

Alper Mete1; Sabit Kimyon1; Oguzhan Saygılı1; Kıvanç Güngör1; Mithat Temizer2
DOI: 10.5935/0004-2749.20180023
ABSTRACT
Purpose:To compare the use of topical anesthesia and retrobulbar anesthesia during silicone oil removal with a mixed pars plana technique, through evaluating the pain experience of patients.
Methods: We selected patients according to their behavior during previous vitreoretinal surgery and ophthalmologic examinations and divided them into two anesthesia groups: topical (n=36) and retrobulbar (n=33). We used a mixed technique for the passive removal of silicone oil in both groups. During each step of the surgery, the patients' pain experience and the surgeon's comfort were scored according to a pain scale.
Results: The pain experienced during the application of the anesthesia was significantly greater in the retrobulbar group (p<0.001). The topical group experienced greater pain during trocar insertion (p<0.001). There was no significant difference between the groups regarding the overall pain experience or complications.
Conclusions: The pain experience of the selected patients during silicone oil removal was comparable between the topical and the retrobulbar anesthesia. Topical anesthesia with the mixed pars plana technique is an effective and safe alternative option for silicone oil removal surgery.
Keywords: Pain; Silicone oils; Anesthetics, local; Administration, topical; Vitreoretinal surgery; Patient satisfaction
RESUMO
Objetivo: Comparar a sensação de dor de pacientes durante a remoção do óleo de silicone sob anestesia tópica e retrobulbar, usando uma técnica via pars plana combinada.
Métodos: Os pacientes foram selecionados, de acordo com suas atitudes durante cirurgia vitreorretiniana prévia e exames oftalmológicos, e divididos em dois grupos: anestesia tópica e retrobulbar. Para a remoção passiva do óleo de silicone, utilizouse uma técnica combinada em ambos os grupos. A sensação de dor dos pacientes e o conforto do cirurgião foram classificados através de uma escala de dor durante cada etapa da cirurgia.
Resultados: Os grupos anestesia tópica e retrobulbar incluíram 36 e 33 pacientes, respectivamente. A sensação de dor durante a aplicação da anestesia foi significativamente maior no grupo retrobulbar (p<0,001). O grupo anestesia tópica sentiu mais dor durante a inserção do trocarte (p<0,001). Não houve diferença significativa entre os grupos em relação à sensação geral de dor e a complicações.
Conclusões: A sensação de dor é comparável entre a anestesia tópica e a retrobulbar durante a remoção de óleo de silicone. A combinação de anestesia tópica e uma técnica via pars plana é uma opção alternativa eficaz e segura para a cirurgia de remoção de óleo de silicone.
Descritores: Dor; Óleos de silicone; Anestésicos locais; Administração tópica; Cirurgia vitreorretiniana; Satisfação do paciente
INTRODUCTION
During vitreoretinal surgery for complex cases, surgeons generally use silicone oil tamponade(1). Its advantages include quick visual rehabilitation, long-term tamponading of the reattached retina, and relatively stable chemo-physical properties(2,3). However, its use is associated with several complications, including cataracts, keratopathy, corneal endothelial decompensation, glaucoma, and hypotony. It is therefore recommended that the silicone oil is removed as soon as possible after achieving retinal stability(3-6).
Various surgical techniques to remove the silicone oil have been reported(7-10). Transconjunctival sutureless systems result in faster healing, do not require sutures, and result in less discomfort to the patient. However, the passive removal of silicone oil can prolong the operation time during minor sclerotomies, whereas the active vacuum suction needed commonly to extract the silicone oil carries the risk of eyeball collapse or retinal damage(7-9). A further technique that has been reported for silicone oil removal is the mixed 23-gauge infusion and 20-gauge pars plana vitrectomy method(10); 20-gauge sclerotomy is considered to be an efficient, fast, and inexpensive alternative to the passive removal of silicone oil of high or low viscosity.
Injection anesthesia methods are commonly used in posterior vitrectomy procedures(11,12). However, these methods can lead to serious needle-related complications(13,14). Topical anesthesia has been used for cooperative patients as an alternative to other local anesthesia techniques in vitreoretinal surgery; it has the advantages of being non-invasive, early visual recovery, and ease of administration(11-13).
