

Eduardo Gayger Müller1; José Álvaro Pereira Gomes1; Walton Nosé1,2; Ricardo Menon Nosé1,2
DOI: 10.5935/0004-2749.20180015
ABSTRACT
We report intraoperative finding of Granular Corneal Dystrophy Type-1 (GCD1) deposits after stromal pneumodissection in deep anterior lamellar keratoplasty (DALK) in a 61-year-old female. Pneumodissection was performed from the center to the periphery of the cornea, characterizing a big bubble type 1 technique which dissects the deep stroma from the predescemetic layer. After stromal removal, persistence of whitish deposits inside the predescemetic layer was noted. During post-operative evaluation, anterior biomicroscopy and anterior segment optical coherence tomography showed granular opacities between the patient's Descemet's membrane and the donor cornea, suggesting possible involvement of the predescemetic layer in GCD1. This may require the surgeon's attention to choose between DALK keratoplasty or penetrating keratoplasty.
Keywords: Corneal dystrophies, hereditary; Corneal transplantation; Cornea; Corneal diseases; Descemet membranes
RESUMO
Relatamos o achado intraoperatório de persistência dos depósitos de Distrofia Granular Tipo 1 (GCD1) após pneumodissecção estromal no transplante de córnea lamelar anterior profundo (DALK) em uma mulher de 61 anos. A pneumodissecção começou a partir do centro para a periferia da córnea, caracterizando uma big bubble tipo 1, que disseca o estroma profundo da camada pré-Descemet. Após a remoção do estroma, notamos a persistência de depósitos esbranquiçados no interior da camada pré-Descemet. Na avaliação pós-operatória, a biomicroscopia anterior e a tomografia de coerência óptica do segmento anterior evidenciaram opacidades granulares entre a membrana de Descemet e a córnea doadora, sugerindo o possível envolvimento da camada pré-Descemet na GCD1, o que pode chamar atenção do cirurgião para decidir entre manter o DALK ou converter para transplante penetrante.
Descritores: Distrofias hereditárias da córnea; Transplante de cornea; Córnea; Doenças da córnea; Lâmina limitante posterior
INTRODUCTION
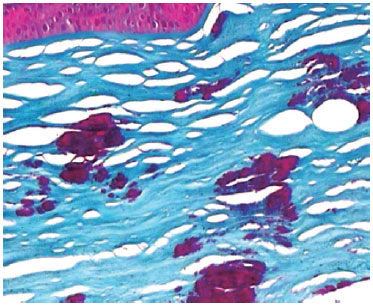
Granular Corneal Dystrophy Type-1 (GCD1) belongs to the International Committee for Classification of Corneal Dystrophies category 1 (IC3D Category 1), and is a stromal, autosomal dominant, transforming growth factor b-induced protein (TGFbIp)-associated corneal dystrophy. Although it is classified as a stromal dystrophy, studies suggest the possibility that its granular opacities originate from the corneal epithelium and migrate to the corneal stroma. With progression, the opacities become more confluent in the superficial cornea and reduce visual acuity. In later life, granules extend into the deeper stroma approaching Descemet's membrane (DM). Light microscopy has demonstrated Masson trichrome-stained keratohyalin deposits at various stromal layers and may show partial destruction of the Bowman layer(1).
When vision is significantly affected or recurrent corneal erosion occurs, management options include photokeratectomy or surgical treatments such as deep anterior lamellar keratoplasty (DALK) and penetrating keratoplasty (PK)(1).
CASE REPORT
We present the case of a 61-year-old female patient with a complaint of low visual acuity in her left eye for a long time. She had a past medical history of PK in her right eye due to corneal dystrophy five years ago. Family history demonstrated the existence of relatives presenting the same ophthalmologic pathology (Figure 1; one daughter and two grandchildren).
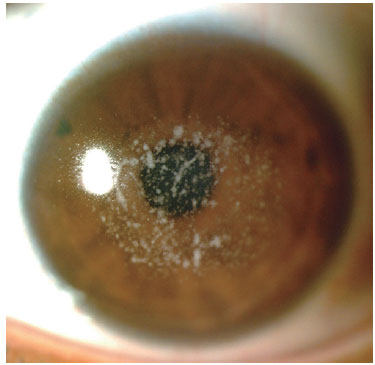
Her best corrected visual acuity (BCVA) was 20/100 in OD and 20/400 in OS. Anterior biomicroscopy showed a clear corneal graft in OD and whitish granules in the center cornea with clear intervening stroma through the whole stromal thickness in OS.
