

Kadriye Erkan Turan1; Hande Taylan Sekeroglu1; Ata Baytaroglu1; Figen Bezci1; Sevilay Karahan2
DOI: 10.5935/0004-2749.20180003
ABSTRACT
Purpose: To (a) determine the normative values for optical coherence tomography (OCT) parameters such as central macular thickness, retinal nerve fiber layer thickness, and choroidal thickness in healthy children; (b) investigate the relationships of these parameters with axial length, central corneal thickness, refractive errors, and intraocular pressure; and (c) determine interexaminer agreement for choroidal thickness measurements.
Methods: In this cross-sectional study, 120 healthy children aged 8-15 years underwent detailed ophthalmological examination and OCT measurements. Choroidal thickness was measured at three separate locations by two independent examiners.
Results: The mean global retinal nerve fiber layer thickness was 98.75 ± 9.45 µm (79.0-121.0). The mean central macular thickness was 232.29 ± 29.37 µm (190.0-376.0). The mean subfoveal choroidal thickness obtained by examiner 1 was 344.38 ± 68.83 µm and that obtained by examiner 2 was 344.04 ± 68.92 µm. Interexaminer agreement was between 99.6%-99.8% for choroidal thickness at three separate locations. Central macular thickness increased with axial length (r=0.245, p=0.007). Choroidal thickness increased with age (r=0.291, p=0.001) and decreased with axial length (r=-0.191, p=0.037). Global retinal nerve fiber layer thickness decreased with axial length (r=-0.247, p=0.007) and increased with central corneal thickness (r=0.208, p=0.022). Global retinal nerve fiber layer thickness positively correlated with choroidal thickness (r=0.354, p<0.001). Global retinal nerve fiber layer thickness (r=0.223, p=0.014) and choroidal thickness (r=0.272, p=0.003) increased with the spherical equivalent (D).
Conclusions: Optical coherence tomography parameters showed a wide range of variability in children. Retinal nerve fiber layer thickness, central macular thickness, and choroidal thickness were found to be either inter-related or correlated with age, central corneal thickness, axial length, and refractive errors. Furthermore, manual measurements of choroidal thickness showed high interexaminer agreement. Because normative values for optical coherence tomography parameters differed in children, the measurements should be interpreted according to an age-appropriate database.
Keywords: Optic nerve; Retina; Choroid; Macula lutea; Refractive errors; Tomography, optical coherence/methods; Reference values; Children
RESUMO
Objetivo: Determinar valores normativos para parâmetros de tomografia de coerência óptica consistindo em espessura macular central, espessura da camada de fibra nervosa da retina e espessura coroidal em crianças saudáveis, para investigar suas relações com o comprimento axial, espessura corneana central, erros refractivos e pressão intraocular e determinar a concordância interexaminador para medidas de espessura coroidal.
Métodos: um total de 120 crianças saudáveis com idade entre 8 e 15 anos foram submetidas a exame oftalmológico detalhado e a medições de tomografia de coerência óptica em uma configuração de estudo transversal. A espessura coroide foi medida por dois examinadores independentes em 3 pontos distintos.
Resultados: A espessura global media da camada de fibra nervosa da retina foi de 98.75 ± 9.45 µm (79.0-121.0). A espessura macular central media foi de 232.29 ± 29.37 µm (190.0-376.0). A espessura coroidea subfoveal media foi de 344.38 ± 68.83 µm medida pelo examinador 1 e 344.04 ± 68.92 µm medida pelo examinador 2. A concordância foi entre 99.6-99.8% para a espessura coroidal em 3 pontos distintos. Verificou-se que a espessura macular central aumentava com o comprimento axial (r=0.245, p=0.007). A espessura da coroide aumentou com a idade (r=0.291, p=0.001) e diminuiu com o comprimento axial (r=-0.191, p=0.037). A espessura global da camada de fibras nervosas da retina diminuiu com o comprimento axial (r=-0.247, p=0.007) e aumenta com a espessura central da córnea (r=0.208, p=0.022). A espessura global da camada de fibras nervosas da retina foi correlacionada positivamente com a espessura coroidal (r=0.354, p<0.001). A espessura global da camada de fibras nervosas da retina (r=0.223, p=0.014) e a espessura coroide (r=0.272, p=0.003) aumentaram com o equivalente esférico (D).
