturbance in the foveal architecture.
Keywords: Fovea centralis; Retinal hemorrhage; Optical coherence tomography; Infant
RESUMO
Durante o exame oftalmológico de rotina de uma criança do sexo feminino de 38 dias, a oftalmoscopia indireta revelou uma hemorragia densa na fóvea e algumas hemorragias superficiais na retina nasal do olho esquerdo. Nenhuma hemorragia foi observada no olho direito. Foi utilizada uma tomografia de coerência óptica de domínio espectral no momento do diagnóstico. A hemorragia na retina nasal foi resolvida na primeira semana de acompanhamento e a hemorragia foveal foi resolvida em 12 semanas após o nascimento. A tomografia de coerência óptica de domínio espectral foi repetida uma vez que a hemorragia foveal foi reabsorvida, e mostrou que o contorno foveal havia se reformado sem sequelas. Este caso sugere que as hemorragias foveais relacionadas ao nascimento não causam qualquer distúrbio na arquitetura foveal.
Descritores: Fóvea central; Hemorragia retiniana; Tomografia de coerência ótica; Lactente
INTRODUCTION
Birth-related retinal hemorrhages are seen at a rate of 2.6%-50% based on variables such as the time and technique of examination. They are mostly located in the posterior pole and are usually intraretinal(1) but can also be subretinal or preretinal. Most hemorrhages resolve spontaneously within a couple of weeks(2).
Macular hemorrhages are less common than extramacular ones, and they take longer to resolve(2). Additionally, hemorrhages involving the macula are more important in terms of the risk of development of deprivation amblyopia and hemorrhage-related retinal toxicity.
Most studies have clinically evaluated retinal hemorrhages because the patients were in the pediatric age group. However, it is now possible to use portable hand-held spectral domain optical coherence tomography (SD-OCT) devices allowing high-resolution and non-invasive imaging of the retina for these patients(3). Here, we discuss the case of an infant with foveal hemorrhage and its resolution, as demonstrated by OCT images. To the best of our knowledge, this is the first report of OCT used to evaluate a neonatal foveal hemorrhage.
CASE REPORT
A female infant born after 37 weeks of gestation via normal spontaneous vaginal delivery, with a birth weight of 2390 g, was referred for a general eye examination 38 days after birth. The history of the patient revealed that her birth was the first one of her 18-year-old mother. No induction had been performed and no assistance, such as forceps or vacuum, had been used during delivery.
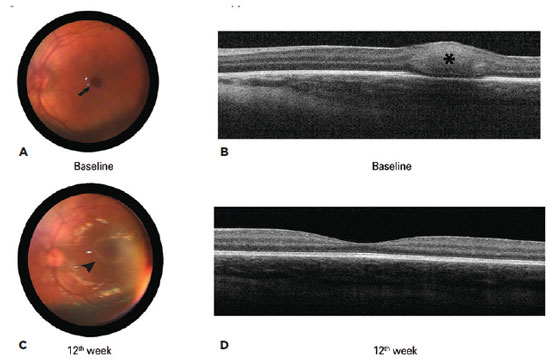
Indirect ophthalmoscopy after pupil dilation revealed a dense hemorrhage the size of half of the diameter of the optic disc on the fovea and some superficial hemorrhages in the nasal retina of the left eye. No hemorrhage was observed in the right eye in the detailed retinal examination. The findings were documented with video indirect ophthalmoscopy (Omega 2C, Heine, Germany). SD-OCT (iVue; Optovue, Fremont, USA) was also performed to evaluate the hemorrhage in more detail. SD-OCT was performed in the supine position with the arms and body of the patient held by the nurse. No sedation was used. A 6 mm × 6 mm retinal thickness map scan protocol comprising a raster pattern of seven horizontal lines was used. Central foveal thickness is defined as the average thickness of the central 1-mm ring of the macular map as defined by the Early Treatment Diabetic Retinopathy Study. On OCT performed at the time of diagnosis, a horizontal foveal cross-section of the left eye showed a lack of the foveal contour and a hyper-reflective dome-shaped lesion corresponding to the area of blood seen clinically. The central foveal thickness was 391 µ at the time of diagnosis. Representative indirect ophthalmoscopy and OCT images of the left eye are shown in figure 1.
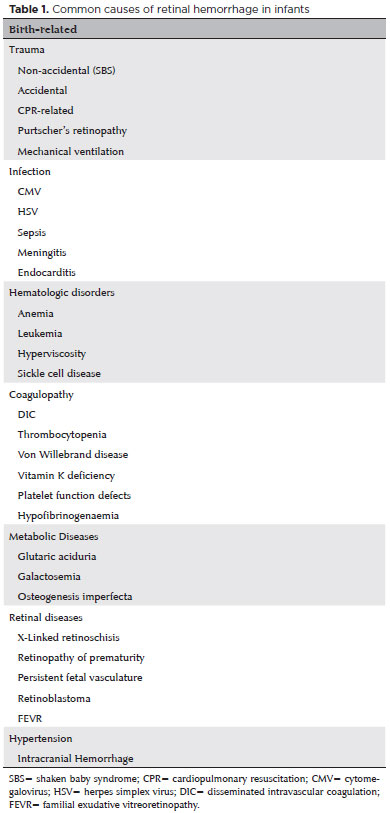
We did a systemic work-up to rule out other causes of retinal hemorrhage, such as accidental or non-accidental injury or hematological and cardiovascular disorders; we found no other abnormalities. The causes of retinal hemorrhage considered in the differential diagnosis are listed in table 1.
The family was informed that there was no need for any treatment and that self-resolution was expected but that follow-up would be needed as the hemorrhage might lead to foveal dysfunction.
