

Hande Celiker1; Ebru Toker1; Tulin Ergun2;Leyla Cinel3
DOI: 10.5935/0004-2749.20170097
ABSTRACT
Rosacea is a chronic, progressive disease of unknown cause affecting the eye and the facial skin. Ocular rosacea is often underdiagnosed if the ophthalmologist does not inspect the patient's face adequately during the ocular examination. Severe ocular complications and blindness can occur if the treatment is delayed because of non-diagnosis of the rosacea. Here, we present a case of ocular rosacea in a 78-year-old Caucasian woman. Based on the ocular lesions, which preceded cutaneous involvement, she was misdiagnosed as having ocular cicatricial pemphigoid initially. This case emphasizes the difficulty in diagnosis when ocular findings precede those of skin manifestations, and rosacea should be kept in mind in the differential diagnosis of chronic cicatrizing conjunctivitis.
Keywords: Rosacea/diagnosis; Rosacea/complications; Rosacea/drug therapy; Diagnosis, differential; Pemphigoid, benign mucous membrane; Eye diseases/diagnosis
RESUMO
A rosácea é uma doença crônica e progressiva de causa desconhecida que afeta o olho e a pele do rosto. A rosácea ocular é muitas vezes pouco diagnosticada se o oftalmologista não inspecionar adequadamente o rosto do paciente durante o exame ocular. Podem ocorrer complicações oculares graves e cegueira se o tratamento for adiado devido ao não diagnóstico da rosácea. Um caso de rosácea ocular em uma mulher caucasiana de 78 anos de idade é apresentado. Com base nas lesões oculares, que precederam o envolvimento cutâneo, ela foi mal diagnosticada como penfigóide cicatricial ocular inicialmente. Este caso enfatiza a dificuldade de diagnóstico quando os achados oculares precedem aqueles das manifestações da pele e um diagnóstico de rosácea deve ser mantido em mente no diagnóstico diferencial da conjuntivite cicatrizante crônica.
Descritores: Rosácea/diagnóstico; Rosácea/complicações; Rosácea/tratamento farmacológico; Diagnóstico diferencial; Penfigóide mucomembranoso benigno; Oftalmopatias/diagnóstico
INTRODUCTION
Rosacea is a cutaneous disorder presenting with facial flushes, erythema, papules, pustules, and telangiectasias(1). Ocular changes, ranging from mild dryness and irritation with blepharitis and conjunctivitis to sight-threatening keratitis, are present in more than 50% of patients(2). According to the National Rosacea Society Expert Committee, the disease is classified into four main nosologic subtypes (erythematotelangiectatic, papulopustular, phymatous, and ocular)(3). Immune system dysfunction, Demodex folliculorum infestation, environmental factors such as sunlight, and vascular anomalies have been implicated in its pathogenesis(4).
Here, we report a patient with ocular rosacea (OR), who had severe sight-threatening ocular symptoms prior to the onset of skin lesions.
CASE REPORT
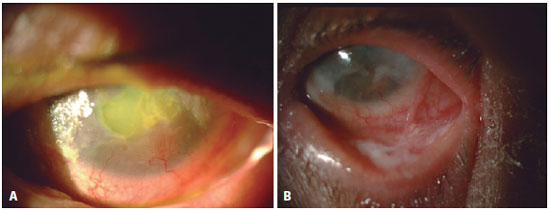
A 78-year-old woman presented with a five-month history of redness, irritation, and blepharospasm in both eyes. She initially presented to an ophthalmologist with the complaint of blepharospasm, and the ophthalmologist diagnosed her with conjunctivitis, glaucoma, and dry eye. She was using artificial tears, dorzolamide/timolol combination, and dexamethasone eye drops. Her visual acuity (VA) could not be measured because of blepharospasm. The conjunctiva was chemotic bilaterally. There were round, deep, and well-demarcated corneal epithelial defects (EDs) of approximately 7 × 6 mm in the right eye (RE) (Figure 1 A) and 5 × 5 mm in the left eye (LE) with stromal excavation, and heavy corneal neovascularization (CN). Thickening of the lid margin and dense keratin plaques were seen bilaterally, and infratemporal forniceal symblepharon involving the LE with forniceal foreshortening was noted (Figure 1 B). Corneal swabs were taken for microbiological tests. Based on the ophthalmic findings and the age of the patient, the initial diagnosis at that time was ocular cicatricial pemphigoid (OCP). She was administered moxifloxacin eye drops and autologous plasma five times a day, cyclopentolate hydrochloride 1% (Sikloplejin® Eye Drop, Abdi Ibrahim Medicine and Health Production Company Inc. Istanbul, Turkey) twice a day, and carboxymethylcellulose eye drops (Refresh® Eye Drop, Allergan Medicine and Health Production Company Inc., Irvine, CA, USA) every hour for both the eyes. Bandage soft contact lenses (PureVision, Bausch & Lomb, Rochester, NY, USA) were applied to help corneal tissue recovery. A matrix-regenerating agent (RGA) (Cacicol® Eye Drop, Théa Laboratories, Clermont-Ferrand, France) was initiated once in 24 hours to promote epithelial healing.