The purpose of this study was to compare retrobulbar anesthesia and topical anesthesia in terms of the pain experience of patients and the comfort of the surgeon during the passive removal of silicone oil using a mixed 23-gauge 20-gauge technique. There have been only a few previous reports of the use of topical anesthesia for silicone oil removal, and this is the first report to evaluate the pain experience of patients during such use.
METHODS
Study
This prospective comparative study included 69 patients operated with a mixed pars plana technique for 1000 centistoke (cSt) passive silicone oil removal under topical or retrobulbar anesthesia at the Department of Ophthalmology, Gaziantep University Hospital, Turkey. This study received local ethics committee approval. The procedures were explained to the patients, and they were told they may experience some pain during silicone oil removal and the administration of the retrobulbar block; all patients subsequently provided written informed consent.
Patients
A total of 69 patients who had experienced a comfortable and calm previous vitreoretinal surgery under local anesthesia and preoperative ophthalmologic examination were included. All were older than 20 years and had undergone a previous combination of phacoemulsification cataract surgery and posterior vitrectomy with silicone oil (1000 cSt) tamponade for retinal detachments (rhegmatogenous retinal detachments, diabetic tractional retinal detachments, or non-diabetic tractional retinal detachments). In addition, the intraocular silicone oil had been in place for at least four months with a stable retina. The exclusion criteria were age younger than 20 years, being phakic or aphakic, redetachments, hypotony (intraocular pressure (IOP) ≤10 mmHg), extreme anxiety, claustrophobia, speech disorder, ocular infection, and a known allergy to topical or retrobulbar anesthetic drugs. The participants were matched according to indications for silicone oil tamponade and an experienced surgeon (A.M.) distributed them randomly between the two anesthesia groups: the topical group (n=36) and the retrobulbar group (n=33).
Surgical procedures and pain–discomfort scoring
A single experienced vitreoretinal surgeon (O.S.) performed all surgeries. For the topical group patients, the surgeon administered topical 0.5% proparacaine hydrochloride drops into the conjunctival sac four times in the 15 minutes preceding surgery, with additional drops administered every 5 minutes throughout the duration of the procedure. During the silicone oil removal, the participants were asked to tell the surgeon if they felt intolerable pain, with additional subtenon anesthesia ready prepared for such an eventuality. For the retrobulbar group patients, a mixture of 3 mL 5% bupivacaine and 3 mL 2% lidocaine was injected into the retrobulbar space using an 0.5-inch 26-gauge needle. Neither patient group received sedation, although we gave an oral analgesic to uncomfortable patients postoperatively. All patients received nasal oxygen (4 L/min) during the procedure.
Povidone iodine (5%) was used to clean the eye and periocular area. Anesthetic status was checked by grasping the bulbar conjunctiva using colibri forceps after draping and insertion of the eye speculum(18). Then, an inferotemporal transconjunctival sclerotomy was created 3.5 mm posterior to the limbus by using 23-gauge trocar cannula, and a 23-gauge infusion cannula was connected to the vitrectomy system (Dutch Ophthalmic Research Center, Zuidland, The Netherlands). A second transconjunctival sclerotomy was created 3.5 mm posterior to the limbus with a 20-gauge blade (0.89 mm), either superonasal or superotemporal at the surgeon's discretion, and a 20-gauge trocar cannula system was inserted. When no additional procedures were needed, only two sclerotomies were made. Otherwise, an additional sclerotomy was created using a 23-gauge trocar cannula system. In all cases, to reduce the patient's pain and discomfort, the trocars were inserted directly at an angle of approximately 90° to the sclera without displacing the conjunctiva.
A silicone oil-fluid exchange was then performed. In the retrobulbar group, the eyeball was tilted to clear the residual small oil bubbles using colibri forceps. In the topical group, the surgeon instructed the patient to move his or her eyes in the directions needed to clear the residual small silicone oil bubbles. The cannulas were the removed and the IOP was checked. Finally, all the sclerotomies were closed with 8-0 absorbable sutures. A topical antibiotic drop was instilled in the conjunctival sac. The operative time was recorded.