Conclusões: os parâmetros de tomografia de coerência óptica parecem mostrar uma ampla gama de variabilidade em crianças. A espessura da camada de fibra nervosa da retina, a espessura macular central, a espessura coroidea estão inter-relacionadas ou correlacionadas com a idade, espessura corneana central, comprimento axial e erros refractivos. Além disso, as medidas manuais da espessura coroidea apresentaram alta concordância entre examinadores. Deve-se ter em mente que os valores normativos dos parâmetros da tomografia de coerência óptica diferem em crianças, portanto, as medidas devem ser interpretadas de acordo com uma determinada base de dados apropriada para idade.
Descritores: Nervo óptico; Coroide; Macula lutea; Erros de refração; Tomografia de coerência óptica/métodos; Valores de referência; Criança
INTRODUCTION
Optical coherence tomography (OCT) is a noninvasive tool that provides high-quality in vivo images of the retina, macula, optic disc, and choroid due to differences in the reflective properties of the ocular media, enabling quantitative assessment(1). OCT is a very important diagnostic procedure in the detection and follow-up of many macular diseases, glaucoma, and other optic nerve diseases(2).
The normative database in OCT device software is targeted at adults aged >18 years and its utility in children is limited. Unlike the eyes of adults, eyes of healthy children are still developing. Several studies have investigated whether there OCT parameters change with age. Alamouti and Funk(3) reported that both the total retinal thickness and the retinal nerve fiber layer thickness (RNFLT) significantly decrease with age. Axonal loss with age was thought to be responsible for RNFLT decrease in adults, especially after age 50 years (3). Schuman et al.(4) also reported a decrease in RNFLT with age. Shao et al.(5) reported a decrease in the choroidal thickness (CT) of the posterior pole with age. However, other reports have shown no association of OCT parameters with age(1,6,7).
Since OCT normative data are mainly based on age, it is not appropriate to compare the findings obtained for children with the values in the standard database(2). The objective of the present study was to determine the normative values for central macular thickness (CMT), RNFLT, and CT measured using OCT in healthy children and to investigate their relationships with axial length (AL), central corneal thickness (CCT), refractive errors, and intraocular pressure (IOP). The second objective was to determine the interexaminer agreement for CT measurements.
METHODS
The study included 120 healthy children aged 8-15 years, who visited the ophthalmology clinic for a routine examination. One eye from each subject was randomly selected for analysis. The study protocol was approved by the ethics committee and the study was conducted in accordance with the tenets of the Declaration of Helsinki.
Inclusion criteria included children born at term (≥37 weeks gestational age) with normal birth weight (≥2500 g), 1.0 best-corrected visual acuity or better (on the Snellen scale), refractive error (in spherical equivalent) within ± 2.50 diopters, intraocular pressure £21 mmHg, and without any retinal or optic disc anomalies determined by mydriatic fundus examination. Patients with systemic diseases were also excluded.
Detailed demographic data were obtained from the parents. All children underwent detailed ophthalmological evaluation including cycloplegic refraction, best-corrected visual acuity (BCVA), slit lamp biomicroscopy, dilated fundus examination, IOP (using contact tonometer), OCT measurement (Spectralis OCT, Heidelberg Engineering, Heidelberg, Germany), and AL and CCT measurements.
BCVA levels were measured using Snellen acuity testing. AL and CCT were measured before cycloplegia. AL was measured with the Axis II A-scan contact biometer (Quantel Medical, Auvergne, France). CCT measurements were obtained in a noncontact manner using the Sirius Scheimpflug Analyzer (CSO, Costruzione Strumenti Oftalmici, Florence, Italy). Cycloplegia was induced by instilling three drops of cyclopentolate 1% at 5-min intervals. Cycloplegic refraction was measured 45 min after the last drop. The spherical equivalent (SE=spherical error + 1/2 of cylindrical error) was calculated from the average refractive error values.