The hemorrhage at the nasal retina had resolved at the time of the 1-week follow-up, and the foveal hemorrhage had resolved 12 weeks after birth. SD-OCT was repeated at this time and showed a normal foveal contour without any disturbances and a central foveal thickness reduced to 161 µ (Figure 1). The parents were asked to bring the patient back for a 6-month follow-up.
DISCUSSION
Most birth-related retinal hemorrhages are located bilaterally on the posterior pole, which has rich retinal vascularity and a thick nerve fiber layer. They are mostly resolved within the first month(4). In our case, we suspect that if we had seen the patient right after birth (we first saw the patient 38 days after birth), the hemorrhage would have been much more severe and possibly bilateral.
Macular hemorrhages on the posterior pole are more important clinically because they take longer to resolve and may cause toxic and mechanical damage to the retina. For example, granular macular changes after the resolution of macular hemorrhages have been reported in a neonate(5).
In a cohort of 53 neonates with retinal hemorrhage, only two cases (3.8%) were found to have foveal hemorrhages; all hemorrhages resolved spontaneously within 16 days except the two foveal cases, which took 22 and 31 days to get resolved(4). In another study with 34 pediatric macular hemorrhages, classified as foveal or extrafoveal, only six were foveal (the study did not report resolution times)(6). The rate of macular hemorrhages has been reported to be 17% and the rate of foveal hemorrhages 2.72% in a large cohort of 1199 newborns (this study did not report resolution times either)(7). In addition, a case of retinal and foveal hemorrhages in a newborn delivered by vacuum extraction was reported as resolved completely within 5 weeks(8).
In our case, the foveal hemorrhage took 12 weeks to resolve, longer than that in the literature reports(4,7). Although the reason for this is unclear, it may be because of the location of the hemorrhage; our patient's hemorrhage was located intraretinally, as evidenced with the OCT, and not just on the surface of the retina.
The few reports evaluating retinal hemorrhages in infants using OCT have referred to patients with shaken baby syndrome (SBS). The first one of such reports evaluated an infant with a full-thickness macular hole with retinal scarring and another infant with a double layer of epiretinal membrane(3). Other OCT findings, including retinoschisis, disruption of the foveal architecture, foveolar detachment, disinsertion of the internal limiting membrane, and cavity overlying the macula, have also been reported in patients with SBS(9,10). The mechanical and toxic effects of the retinal hemorrhages have been thought to be the cause of the retinal findings seen in patients with SBS. Although we did not observe any disturbances in the foveal architecture due to the hemorrhage in our case, the pathogenesis of SBS is different from that in our case.
Although we performed OCT in this study to determine whether a foveal disturbance had developed, using OCT at the time of diagnosis can also facilitate the differential diagnosis for retinal hemorrhages. For example, OCT could help identify conditions that affect the retinal structure in addition to causing hemorrhages in newborns (such as SBS and retinoschisis), as listed in table 1.
In conclusion, we describe the case of an infant with a foveal hemorrhage that resolved by the 12th week (it took longer than the time taken in other reports). Using OCT, we were able to show the precise location of the hemorrhage inside the retinal layer and demonstrate that there was no disruption of the foveal architecture after resolution.
REFERENCES
1. Watts P, Maguire S, Kwok T, Talabani B, Mann M, Wiener J, et al. Newborn retinal hemorrhages: a systematic review. J AAPOS. 2013; 17(1):70-8. Erratum in: J AAPOS. 2013;17(3):341.
2. Emerson MV, Pieramici DJ, Stoessel KM, Berreen JP, Gariano RF. Incidence and rate of disappearance of retinal hemorrhage in newborns. Ophthalmology. 2001;108(1):36-9.
3. Scott AW, Farsiu S, Enyedi LB, Wallace DK, Toth CA. Imaging the infant retina with a hand-held spectral-domain optical coherence tomography device. Am J Ophthalmol. 2009;147(2):364-73. Comment in: Am J Ophthalmol. 2009;147(6):1102; author reply 1102-3.
4. Hughes LA, May K, Talbot JF, Parsons MA. Incidence, distribution, and duration of birth-related retinal hemorrhages: a prospective study. J AAPOS. 2006;10(2):102-6.
5. Paris CL, Peyman GA, Breen C, Blinder KJ. Neonatal macular hemorrhage. Int Ophthalmol. 1991;15(3):153-5.
6. Callaway NF, Ludwig CA, Blumenkranz MS, Jones JM, Fredrick DR, Moshfeghi DM. Retinal and optic nerve hemorrhages in the newborn infant: one-year results of the Newborn Eye Screen Test Study. Ophthalmology. 2016;123(5):1043-52.
7. Zhao Q, Zhang Y, Yang Y, Li Z, Lin Y, Liu R, et al. Birth-related retinal hemorrhages in healthy full-term newborns and their relationship to maternal, obstetric, and neonatal risk factors. Graefes Arch Clin Exp Ophthalmol. 2015;253(7):1021-5.
8. Naderian G, Fesharaki H, Sajjadi V, Naderian MA. Retinal hemorrhages in a neonate following vacuum extraction. J Ophthalmic Vis Res. 2013;8(2):179-81.
9. Muni RH, Kohly RP, Sohn EH, Lee TC. Hand-held spectral domain optical coherence tomography finding in shaken-baby syndrome. Retina. 2010;30(4 Suppl):S45-50.
10. Koozekanani DD, Weinberg DV, Dubis AM, Beringer J, Carroll J. Hemorrhagic retinoschisis in Shaken Baby Syndrome imaged with spectral domain optical coherence tomography. Ophthalmic Surg Lasers Imaging. 2010;9:1-3.
Submitted for publication:
October 6, 2017.
Accepted for publication:
November 23, 2017.
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.