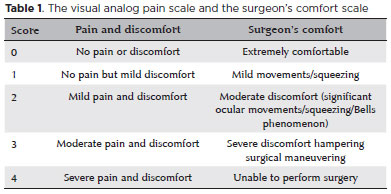
The pain experienced by the patient was scored using a visual analog pain scale (VAPS) at several timepoints: as the anesthesia was administered, during each step of the surgery, and immediately after surgery (Table 1)(11,12). If the patient was unable to see the chart because of low vision, he or she was asked for an oral score. The surgeon's comfort was also scored using a surgeon's comfort scale. Each patient underwent follow-up ocular examinations on the first postoperative day and at the end of the first week and first month.
Data analysis
All statistical analyses were performed using SPSS 16.0 software (SPSS Inc, Chicago, IL). Patient characteristics, clinical characteristics, clinical outcomes, pain scores, and the surgeon's comfort scores were compared between the two anesthesia groups using Mann-Whitney U, chi-square, and paired samples t tests. A p value less than 0.05 was considered statistically significant.
RESULTS
Table 2 presents the patients' characteristics, indications for silicone tamponade, duration of silicone tamponade, operative times, additional procedures during surgery, and preoperative and postoperative best-corrected visual acuity (BCVA). There was no significant difference between the two groups with regard to age, sex, laterality, distribution of indications for silicone tamponade, duration of silicone tamponade, operative time, distribution of additional procedures, or preoperative and postoperative BCVA.
The mean pain scores during the administration of anesthesia differed significantly between the groups (p<0.001). In the retrobulbar group, 28 of the 33 patients (85%) scored grade 2 and five (15%) scored grade 3 pain as the retrobulbar block was administered, with a mean pain score of 2.15 ± 0.36. In the topical group, none of the patients reported any pain sensation as the topical anesthesia was administered. The mean pain scores for all the surgical steps for the topical and retrobulbar groups are shown in tables 3 and 4, respectively.
During trocar insertion, 27 of the 36 patients (75%) in the topical group scored grade 2, seven (19%) grade 3, and two (6%) grade 1 pain; in contrast, only 3 of the 33 patients (9%) in the retrobulbar group scored grade 1 pain. The mean pain scores during trocar entry differed significantly between the groups (p<0.001). However, there was no statistically significant difference between the groups during the passive removal of silicone oil, cannula removal, or the sclerotomy suturing steps of the surgery (p=1.000, p=0.173, and p=0.06, respectively).
The mean ( ± SD) comfort score of the surgeon was 0.11 ± 0.40 for the topical group. With the retrobulbar group, the surgeon performed all the procedures with extreme comfort (Grade 0). There was no significant difference in the overall pain and discomfort scores (for anesthesia administration and surgery) or the surgeon's comfort scores between the groups (p=0.448 and p=0.092; respectively). In both groups, the postoperative mean BCVA increased or remained the same when compared with the preoperative BCVA. Postoperative BCVA was not changed in seven eyes (19%) in the topical group and in six eyes (18%) in the retrobulbar group.
Additional subtenon anesthesia was not required in any case. None of the patients required oral analgesic or sedation during surgery or postoperatively. Postoperatively, we observed no ocular hypotony or leakage in either group during the follow-up period. We observed injection anesthesia-related mild lid edema in three patients (9%) in the retrobulbar group. Two patients (6%) in the topical group and two (6%) in the retrobulbar group underwent reoperation because of recurrent retinal detachment.
