

Gabriel Costa de Andrade1; João Rafael de Oliveira Dias1; André Maia1; Liliane de Almeida Kanecadan1; Nilva Simeren Bueno Moraes1; Rubens Belfort Junior1; Jade Marie Edenvirg Lasiste2; Miguel N Burnier2
DOI: 10.5935/0004-2749.20180014
ABSTRACT
This study reports the first case of intravitreal angiostrongyliasis in South America treated with posterior worm removal via pars plana vitrectomy. This was a retrospective, observational case study. Data from medical charts, wide-field digital imaging, ocular ultrasound, and visual evoked potential studies were reviewed. A 20-month-old boy presented with eosinophilic meningitis and right eye exotropia. Polymerase chain reaction analysis of the cerebrospinal fluid showed a positive result for Angiostrongylus cantonensis. Fundus examination revealed a pale optic disc, subretinal tracks, vitreous opacities, peripheral tractional retinal detachment, and a dead worm in the vitreous cavity. The patient underwent pars plana vitrectomy with worm removal. This case report illustrates the first case of intravitreal angiostrongyliasis in South America, possibly related to the uncontrolled spread of an exotic invasive species of snail.
Keywords: Angiostrongylus cantonensis; Eye diseases/parasitology; Vitrectomy; Case report; South America
RESUMO
O objetivo deste estudo foi relatar o primeiro caso na América do Sul de angiostrongilíase intravítrea tratada com vitrectomia posterior via pars plana e remoção do verme. Este foi um relato de caso observacional. O prontuário médico, sistema de imagem digital de campo amplo, ultrassonografia ocular, e potenciais evocados visuais foram revistos. Um menino de 1 ano e 8 meses de idade manifestou meningite eosinofílica e exotropia olho direito. A análise de PCR do liquor foi positiva para Angiostrongylus cantonensis. O exame de fundo de olho revelou disco óptico pálido, faixas sub-retinianas, opacidades vítreas, descolamento de retina tracional periférico e um verme morto no vítreo. O paciente foi submetido a vitrectomia posterior via pars plana com a remoção do verme. Concluindo, este é o primeiro relato de caso de angiostrongilíase intravítrea na América do Sul, possivelmente relacionado com a disseminação de uma espécie de lesma exótica neste continente.
Descritores: Angiostrongylus cantonensis; Oftalmopatias/parasitologia; Vitrectomia; Relatos de casos; América do Sul
INTRODUCTION
Parasitic infection is common in many developing areas of the world and is related to the lack of health care and piped water and the habit of eating raw foods(1). Eosinophilic meningitis, common in some Asian countries, is most commonly caused by the nematode Angiostrongylus cantonensis. Most patients present with fever and severe headache without neurological signs. While the rat is the definitive host, humans are infected by eating inadequately cooked intermediate hosts (slugs, snails, or crabs) or vegetables contaminated by immature larvae(2). Incubation times can range from two weeks to two months; ova or parasites are rarely seen in stool exams, compounding the difficulty in diagnosis(3).
Only 1.2% of angiostronglyiasis cases have ocular involvement, and only 1.1% of these cases show Angiostrongylus cantonensis larvae in the eye(4,5). Ocular manifestations in this disease are rare but are associated with significant morbidity. The disease is associated with eating habits and also occurs in some developing areas of the world. Intraocular angiostrongyliasis has previously been described in patients from Thailand, Vietnam, Japan, Taiwan, Papua New Guinea, India, and Sri Lanka(1,2,4,6-10). The first case of snails infected with Angiostrongylus cantonensisin South America was reported in 2007, and the first human case in South America was described in 2009 in Ecuador(11). Here, we report a case of ocular angiostrongyliasis with an intravitreal worm, treated using posterior pars plana vitrectomy (PPV), which resulted in successful worm removal.
