

Vesna Jovanovic1,2; Mirko Jankov2; Ljubisa Nikolic2
DOI: 10.5935/0004-2749.20180013
ABSTRACT
We report a case of central corneal perforation treated with an autologous lamellar scleral graft and histologic findings obtained after a subsequent penetrating keratoplasty. A corneal perforation within a large Pseudomonas ulcer in a 55-year-old male rigid gas permeable contact lens wearer was sealed by a lamellar scleral graft from the same eye, followed by an uneventful penetrating keratoplasty 6 months later. Histology of the excised button revealed that the well-apposed graft, which maintained the irregular arrangement of the scleral collagen fibers, was embedded in the corneal stroma over the deep blood vessels and a rupture in Descemet's membrane. The clinical and histologic findings showed that autologous lamellar scleral grafts can be successfully used for the emergency treatment of corneal perforation when a corneal transplant is not available. The distinctive scleral structure revealed by histology and the inadequate graft transparency indicate that visual rehabilitation of eyes with a central corneal perforation can be achieved only by a subsequent optic penetrating keratoplasty.
Keywords: Corneal injuries; Corneal transplantation; Sclera/transplantation; Transplantation, autologous; Keratoplasty, penetrating
RESUMO
Relatamos um caso de perfuração corneana central tratada com enxerto autólogo lamelar de esclera e os achados histológicos obtidos após ceratoplastia penetrante (CP) subsequente. Uma perfuração da córnea devido a uma grande úlcera por Pseudomonas em um usuário de lentes de contato rígidas gás permeável de 55 anos de idade foi selada por um enxerto escleral lamelar do mesmo olho, seguida de ceratoplastia penetrante, sem intercorrências, seis meses depois. A histologia do botão excisado revelou que um enxerto bem posicionado, que manteve o arranjo irregular das fibras de colágeno escleral, foi incorporado no estroma corneano sobre os vasos sanguíneos profundos e uma ruptura na membrana de Descemet. Os achados clínicos e histológicos demonstraram que o enxerto autônomo de esclerose lamelar pode ser usado com sucesso como tratamento de emergência da perfuração da córnea, quando o transplante de córnea não é possível. A estrutura escleral característica revelada pela histologia e a transparência inadequada do enxerto indicam que a reabilitação visual dos olhos com uma perfuração corneana central só pode ser alcançada através de uma ceratoplastia penetrante óptica subsequente.
Descritores: Lesões da córnea; Transplante de córnea; Esclera/transplante; Transplante autólogo; Ceratoplastia penetrante
INTRODUCTION
Corneal perforations are serious ophthalmic emergencies, which if not promptly treated, lead to permanent visual and eyeball loss. Depending on the causative factor, the size of the perforation, and the visual potential, suggested procedures for saving the globe are: cyanoacrylate glue, amniotic membrane transplantation, conjunctivoplasty, therapeutic keratoplasty(1), and the almost forgotten technique of autologous lamellar scleral grafting(2).
Introduced into clinical practice by Larsson in 1946(2), the technique did not gain much attention. Since then, only three papers describing similar techniques in clinical settings have been published, two of them recently(3-5). The use of autologous scleral lamellar tissue is an excellent way to close perforated corneas in emergency cases, especially if donor corneas are unavailable. Autologous scleral tissue is readily available, provides sufficient strength, and eliminates the possibility of an immune reaction. In terms of globe stability and visual acuity restoration, peripheral corneal perforations treated in this way have good long-term results because the corneal transparency away from the visual axis is of minimal importance(2,4). On the other hand, although central corneal perforation closure with scleral lamellae can save the globe, it may not produce a favorable final visual outcome. Earlier reports presented histologic findings of scleral tissue embedded into the cornea in an experimental model(6,7).
Here, we present a case of corneal perforation treated with an autologous lamellar scleral graft and the histologic findings after penetrating keratoplasty (PK). To the best of our knowledge, this is the first report on the histology of such a graft in human eyes.
CASE REPORT
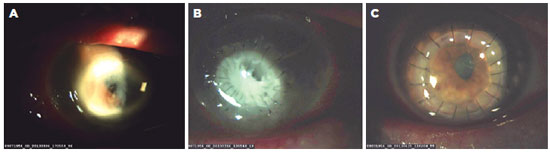
A 55-year-old male presented with irritation, redness, and diminished visual acuity for a couple of days in his right eye. The patient had keratoconus and wore rigid gas permeable contact lenses in both eyes. On presentation, his best distance corrected visual acuity (BDCVA) was hand motion. Slit-lamp examination revealed a central corneal perforation of 2 × 2 mm, within a large central 6 × 6 mm ulcer (Figure 1 A). The globe was soft, and the Seidel test was positive. Corneal scraping was performed, and the initial treatment was commenced with hourly topical tobramycin. The culture was positive for Pseudomonasspp. Therapeutic PK was not possible because of the lack of donor corneas; therefore, the patient underwent autologous lamellar scleral grafting 3 days after the initial presentation. A superior 180º peritomy with a fornix-based flap was performed until the bare sclera was reached. A partial-thickness scleral patch measuring 6 × 6 mm was harvested by manual dissection from the superotemporal quadrant of the same eye. The graft was sutured with multiple interrupted nylon 10-0 sutures with many knots left unburied because of the fragility of the surrounding corneal tissue (Figure 1 B). The postoperative treatment included topical tobramycin 0.3% (Tobrex; Alcon, Fort Worth, TX, USA) hourly. On the following day, the Seidel test was negative, and the intraocular pressure, which was checked digitally, was normal. The eye gradually became quiet, and the loose sutures were selectively removed over the following 3 months. The examination at 6 months showed a BDCVA of 1/60 as a result of the still opaque scleral graft. The patient then underwent an optical PK (Figure 1 C), and the excised button was examined histologically. Postoperatively, the graft was transparent, and the BDCVA was reduced to 6/30 because of the partial prepupillary membrane, and cortical cataract. Eight months after PK, the patient underwent phacoemulsification, membrane excision, and posterior chamber intraocular lens implantation, after which his BDCVA was 6/6.