DISCUSSION
Several surgical techniques have been described for silicone oil removal(7-10,15,16). Surgeons commonly prefer transconjunctival sutureless systems for silicone oil removal because these systems are less invasive, faster, and more comfortable for the patient than 20-gauge systems( 5,7,9,15,17). Silicone oil removal can be performed by the anterior route in aphakic or pseudophakic patients or along with cataract extraction(18-20). Cacciatori et al.(18) reported that the anterior route is more advantageous because it allows the silicone oil to be removed under topical anesthesia, eliminating the potential risks of injection anesthesia and sclerotomy-related complications( 18). However, the anterior route has some limitations in complex posterior vitrectomy procedures, anatomically limiting surgical maneuvers during these procedures( 18-20). For these cases, the pars plana approach is usually preferred by surgeons because it simplifies the complete evaluation of the peripheral retina during surgery and the additional procedures(7-10,15-20). In our study, we used the two-port pars plana technique for silicone oil removal. For additional procedures, we created an additional sclerotomy using a 23-gauge trocar system. Tan et al.(21) compared two-port and three-port approaches for silicone oil removal and reported no significant difference between them with regard to the recurrent retinal detachment rate. In contrast, Guo et al.(22) showed that the incidence of recurrent retinal detachment rate was significantly higher with the two-port than with the three-port technique. The incidence of recurrent retinal redetachment in conventional 20-gauge silicone oil removal surgery has been reported as nearly as 20%(23,24). In our study, the incidence of recurrent retinal detachment with the passive removal of silicone oil using the two-port mixed technique was 6% in both groups. We believe that the low incidence of recurrent detachment in our study was associated with several factors, including performing the silicone oil removal procedures passively in all cases without the use of a powered vacuum system, with its risk of retinal injuries, and suturing all sclerotomies in all patients after the silicone oil had been removed. In this way, we prevented potential ocular hypotony due to leakage. The reported incidence of postoperative ocular hypotony ranges from 0% to 3.8% after 23-gauge transconjunctival procedures(25-27). However, we did not observe any ocular hypotony in either group during the postoperative period.
Compared with 20-gauge systems, 25-gauge systems and instruments are more expensive and generally require a powered suction device for active silicone oil removal, as well as a prolonged learning curve for the surgeon(15,28). In contrast, 20-gauge systems and instruments are more comfortable and efficient, less expensive, and faster when performing additional procedures. Furthermore, 20-gauge systems do not generally require powered suction for the silicone oil removal, and they are more effective and faster than transconjunctival sutureless systems for the removal of high-density silicone oil(7,10). Active suction for silicone oil removal carries the risk of optic nerve injury or eyeball collapse due to the high vacuum pressure(10). In addition, 23-gauge systems are widely used for silicone oil removal(7,10,15), and some authors have proposed techniques that combine different systems. Lei et al.(10) described a quick and simple mixed pars plana technique using a 23-gauge entry for infusion combined with a 20-gauge entry, which they used to remove 5700-cSt silicone oil for 29 patients. They reported no serious complications during surgery and only one recurrent retinal detachment during the follow-up period. Our outcomes were similar with the findings of that report; we experienced no serious complications during surgery in either of our groups(10).
Topical anesthesia is a useful alternative option for selected patients in posterior vitrectomy procedures(11-13). The well-established advantages of topical anesthesia are the absence of needle complications, fast visual recovery, and easy administration(11-13). Our experience suggests that the two-port mixed pars plana approach is the most appropriate, suitable, and comfortable technique for using with topical anesthesia for silicone oil removal procedures. This mixed technique with topical anesthesia has advantages over other techniques. First, it provides quick and easy removal of silicone oil of various densities through the 20-gauge trocar port. Second, the use of 20-gauge instrumentation provides cost-effective and fast surgery that is comfortable for the surgeon. Third, eye movements during surgery are helpful for the faster removal of silicone oil and air bubbles, and they allow the adequate evaluation of the peripheral retina during surgery without the need for scleral indentation; however, they can result in iatrogenic complications. Surgical instruments passing through the trocars are useful for the surgeon because they limit sudden eye movements and can provide eye movement in desired directions during the procedures. In the present study, we did not experience any complications during surgery.