CASE REPORT
A 20-month-old boy presented with fever (39.5ºC), lethargy, loss of appetite, and vomiting. The patient was born and raised in São Paulo, and the family had not traveled abroad. His leukocyte count was 13.5 × 103/mm3 with 36% eosinophils. Hemoglobin, hematocrit, and serum electrolyte levels were within normal ranges. After systemic evaluation, a lumbar puncture was performed for Angiostrongylus cantonensis testing (using polymerase chain reaction (PCR) carried out at Adolfo Lutz Institute, São Paulo, Brazil), which was positive. He was treated with 15 mL/day albendazole and prednisolone for 15 days and progressed to recovery of CNS-related symptoms. Ophthalmological evaluation of the left eye was normal and that of the right eye revealed exodeviation, anterior chamber reaction, and posterior synechia. Fundus examination revealed a pale optic disc associated with vitreous opacities, generalized retinal pigment epithelial pigmentary alterations, subretinal tracks, peripheral retinal detachment, and the presence of a presumed dead larva in the vitreous cavity. Visually evoked potential (VEP) showed 20/600 visual acuity in the right eye and 20/40 in the left eye.
Ultrasound scanning (UltraScan, Alcon, 10 MHz transducer) was performed and showed partial posterior vitreous detachment, tractional retinal detachment in the nasal wall, and splitting of the posterior cortical vitreous (vitreoschisis). Elevation of the optic disc was present, suggesting an inflammatory process. An area of high reflectivity and thick interface, which mobilized along with the vitreous, was observed in the vitreous body, consistent with the larvae observed in the funduscopic exam (Figure 1 E and F).
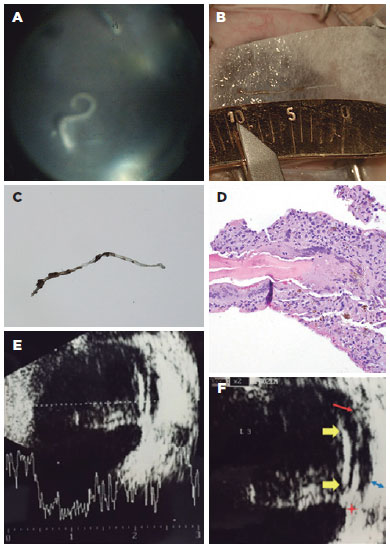
The patient underwent 23-gauge PPV. During surgery, the larva was seen as a thin, whitish, semitransparent, and cylindrical structure without motile response to the endoilluminator probe (Figure 1 A). The larva was removed and sent for parasitological evaluation (Figure 1 B).
A follow-up VEP performed two months after surgery showed maintenance of 20/600 visual acuity in the right eye. Post-operatory ophthalmological examination revealed no active anterior or posterior uveitis. No complication related to the surgical procedure, such as uveitis, cataract, glaucoma, or retinal detachment, was present.
Histopathology
On gross examination, the larva extracted from the vitreous measured 10 mm in length and 0.15 mm in width (Figure 1 C). The larva was surrounded by strongly attached pigmented tissue. Its buccal and anal cavities were difficult to distinguish. On hematoxylin-eosin staining (Figure 1, 0.50x magnification), the larva showed loss of basophilic reactivity and homogenization of internal structures. Moreover, a scant, patchy, and shiny eosinophilic amorphous material was noticed, consistent with Hoeppli-Splendore phenomena. In addition, a foreign body-type granulomatous reaction with multinucleated giant cells and few retinal pigmented epithelium cells was seen surrounding the larva (Figure 1 D). All these features were consistent with a dead nematode of the Angiostrongylus sp.-type.
DISCUSSION
Ocular angiostrongyliasis most commonly presents with blurred vision(8). Ocular manifestations include optic neuritis, uveitis, retinal changes, keratic precipitates on the cornea, blepharospasm, macular or retinal edema, papilledema, binocular diplopia and abducens nerve palsy, optic nerve compression, necrotic retinitis with exudative retinal detachment, and peri-orbital inflammation(1-5). The diagnosis of ocular angiostrongyliasis depends on elucidating travel history and/or possible intake of food suspected of infective larvae, as well as on a thorough clinical examination.
Invasion of the eye by A. cantonensis is thought to result from two mechanisms: (1) migration of the larva along the surface and base of the brain and traveling between the nerve and sheath upon reaching the optic nerve; and (2) direct invasion from the bloodstream(5). The optic nerve, with its long intracranial portion, is particularly susceptible to invasion(6).