Histology
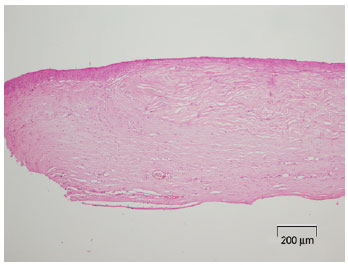
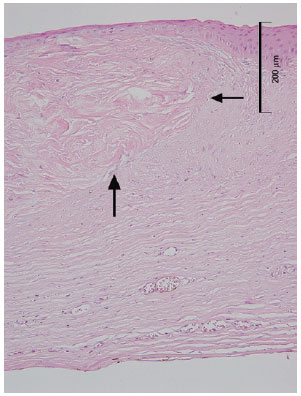
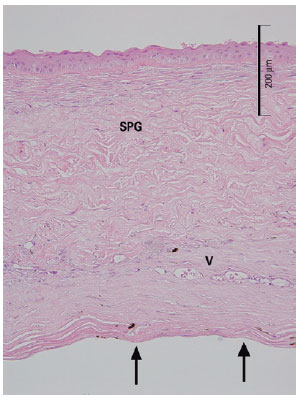
The excised 7.0-mm corneal button was examined histologically (hematoxylin-eosin staining) (Figure 2). The corneal epithelium was continuous, completely covering both the cornea and the scleral graft. The embedded scleral graft was well adapted. Irregular arrangement of the scleral collagen fibers was completely distinct from the characteristically regular corneal stromal collagen architecture (Figure 3). Numerous blood vessels were present, reaching both the peripheral and central parts of the deeper layers of corneal tissue. The break in Descemet's membrane was clearly visible (Figure 4).
DISCUSSION
In 1946, Larsson introduced a new technique to treat perforated corneas using an autologous scleral transplant(2). After several failed conjunctivoplasties, Larsson successfully treated a peripheral corneal perforation caused by exposure keratitis in a 7-year-old girl using a 2.5-mm autologous scleral graft. Few similar reports have been published since. In 1983, Stilma reported the use of autologous scleral grafts in six eyes for the treatment of peripheral corneal perforations originating from Mooren's ulcers in an African population(3). Further, Prydal reported a case of a professional driver with a traumatic peripheral corneal perforation closed with an autologous scleral patch that resulted in rapid visual rehabilitation with a good outcome (BDCVA 20/30)(4). The same technique used by Prasher was effective in closing a peripheral perforation within a previously healed corneal ulcer(5). The method proved to be safe with no complications reported and no further surgeries needed for peripherally placed perforations.
A patch can be created from the superior or inferior parts of the sclera using either a trephine(3-5) or customized free-hand dissection and excision(2), depending on the size and shape of the wound. In order to save globes when donor corneas are lacking in our country, we used the same technique, although the perforation was large and placed centrally. The globe was saved, and the eye became quiet. Nonetheless, the final visual outcome was not satisfactory despite a certain degree of scleral translucency, which developed over time and required a subsequent optical PK.
As early as the mid-20th century, it was observed that the sclera loses its dense opaque white color if it is embedded into the corneal tissue. Both Winkelman(6) and Maurice and Singh(7) used experimental models to investigate this phenomenon, and suggested that a gradual replacement of the scleral collagen with corneal collagen eventually leads scleral grafts to express corneal properties.
The course of our clinical case and the histologic examination of the excised human cornea with an embedded scleral graft indicate that a 6-month period is not long enough to observe substantial changes in either the scleral properties of the patch graft or visual acuity.
In conclusion, autologous lamellar scleral grafts can be successfully used for the treatment of corneal perforation when a corneal transplant is not available. However, it is prudent to plan a PK at a later date as the ultimate solution for visual disability when the perforation is located centrally.
REFERENCES:
1. Portnoy SL, Insler MS, Kaufman HE. Surgical management of corneal ulceration and perforation. Surv Ophthalmol. 1989;34(1):47-58.
2. Larsson S. Treatment of perforated corneal ulcer by autoplastic scleral transplantation. Br J Ophthalmol. 1948;32(1):54-7.
3. Stilma JS. Conjunctival excision or lamellar scleral autograft in 38 Mooren`s ulcers from Sierra Leone. Br J Ophthalmol. 1983;67(7): 475-8.
4. Prydal JI. Use of an autologous lamellar scleral graft to repair a corneal perforation. Br J Ophthalmol. 2006;90(7):924.
5. Prasher P. Use of an autologous lamellar scleral graft to repair corneal perforation. Int Ophthalmol. 2014;34(4):957-60.
6. Winkelman JE. Optical behaviour of sclera transplanted into the cornea. Am J Ophthalmol. 1951;34(10):1379-97 .
7. Maurice DM, Singh T. The fate of scleral grafts in the cornea. Cornea. 1996;15(2):204-9.
Submitted for publication:
July 7, 2017.
Accepted for publication:
August 24, 2017.
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.