Bacterial culture, polymerase chain reaction (PCR) for herpesvirus, histopathological tests, and direct immunofluorescent tests were performed for a definitive diagnosis. Herpesvirus infection was excluded owing to a negative PCR result. Bacterial culture revealed Staphylococcus aureus species. She underwent conjunctival biopsy with preoperative 0.1 ml triamcinolone acetonide injection to the inferior subconjunctival area in the LE. Histopathological examination of the conjunctiva revealed lymphocytic infiltration in the subepithelial area (Figure 2 A) without blister formation. Ocular cicatricial pemphigoid (OCP) was also excluded owing to the lack of linear/granular subepithelial deposition of immunoglobulin (Ig)-G and C3 in the basement membrane zone on direct immunofluorescent testing. Serum anti-BP180 and anti-BP230 antibodies were negative. The patient's ocular examination findings did not improve during this period. Topical cyclosporine 0.05% (Restasis® Eye Drop, Allergan Medicine and Health Production Company Inc.) five times a day was added to the treatment.
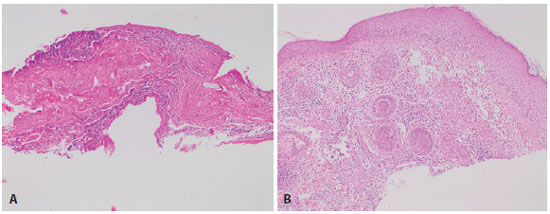
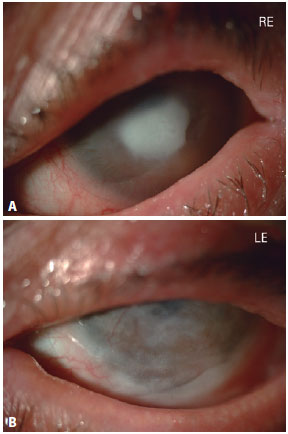
During follow-up, she developed erythematous papules and pustules over the cheeks, chin, and forehead. Dermatological consultation suggested a diagnosis of rosacea, which was proven histopathologically with enlarged, dilated capillaries and venules located in the upper dermis, angulated telangiectasias, perivascular and perifollicular lymphocytic infiltration, and superficial dermal edema (Figure 2 B). Treatment with doxycycline 100 mg capsule (Tetradox® Capsule Actavis Ltd., UK) once daily combined with topical metronidazole cream was initiated. After three months of treatment, her skin lesions disappeared substantially, and the itching and stinging sensation, redness, blepharospasm, and discharge subsided gradually. The VA was hand movements for both the eyes. Biomicroscopic examination revealed an ED of 3 × 2 mm in the RE and punctate keratoepitheliopathy with a dense central corneal scar and mid-peripheral CN in the LE. Symblepharon, which was located infratemporally in the LE, regressed (Figure 3). Doxycycline treatment was discontinued owing to a satisfactory response. One month later, she experienced an increase in itching and stinging. Physical examination revealed papulopustular lesions on the face and an increase in telangiectatic appearance. The cornea showed a 4 × 4-mm, round, deep, corneal ulcer in the RE, and heavy CN in the LE (Figure 4). Amnion grafting was performed for the corneal ulcer in the RE, and doxycycline 100 mg twice daily was reinitiated. Microscopic evaluation was performed through examination of eyelash roots. Demodex folliculorum was found in the eyelash follicles on direct microscopic examination, and a tea-tree oil-based cleansing solution (Blefaritto® Eye Shampoo 100 ml, Jeomed Medicine and Health Production Company Inc., Ankara, Turkey) was initiated for demodicosis. During follow-up, the ED healed with a persistent vascularized dense scar, and penetrating keratoplasty was planned for both the eyes.