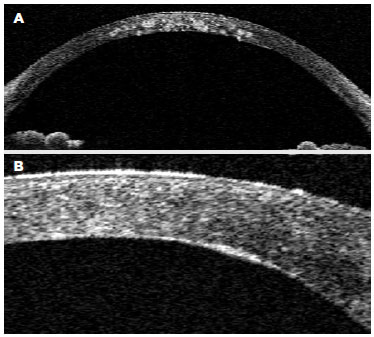
We performed Visante optical coherence tomography (OCT)® (Carl Zeiss Meditec, Dublin, CA, USA) which showed hyperreflective granules from the Bowman's layer to the deep stromal lamellae, indenting the DM in some areas (Figure 2 A).
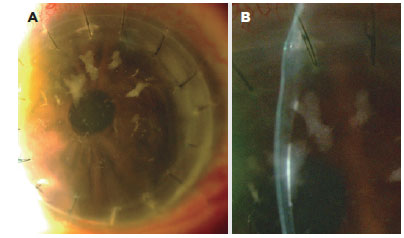
Due to the depth of granular opacities and strong suspicion of GCD1, Big-bubble DALK was performed. Surgery was performed starting with partial thickness trephination using a Barron vacuum trephine. Next, deep stromal lamellae were punctured using a 26-gauge needle and a Sarnicola model cannula was inserted through the dissected lamellae. Air was forced into the stroma and pneumodissection involved a Type-1 big-bubble technique, which separated the deep stroma from the predescemetic layer. Stromal dissection was performed and the predescemetic layer remained intact, with evident residual whitish granules in the superior portion of the predescemetic layer. The opacities were left untouched due to the risk of rupture through manipulation as well as their apparent position outside the visual axis. The previously trephined donor graft (with DM) was attached using separate mononylon 10-0 sutures.
The dissected stroma was sent for anatomopathological analysis with Masson trichrome staining and showed stained hyaline deposits at various stromal layers, confirming diagnosis of GCD1 (Figure 3).
Post-operative anterior biomicroscopy with scleral scattering illumination showed persistence of whitish granules in the recipient's cornea (Figure 4 A), which were identified as being anterior to the DM and posterior to the donor cornea using a slit lamp (Figure 4 B). Visante® OCT was performed one month post operatively and showed hyperreflective opacities between the donor cornea and the recipient's DM, demonstrating persistence of dystrophy deposits inside the predescemetic layer (Figure 2 B). Her BCVA improved to 20/60 in the first month even with opacities near the visual axis.
DISCUSSION
Treatment of deep stromal opacities such as corneal dystrophies that do not affect the DM can be safely performed using the DALK technique(2). Considering this, and after performing anterior segment OCT, we chose to perform DALK in our case aiming to remove the entire stromal thickness along with the hyaline deposits. However, stromal opacities persisted after pneumodissection with the big bubble technique, suggesting possible involvement of the predescemetic layer in GCD1.
DALK has been considered a safe alternative to PK in the treatment of corneal stromal diseases that do not affect the endothelium and DM(3). With advances in dissection techniques (i.e., Anwar's big-bubble(4), it has become even more reproducible and can now deliver visual acuity results as good as PK. Recognition of the novel predescemetic layer (PDL) by Dua et al.,(5) has led to further surgical improvements such as the utility of this layer in DALK(6), and new techniques like predescemetic endothelial keratoplasty (PDEK)(7).
Bubble types in pneumodissection are described by Dua et al.(5), and are classified as Type-1 (a bubble between the PDL and the deep stromal lamellae) and Type-2 (a bubble between the DM and the PDL). It is now known that when a Type-1 big bubble is achieved, resistance of the residual lamellae is higher allowing even triple procedures without rupture(8).