The assessment o(11-13)f the patients' pain and discomfort while using topical anesthesia is helpful for following up and for improving the quality of pre- (e.g. deciding premedication usage), post-, and intraoperative care(29). Pain and discomfort are not objective signs of the quality of anesthetic care; nevertheless, the scored pain values help with evaluating the outcomes from the patient's perspective(30). We thought that patient selection and surgeon experience played key roles for a comfortable and uncomplicated silicone oil removal surgery under topical anesthesia. The surgeon's comfort scores did not differ between the retrobulbar and topical groups in our study; however, it was not possible to blind the surgeon to the anesthesia type so there may have been some bias.
The requirement for sedation is another controversial issue associated with silicon oil removal procedures(11). As previously reported, sedation may cause serious complications, such as respiratory depression or cardiopulmonary complications(11). We thought that sedation would be required for a very small number of patients during silicone oil removal under topical anesthesia. Patient selection considerably reduced the requirement for sedation; in this study, sedation was not used in either group preoperatively or intraoperatively. Nevertheless, we kept additional subtenon anesthesia readily available for potential challenges during the surgery.
In conclusion, topical anesthesia provides an alternative option for silicone oil removal. We observed comparable pain scores and surgeon's comfort scores with both topical and retrobulbar anesthesia. Our experience also suggested that the mixed pars plana technique is the most suitable for silicone oil removal under topical anesthesia. Patient selection plays critical role for silicone oil removal under topical anesthesia. To the best of our knowledge, this report is the first on the patients' pain experience during silicone oil removal using a mixed technique under topical anesthesia.
REFERENCES
1. Krepler K, Mozaffarieh M, Biowski R, Nepp J, Wedrich A. Cataract surgery and silicone oil removal: visual outcome and complications in a combined vs. two step surgical approach. Retina. 2003; 23(5):647-53.
2. Foulks GN, Harebell DL, Proia AD, Klintworth GK. Histopathology of silicone oil keratopathy in humans. Cornea. 1991;10(1):29-37.
3. Casswell AG, Gregor ZJ. Silicone oil removal: operative and postoperative complications. Br J Ophthalmol. 1987;71(12):898-902.
4. Kim SW, Oh J, Yang KS, Kim MJ, Rhim JW, Huh K. Risk factors for the development of transient hypotony after silicone oil removal. Retina. 2010;30(8):1228-36.
5. Oh HJ, Chang W, Sagong M. Efficacy and safety of active silicone oil removal through a 23-gauge transconjunctival cannula using an external vacuum pump. Int J Ophthalmol. 2015;8(2):347-52.
6. Gupta S, Chaurasia AK, Chawla R, Kapoor KS, Mahalingam K, Swamy DR, et al. Long-term outcomes of glaucoma drainage devices for glaucoma post-vitreoretinal surgery with silicone oil insertion: a prospective evaluation. Graefes Arch Clin Exp Ophthalmol. 2016; 254(12):2449-54.
7. Patwardhan SD, Azad R, Shah V, Sharma Y. The safety and efficacy of passive removal of silicone oil with 23-gauge transconjunctival sutureless system. Retina. 2010;30(8):1237-41.
8. Cekiç O, Cakir M, Yilmaz OF. Passive silicone oil removal in 23-gauge tranconjunctival vitrectomy. Ophthalmic Surg Lasers Imaging. 2011;42(6):514-5.
9. Kapran Z, Acar N, Unver YB, Altan T, Ocak B. Passive removal of silicone oil with a 25-gauge sutureless system. Jpn J Ophthalmol. 2008;52(1):63-6.
10. Lei JQ, Xie AM, Shi Q. Clinical presentation of a mixed 23-gauge infusion and 20 gauge pars plana technique for active silicone oil removal. Int J Ophthalmol. 2012;5(5):600-4.
11. Mete A, Saygılı O, Kimyon S, Pamukcu C, Çeri S, Güngör K, et al. Comparison of pain experience during 23-G vitreoretinal surgery under topical and retrobulbar anesthesia. Int Ophthalmol. 2017; 37(2):349-56.
12. Mahajan D, Sain S, Azad S, Arora T, Azad R. Comparison of topical anesthesia and peribulbar anesthesia for 23-gauge vitrectomy without sedation. Retina. 2013;33(7):1400-6
13. Bahçecioglu H, Unal M, Artunay O, Rasier R, Sarici A. Posterior vitrectomy under topical anesthesia. Can J Ophthalmol. 2007; 42(2):272-7.