DISCUSSION
In rosacea, ocular involvement is less easily recognized and often remains underdiagnosed, despite serious complications. Its symptoms and signs can be quite non-specific, and in up to 90% of patients, accompanying skin changes may be very subtle(5). Akpek et al. reported 131 patients with a diagnosis of OR(6). Twelve of these patients were referred because of cicatrizing conjunctivitis in order to rule out OCP. In this case, we experienced a diagnostic dilemma owing to the presence of the clinical features of OCP. However, the conjunctival biopsy specimen did not show histopathological changes consistent with OCP. According to Thorne et al., rosacea blepharoconjunctivitis is responsible for 20% of presumed causes of ocular pseudopemphigoid(7). OR was included in the differential diagnosis when the patient developed erythematotelangiectatic papular and pustular skin lesions. OR is often underdiagnosed by ophthalmologists especially when skin manifestations are not evident. In approximately 20% of patients, eye changes may precede skin changes; however, half of the patients develop skin lesions first, while one-third develop both manifestations simultaneously(2). Severe ocular complications and permanent loss of vision can occur if treatment is delayed because of non-diagnosis of OR. As in the present case, dermatological consultation for both diagnosis and management is invaluable. The ophthalmologist often does not inspect the patient's face adequately during ocular examination(8). This negligence may confound the diagnosis and delay appropriate treatment; thus, severe eye complications may lead to blindness. In a previous report, a patient had developed redness and itching in both eyes three months prior to the onset of skin lesions, and this condition worsened over the subsequent six years, eventually leading to the need for keratoplasty(9).
There are no histopathological or laboratory tests of this disease. The diagnosis depends on evaluation of clinical signs, which are mostly non-specific. Response to a therapeutic trial of oral tetracycline may be helpful in confirming a tentative diagnosis(2). In the present case, after discontinuation of the drug, early recurrence of the disease was noted; therefore, our diagnosis was confirmed.
In conclusion, OR should be kept in mind in the differential diagnosis of chronic cicatrizing conjunctivitis. The lack of skin lesions may cause difficulty in the diagnosis of OR.
REFERENCES
1. Powell FC. Rosacea. N Engl J Med. 2005;352(8):793-803.
2. Browning DJ, Proia AD. Ocular rosacea. Surv Ophthalmol. 1986;31(3):145-58.
3. Wilkin J, Dahl M, Detmar M, Drake L, Feinstein A, Odom R, et al. Standard classification of rosacea: report of the National Rosacea Society Expert Committee on the classification and staging of rosacea. J Am Acad Dermatol. 2002;46(4):584-87.
4. Crawford GH, Pelle MT, James WD. Rosacea: I. Etiology, pathogenesis and subtype classification. J Am Acad Dermatol. 2004;51(3):327-41; quiz 342-4.
5. Vieira AC, Höfling-Lima AL, Mannis MJ. Ocular rosacea--a review. Arq Bras Oftalmol. 2012;75(5):363-9.
6. Akpek EK, Merchant A, Pinar V, Foster S. Ocular rosacea. Patient characteristics and follow-up. Ophthalmology. 1997;104(11):1863-67.
7. Thorne JE, Anhalt GJ, Jabs DA. Mucous membrane pemphigoid and pseudopemphigoid. Ophthalmology. 2004;111(1):45-52.
8. Macsai MS, Mannis MJ, Huntley AC. Acne rosacea. In: Mannis MJ, Macsai MS, Huntley AC, editors. Eye and skin disease. Philadelphia: Lippincott-Raven; 1996. p.335-341.
9. Subashini K, Pushpa G, Venugopal V, Murali N. Rosacea with severe ophthalmic involvement and blindness - a rare occurrence. Int J Dermatol. 2012;51(10):1271-3.
Submitted for publication:
January 18, 2017.
Accepted for publication:
August 8, 2017.
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: None of the authors have any potential conflict of interest to disclose.