Recurrences of GCD1 in the host cornea have been described after anterior lamellar keratoplasty. Pantanelli et al.(9) reported the case of a 28-year-old male with GCD1 who underwent non-Descemet baring DALK and presented dystrophy recurrence confined to the residual host stroma just anterior do the DM, which was confirmed by OCT. Rama et al.(10), described recurrence of typical deposits of GCD1 deep in the graft interface area. This localization is atypical, since in most cases recurrences in grafts tend to be initially superficial and situated in the epithelial or sub-epithelial corneal layers(10).
In the present study, there was no dystrophy recurrence. Instead, we found persistence of GCD1 deposits in the predescemetic layer after Type-1 Big Bubble DALK. GCD1 diagnosis was confirmed with unequivocal pathological analysis with Masson trichrome staining and topography of persistent deposits was indicated by the surgical technique (which kept the predescemetic layer intact using a Big-Bubble Type-1 technique) as well as by Visante OCT® imaging showing the persistence of deposits just anterior to the DM.
Intraoperatively, we chose to avoid further manipulation in order to keep the PDL intact. Maintaining the patient's DM can be more beneficial to the patient in terms of less post-operative complications and graft rejection chances in comparison to the possibility of switching to PK. In addition, residual opacities did not compromise the visual outcome considering that denser stromal deposits were outside the visual axis. However, corneal surgeons should note that in case of denser opacities remaining inside the visual axis, switching to PK would be a better option to improve the visual outcome.
REFERENCES
1. Roncone DP. Granular corneal dystrophy: a novel approach to classification and treatment. Optom Vis Sci. 2014;91(3):e63-71.
2. Unal M, Arslan OS, Atalay E, Mangan MS, Bilgin AB. Deep anterior lamellar keratoplasty for the treatment of stromal corneal dystrophies. Cornea. 2013;32(3):301-5. Comment in: Cornea. 2013;32(8):e185. Cornea. 2013;32(8):e184-5.
3. Chen G, Tzekov R, Li W, Jiang F, Mao S, Tong Y. Deep anterior lamellar keratoplasty versus penetrating keratoplasty: a meta-analysis of randomized controlled trials. Cornea. 2016;35(2):169-74.
4. Anwar M, Teichmann KD. Big-bubble technique to bare Descemet's membrane in anterior lamellar keratoplasty. J Cataract Refract Surg. 2002;28(3):398-403.
5. Dua HS, Faraj LA, Said DG, Gray T, Lowe J. Human corneal anatomy redefined: a novel pre-Descemet's layer (Dua's layer). Ophthalmology. 2013;120(9):1778-85. Comment in: Ophthalmology. 2014;121(5):e24-5; Ophthalmology. 2013;120(9):1715-7; Ophthalmology. 2014;121(5):e25-6; Arch Soc Esp Oftalmol. 2015; 90(7):301-2.
6. Dua HS, Mastropasqua L, Faraj L, Nubile M, Elalfy MS, Lanzini M, et al. Big bubble deep anterior lamellar keratoplasty: the collagen layer in the wall of the big bubble is unique. Acta Ophthalmol. 2015; 93(5):427-30.
7. Agarwal A, Dua HS, Narang P, Kumar DA, Agarwal A, Jacob S, et al. Pre-Descemet's endothelial keratoplasty (PDEK). Br J Ophthalmol. 2014;98(9):1181-5.
8. Zaki AA, Elalfy MS, Said DG, Dua HS. Deep anterior lamellar keratoplasty--triple procedure: a useful clinical application of the pre-Descemet's layer (Dua's layer). Eye (Lond). 2015;29(3):323-6.
9. Pantanelli SM, Herzlich A, Yeaney G, Ching ST. Recurrence of granular corneal dystrophy type I deposits within host stroma after non-descemet baring anterior lamellar keratoplasty. Cornea. 2014; 33(12):1348-51. Comment in: Cornea. 2015;34(6):e17-8. Comment in: Cornea. 2015;34(5)e15. Comment on: Cornea. 2014;33(12): 1348-51.
10. Rama P, Knutsson KA, Rojo C, Carrera P, Ferrari M. Unusual early recurrence of granular dystrophy after deep anterior lamellar keratoplasty: case report. Arq Bras Oftalmol. 2013;76(2):126-8.
Submitted for publication:
February 9, 2017.
Accepted for publication:
September 3, 2017.
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.