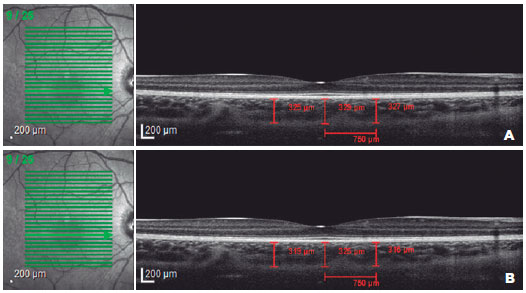
OCT analysis, in addition to CT measurement, was performed by the same experienced operator. All measurements were made between 10 AM and 2 PM to limit the potential confounding influence of diurnal variations on CT. Macular and peripapillary RNFL examinations were performed using an internal fixator. MT and peripapillary RNFLT parameters were automatically calculated by the OCT device. RNFLT parameters were divided into seven regions including temporal quadrant thickness (90º), temporal superior quadrant thickness (45º), nasal superior quadrant thickness (45º), nasal quadrant thickness (90º), nasal inferior quadrant thickness (45º), temporal inferior quadrant thickness (45º), and average thickness (360º). After the exposures, noncentered scans and scans with signal strength <20 dB were excluded from the study(2). Then, for each participating child, high-resolution linear OCT scan lines, at a rate of 4.7/s using the automatic real-time tracker mode and centered on the fovea, were captured using the instrument's Enhanced Depth Imaging (EDI) mode. The OCT image scan angle was 20º and image sizes were 5.9 mm × 1.9 mm. Scans with quality index values >20 dB were used for analysis(8). CT was measured at the fovea, 750 µ nasal, and 750 µ temporal to the fovea by two independent examiners. Borders of the choroid were defined as the outer aspect of Bruch's membrane and the outmost identifiable hyper-reflective layer between the choroid-sclera junction (Figure 1 A, B). Interexaminer agreement for the CT measurements was also calculated.
Statistical analysis
Statistical analyses were performed using IBM SPSS for Windows Version 22.0 statistical package. Continuous variables were presented as mean ± standard deviation and categorical variables were summarized as frequencies and percentages. Differences between the two raters according to continuous measures were determined using the paired t-test. Agreement between the two raters was represented by the intraclass correlation coefficient. Pearson or Spearman correlation coefficients were used to show the relationships between continuous variables. Independent samples t-test was used to verify gender differences. A p value of <0.05 was regarded as significant.
Before calculating the reference intervals, extreme values were excluded according to the Tukey test. The Shapiro-Wilk test was used to assess the normality of variables. The 95% reference intervals were established using the parametric (based on normal distribution) or nonparametric method (based on CLSI (Clinical and Laboratory Standards Institute) C28-A3 standard) for the obtained data as appropriate. Percentiles were calculated as observations corresponding to rank r=p* (n+1).
RESULTS
The study included 72 girls and 48 boys. The mean age was 11.95 ± 2.26 (range 8-15) years. All patients had a visual acuity of 1.0 bilaterally. The mean global RNFLT was 98.75 ± 9.45 (79-121) µ (Table 1). The mean CMT was 232.29 ± 29.37 (190-376; reference range 195.12-300.95) µ. The mean subfoveal CT was measured as 344.38 ± 68.83 (148-572; reference range 201.14-444.87) µ by examiner 1 and 344.04 ± 68.92 (141-573) µ by examiner 2 (Table 2). Interexaminer agreement was 99.6%-99.8% for CT at three separate locations. There was no difference between the genders in the OCT parameters (p>0.05 for all).
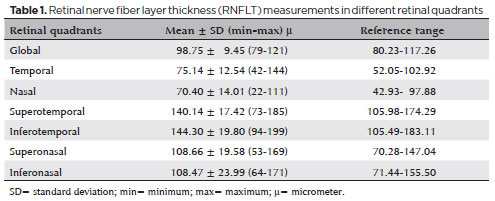
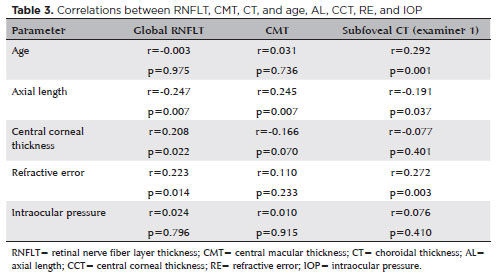
CMT was found to increase with AL (r=0.245, p=0.007) (Table 3). CT was demonstrated to increase with age (r=0.292, p=0.001) and to decrease with AL (r=-0.191, p=0.037). Global RNFLT was found to decrease with AL (r=-0.247, p=0.007) and to increase with CCT (r=0.208, p=0.022). Global RNFLT was also positively correlated with CT (r=0.354, p<0.001). CMT was not correlated with global RNFLT or subfoveal CT (p>0.05). In addition, global RNFLT (r=0.223, p=0.014) and CT (r=0.272, p=0.003) were found to increase with refractive error. There was no correlation between intraocular pressure and OCT parameters (p>0.05 for all).