Management of ocular angiostrongyliasis generally involves use of steroids administered orally, topically, or-with the involvement of more systemic infections-intravenously. Anti-helminthic medications, such as albendazole, are usually recommended, and the patient should be closely monitored for signs of worsening inflammation in the eye. Surgical removal of any larvae noticed is imperative. If the larva is considered to be alive, laser immobilization can be performed prior to surgery, and the worm should be directed away from the posterior pole(5,6). In this case, as the larva was observed to be immotile on probing, no pre-operative laser was necessary.
Awareness of the evolving epidemiology of ocular angiostrongyliasis is important for clinicians. The first case of human ocular angiostrongyliasis was reported in 1962(7), and, to date, 35 more cases from 10 countries (Asia and Africa) have been reported. Traditionally, this disease was considered to be endemic to the Southeast Asia and Pacific regions(4). The first case in the Americas was reported in 2009 in Jamaica in a 30-year-old woman presenting with a live worm in the anterior chamber(10).
In conclusion, this is a case report of rare intraocular manifestation caused by A. cantonensis that raises the possibility that the disease may become an emerging infection in Brazil, notably in areas where the local population lives in areas without basic sanitation and under low socio-economic conditions. Furthermore, increasing prevalence of the intermediate host, the giant African snail, across Brazil is worthy of note.
REFERENCES
1. Chiu JK, Huang WH, Cheng KH, Chang IH, Teng WH, Kao TH. Three cases of worm proven human angiostrongyliasis in Taiwan. Zhonghua Min Guo Wei Sheng Wu Ji Mian Yi Xue Za Zhi. 1981; 14(4):247-50.
2. Scrimgeour EM, Chambers BR, Kaven J. A probable case of ocular angiostrongyliasis in New Britain, Papua New Guinea. Trans R Soc Trop Med Hyg. 1982;76(4):538-40.
3. Singalavanija A, Wangspa S, Teschareon S. Intravitreal angiostrongyliasis. Aust N Z J Ophthalmol. 1986;14(4):381-4.
4. Durette-Desset MC, Chabaud AG, Cassim MH, Ismail MM, Premaratne UN, Abeyewickreme W, et al. On an infection of a human eye with Parastrongylus (= Angiostrongylus) sp. in Sri Lanka. J Helminthol. 1993;67(1):69-72.
5. Toma H, Matsumura S, Oshiro C, Hidaka T, Sato Y. Ocular angiostrongyliasis without meningitis symptoms in Okinawa, Japan. J Parasitol. 2002;88(1):211-3.
6. Thu TP, Nguyen NX, Lan le T, Kuchle M. [Ocular angiostrongylus cantonensis in a female Vietnamese patient: case report]. Klin Monatsbl Augenheilkd. 2002;219(12):892-5. German.
7. Patikulsila D, Ittipunkul N, Theerakittikul B. Intravitreal angiostrongyliasis: report of 2 cases. J Med Assoc Thai. 2003;86(10):981-5.
8. Sawanyawisuth K, Kitthaweesin K, Limpawattana P, Intapan PM, Tiamkao S, Jitpimolmard S, et al. Intraocular angiostrongyliasis: clinical findings, treatments and outcomes. Trans R Soc Trop Med Hyg. 2007;101(5):497-501.
9. Prommindaroj K, Leelawongs N, Pradatsundarasar A. Human angiostrongyliasis of the eye in Bangkok. Am J Trop Med Hyg. 1962; 1:759-61.
10. Mattis A, Mowatt L, Lue A, Lindo J, Vaughan H. Ocular angiostrongyliasis-first case report from jamaica. West Indian Med J. 2009; 58(4):383-5.
11. Pincay T, Garcia L, Decker O, Martini L, Moreira JM. Angiostrongiliasis por Parastrongylus (Angiostrongylus) cantonensis em Ecuador. Bol Epidem Ecuador. 2009;6:25-32.
Submitted for publication:
June 12, 2017.
Accepted for publication:
October 8, 2017.
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.