14. Frieman BJ, Friedberg MA. Globe perforation associated with subtenon's anesthesia. Am J Ophthalmol. 2001;131(4):520-1.
15. Kapran Z, Acar N. Active removal of silicone oil with 25-gauge sutureless system. Retina. 2007;27(8):1133-5.
16. Tsui I, Reddy S, Hubschman JP. An elementary and effective method for silicone oil removal. Retina. 2010;30(3):524-6.
17. Abouammoh MA, Yeung J, Gale JS. Sutureless silicone oil removal: a quick and safe technique. Retina. 2012;32(2):396-8.
18. Cacciatori M, Nayak H, Arpa P. Silicone oil removal in pseudophakic and aphakic eyes. Retina. 2007;27(9):1300-1.
19. Dada VK, Talwar D, Sharma N, Dada T, Sudan R, Azad RV. Phacoemulsification combined with silicone oil removal through a posterior capsulorhexis. J Cataract Refract Surg. 2001;27(8):1243-7. Comment in: J Cataract Refract Surg. 2002;28(1):5. J Cataract Refract Surg. 2002;28(10):1719; author reply 1719.
20. El Baha SM, Abouhussein MA, Hemeida TS. Sutureless phacoemulsification with transpupillary removal of silicone oil and intracapsular intraocular lens implantation using illuminated 23-gauge infusion system. Retina. 2011;31(2):408-12.
21. Tan HS, Dell'omo R, Mura M. Silicone oil removal after rhegmatogenous retinal detachment: comparing techniques. Eye (Lond). 2012;26(3):444-7. Comment in: Eye (Lond). 2012;26(9):1276; author reply 1277.
22. Guo CM, Wang YS, Hui YN. Analysis of the complications of two kinds of silicone oil removal. Int J Ophthalmol. 2008;11(1):167-70.
23. Jiang F, Krause M, Ruprecht KW, Hille K. Risk factors for anatomical success and visual outcome in patients undergoing silicone oil removal. Eur J Ophthalmol. 2002;12(4):293-8.
24. Goezinne F, La Heij EC, Berendschot TT, Liem AT, Hendrikse F. Risk factors for redetachment and worse visual outcome after silicone oil removal in eyes with complicated retinal detachment. Eur J Ophthalmol. 2007;17(4):627-37.
25. Woo SJ, Park KH, Hwang JM, Kim JH, Yu YS, Chung H. Risk factors associated with sclerotomy leakage and postoperative hypotony after 23-gauge transconjunctival sutureless vitrectomy. Retina. 2009;29(4):456-63.
26. Parolini B, Prigione G, Romanelli F, Cereda MG, Sartore M, Pertile G. Postoperative complications and intraocular pressure in 943 consecutive cases of 23-gauge transconjunctival pars plana vitrectomy with 1-year follow-up. Retina. 2010;30(1):107-11.
27. Singh CN, Iezzi R, Mahmoud TH. Intraocular pressure instability after 23-gauge vitrectomy. Retina. 2010;30(4):629-34.
28. Jusufbegovic D, Gambrell JD, Barak Y, Schaal S. Twenty-five-gauge vitrectomy for the removal of 5000 centistokes silicone oil. Retina. 2013;33(9):1938-42.
29. Fernandes MB, Souza RV, Vasconcelos GC, Ribeiro KG, Andrade BB, Fernandes CR. Assessing patient satisfaction with cataract surgery under topical anesthesia supplemented by intracameral lidocaine combined with sedation. Arq Bras Oftalmol. 2013;76(6):345-9. Comment in: Arq Bras Oftalmol. 2014;77(2):132.
30. Capuzzo M, Alvisi R. Is it possible to measure and improve patient satisfaction with anesthesia? Anesthesiol Clin. 2008;26(4):613-26.
Submitted for publication:
February 6, 2017.
Accepted for publication:
October 8, 2017.
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.
Approved by the following research ethics committee: Gaziantep University Research Ethics Committee (# 2015/173).