DISCUSSION
OCT, which has been one of the most commonly used technique in ophthalmology clinics for many years, offers qualitative and quantitative data regarding anterior and posterior segments of the eye. Quantitative measurements may be further processed according to age-based normative data depending on the particular software used and a classification of normal, borderline, or abnormal may be suggested such as in cases of RNFLT analysis in glaucoma. Therefore, the normative range and database used for OCT parameters are critically important for the interpretation of the numerical data. As OCT is performed mainly on adults, the OCT database represents and compares the values for adults. However, due to the increasing use of OCT in children, an age-appropriate database is needed.
Several studies found differences between genders in some OCT parameters, such as increased CMT in men(7,9-11) and increased RNFLT in women(12). Similar to the present study, other studies found no differences between genders(3,4,13).
Age-related decreases in retinal thickness(3), in RNFLT(3,4,14), and in CT(5,15) have been reported. However, varied results have been presented in the pediatric group. Table 4 shows RNFLT values from different studies involving children(2,13,14). Turk et al.(2) reported that OCT measurements did not significantly correlate with age while Yanni et al.(14) noted that CMT significantly correlated with age. Leung et al.(1) emphasized that the effect of age on RNFLT was not significant. In the study by Al-Haddad et al.(10), RNFLT measurements did not correlate with age whereas all macular parameters showed consistent positive correlations with age. Barrio-Barrio et al.(11) reported a positive correlation between CMT and age in their study. Park and Oh(16) suggested that the mean subfoveal CT in children was relatively thick in comparison with previous studies on healthy adults; in addition subfoveal CT showed a significant negative correlation with age (16). Chhablani et al.(17) argued that age is a critical factor negatively correlated with CT. In the present study, there was a weak positive correlation only between subfoveal CT and age. The results should be analyzed in light of the fact that the study included children only aged 8-15 years. Li et al.(18) emphasized that the choroid thickness may increase during puberty despite the axial elongation of the eye.
Several published reports showed that RNFLT(1,12,19) and CMT(19) negatively correlated with AL whereas others asserted that AL was not associated with RNFLT(2) and CMT(9,20) in children. In the present study, CMT increased with AL and global RNFLT was decreased with AL. Hence, the disc diameter decreases when AL increases. The scanning circle will therefore be further away from the optic disc margin, which could result in a thinner RNFLT measured by OCT(1). Furthermore, CT negatively correlated with AL in the present study. Similar to the other parameters, there are contradictory reports about CT and AL correlation. Some authors found a negative correlation between CT and AL(17,20), whereas others reported no correlation(16) in children.
It has been argued that as CT measurements are obtained with operator-directed caliper positioning, they are prone to variability and are even more variable in children(17). In the present study, CT was measured by two independent examiners in three separate locations and the interexaminer agreement was 99.6%-99.8%.
In the present study, global RNFLT and subfoveal CT positively correlated with their spherical equivalents, similar to some other studies in the literature(5,20). However, children with high refractive errors were not included in this study. Furthermore, there was no correlation between intraocular pressure and OCT parameters. Unlike the present study, Jin et al.(20) reported that CMT increased with intraocular pressure and that global RNFLT increased with CCT.
In the present study, all participants received a detailed examination, and both AL and CCT were recorded. However, the limitations of the study include a uniform ethnic group and the fact that patients with high refractive errors were excluded. Hence, normative data for other groups were not determined.
In the present study, we presented normative value ranges for OCT parameters and interexaminer agreement for CT measurements in children. Normative reference ranges for each of the SD-OCT parameters for children in different ethnic populations will improve our ability to diagnose pediatric disorders affecting the retina, optic disc, and choroid. It is worthy of note that an age-appropriate database should be taken into consideration while interpreting OCT values. Despite being prone to variability, CT measurements may be made with a high level of interexaminer agreement.
REFERENCES
1 Leung MM, Huang RY, Lam AK. Retinal nerve fiber layer thickness in normal Hong Kong chinese children measured with optical coherence tomography. J Glaucoma. 2010;19(2):95-9.
2 Turk A, Ceylan OM, Arici C, Keskin S, Erdurman C, Durukan AH, et al. Evaluation of the nerve fiber and macula in the eyes of healthy children using spectral-domain optical coherence tomography. Am J Ophthalmol. 2012;153(3):552-9. Comment in: Am J Ophthalmol. 2012;153(4):774; author reply 774-5.
3 Alamouti B, Funk J. Retinal thickness decreases with age: an OCT study. Br J Ophthalmol. 2003;87(7):899-901.
4 Schuman JS, Hee MR, Puliafito CA, Wong C, Pedut-Kloizman T, Lin CP, et al. Quantification of nerve fiber layer thickness in normal and glaucomatous eyes using optical coherence tomography. Arch Ophthalmol. 1995;113(5):586-96.
5 Shao X, Zou C, Qin B. Correlation of choroidal thickness and ametropiain young adolescence. PLoS ONE. 2017;12(4):e0174385.
6 Sull AC, Vuong LN, Price LL, Srinivasan Vj, Gorczynska I, Fujimoto JG, et al. Comparison of spectral/Fourier domain optical coherence tomography instruments for assessment of normal macular thickness. Retina. 2010;30(2):235-45.
7 Adhi M, Aziz S, Muhammad K, Adhi MI. Macular thickness by age and gender in healthy eyes using spectral domain optical coherence tomography. PLoS ONE. 2012;7(5):e37638.
8 Read SA, Collins MJ, Vincent SJ, Alonso-Caneiro D. Choroidal thickness in myopic and nonmyopic children assessed with enhanced depth imaging optical coherence tomography. Invest Ophthalmol Vis Sci. 2013;54(12):7578-86.
9 Huynh SC, Wang XY, Rochtchina E, Mitchell P. Distribution of macular thickness by optical coherence tomography: findings from a population-based study of 6-year-old children. Invest Ophthalmol Vis Sci. 2006;47(6):2351-7.
10 Al-Haddad C, Barikian A, Jaroudi M, Massoud V, Tamim H, Noureddin B. Spectral domain optical coherence tomography in children: normative data and biometric correlations. BMC Ophthalmol. 2014;14:53.
11 Barrio-Barrio J, Noval S, Galdós M, Ruiz-Canela M, Bonet E, Capote M, et al. Multicenter Spanish study of spectral-domain optical coherence tomography in normal children. Acta Ophthalmol. 2013;91(1):e56-63.
12 Zhu BD, Li SM, Li H, Liu LR, Wang Y, Yang Z, Li SY, Kang MT, Fu J, Qi YH, Zhan SY, Wang N; Anyang Childhood Eye Study Group. Retinal nerve fiber layer thickness in a population of 12-year-old children in central China measured by iVue-100 spectral-domain optical coherence tomography: the Anyang Childhood Eye Study. Invest Ophthalmol Vis Sci. 2013;54(13):8104-11.
13 Pérez-García D, Ibañez-Alperte J, Remón L, Cristóbal JÁ, Sanchez-Cano A, Pinilla I. Study of spectral-domain optical coherence tomography in children: normal values and influence of age, sex, and refractive status. Eur J Ophthalmol. 2016;26(2):135-41.
14 Yanni SE, Wang J, Cheng CS, et al. Normative reference ranges for the retinal nerve fiber layer, macula, and retinal layer thicknesses in children. Am J Ophthalmol. 2013;155(2):354-60.
15 Margolis R, Spaide RF. A pilot study of enhanced depth imaging optical coherence tomography of the choroid in normal eyes. Am J Ophthalmol. 2009;147(5):811-5.
16 Park KA, Oh SY. Choroidal thickness in healthy children. Retina. 2013;33(9):1971-6.
17 Chhablani JK, Deshpande R, Sachdeva V, Vidya S, Rao OS, Panigati A, et al. Choroidal thickness profile in healthy Indian children. Indian J Ophthalmol. 2015;63(6):474-7. Comment in: Indian J Ophthalmol. 2016;64(1):100-1.
18 Li XQ, Jeppesen P, Larsen M, Munch IC. Subfoveal choroidal thickness in 1323 children aged 11 to 12 years and association with puberty: the Copenhagen Child Cohort 2000 Eye Study. Invest Ophthalmol Vis Sci. 2014;55(1):550-5.
19 El-Dairi MA, Asrani SG, Enyedi LB, Freedman SF. Optical coherence tomography in the eyes of normal children. Arch Ophthalmol. 2009; 127(1):50-8.
20 Jin P, Zou H, Zhu J, Xu X, Jin J, Chang TC, et al. Choroidal and retinal thickness in children with different refractive status measured by swept-source optical coherence tomography. Am J Ophthalmol. 2016;168:164-76.
Submitted for publication:
February 23, 2017.
Accepted for publication:
October 8, 2017.
Funding: No specific financial support was available for this study.
Approved by the following research ethics committee: Hacettepe University (# GO16/255).