

Marcio Henrique Mendes1; Alberto Jorge Betinjane1; Veronica Andrea Quiroga1
DOI: 10.1590/S0004-27492013000600007
ABSTRACT
PURPOSE: To identify the correlation between the difference of intraocular pressure measurements (IOP) obtained using the Goldmann applanation tonometer (GAT) and three others tonometers (Handheld applanation tonometer - HAT, Dynamic contour tonometer - DCT and Tono-Pen®) with biometric characteristics (corneal diameter, pachymetry, keratometry and axial length) in patients with congenital glaucoma. METHODS: A cross-sectional study was performed on 46 eyes from 46 patients with congenital glaucoma. IOP measurements were obtained in all patients using GAT, HAT, DCT and Tono-Pen®. Keratometry, pachymetry, biometry and corneal diameter measurements were performed after the IOP measurement. The order of the tonometries was randomized. The correlations between the differences of IOP values of GAT and the other tonometers (Delta-IOP), and the different biometric parameters were studied. RESULTS: Tono-Pen® Delta IOP revealed moderate positive correlation to keratometry (r=0.41, p=0.004). The other Delta-IOPs showed no correlation with any of the biometric characteristics evaluated. CONCLUSIONS: IOP differences between GAT (gold standard) and GAT, HAT, DCT or Tono-Pen tonometers seem not to correlate with majority of ocular biometric characteristics. The only exception was the keratometry, which correlated in a positive and moderate way with Tono-Pen® Delta-IOP. This result suggests that the differences of IOP values of Tono-Pen® and GAT increase with the steepness of the cornea.
Keywords: Tonometry, ocular; Biometry; Glaucoma; Intraocular pressure
RESUMO
OBJETIVOS: Identificar correlações entre as diferenças de medições de pressão intraocular (IOP) obtidas usando o tonômetro de aplanação de Goldmann (GAT) e três outros tonômetros (Tonômetro portátil de aplanação - TPA, Tonômetro de contorno dinâmico - TCD e Tono-Pen®) com características biométricas (diâmetro corneano, paquimetria, ceratometria e comprimento axial) em pacientes com glaucoma congênito. MÉTODOS: Estudo transversal prospectivo foi realizado em 46 olhos de 46 pacientes com glaucoma congênito. As medidas de pressão intraocular foram obtidas em todos os pacientes utilizando TAG, TPA, TCD e Tono-Pen®. Ceratometria, paquimetria, biometria e diâmetro corneano foram realizadas após mensuração da pressão intraocular. A ordem da utilização tonômetros foi aleatória. Correlações entre as diferenças de valores de PIO entre cada um dos três tonômetros (PIOs Delta) e o tonômetro de Goldmann e as características biométricas foram analisadas. RESULTADOS: PIO Delta do Tono-Pen®revelou correlação positiva moderada com ceratometria (r=0,41, p=0,004). As outras PIOs Delta não se correlacionaram significativamente com nenhuma das características biométricas. CONCLUSÕES: As diferenças entre as PIOs obtidas pelo TAG (padrão ouro) e TPA, TCD e Tono-Pen®parece não se correlacionar com a maioria das características biométricas. A única exceção foi a ceratometria, a qual se correlacionou de forma positiva e moderada com a PIO Delta do Tono-Pen®. Estes resultados indicam que o aumento da diferença entre a PIO obtida com TAG e Tono-Pen®aumenta com o encurvamento da curvatura corneana.
Descritores: Tonometria ocular; Biometria; Glaucoma; Pressão intraocular
ORIGINAL ARTICLE
Correlations between different tonometries and ocular biometric parameters in patients with primary congenital glaucoma
Correlações entre diferentes tonometrias e parâmetros biométricos oculares em pacientes com glaucoma congênito primário
Marcio Henrique Mendes; Alberto Jorge Betinjane; Veronica Andrea Quiroga
Physician, Department of Ophthalmology, Faculdade de Medicina, Universidade de São Paulo - USP - São Paulo (SP), Brazil
ABSTRACT
PURPOSE: To identify the correlation between the difference of intraocular pressure measurements (IOP) obtained using the Goldmann applanation tonometer (GAT) and three others tonometers (Handheld applanation tonometer - HAT, Dynamic contour tonometer - DCT and Tono-Pen®) with biometric characteristics (corneal diameter, pachymetry, keratometry and axial length) in patients with congenital glaucoma.
METHODS: A cross-sectional study was performed on 46 eyes from 46 patients with congenital glaucoma. IOP measurements were obtained in all patients using GAT, HAT, DCT and Tono-Pen®. Keratometry, pachymetry, biometry and corneal diameter measurements were performed after the IOP measurement. The order of the tonometries was randomized. The correlations between the differences of IOP values of GAT and the other tonometers (Delta-IOP), and the different biometric parameters were studied.
RESULTS: Tono-Pen® Delta IOP revealed moderate positive correlation to keratometry (r=0.41, p=0.004). The other Delta-IOPs showed no correlation with any of the biometric characteristics evaluated.
CONCLUSIONS: IOP differences between GAT (gold standard) and GAT, HAT, DCT or Tono-Pen tonometers seem not to correlate with majority of ocular biometric characteristics. The only exception was the keratometry, which correlated in a positive and moderate way with Tono-Pen® Delta-IOP. This result suggests that the differences of IOP values of Tono-Pen® and GAT increase with the steepness of the cornea.
Keywords: Tonometry, ocular/methods; Biometry/methods; Glaucoma/congenital; Intraocular pressure
RESUMO
OBJETIVOS: Identificar correlações entre as diferenças de medições de pressão intraocular (IOP) obtidas usando o tonômetro de aplanação de Goldmann (GAT) e três outros tonômetros (Tonômetro portátil de aplanação - TPA, Tonômetro de contorno dinâmico - TCD e Tono-Pen®) com características biométricas (diâmetro corneano, paquimetria, ceratometria e comprimento axial) em pacientes com glaucoma congênito.
MÉTODOS: Estudo transversal prospectivo foi realizado em 46 olhos de 46 pacientes com glaucoma congênito. As medidas de pressão intraocular foram obtidas em todos os pacientes utilizando TAG, TPA, TCD e Tono-Pen®. Ceratometria, paquimetria, biometria e diâmetro corneano foram realizadas após mensuração da pressão intraocular. A ordem da utilização tonômetros foi aleatória. Correlações entre as diferenças de valores de PIO entre cada um dos três tonômetros (PIOs Delta) e o tonômetro de Goldmann e as características biométricas foram analisadas.
RESULTADOS: PIO Delta do Tono-Pen®revelou correlação positiva moderada com ceratometria (r=0,41, p=0,004). As outras PIOs Delta não se correlacionaram significativamente com nenhuma das características biométricas.
CONCLUSÕES: As diferenças entre as PIOs obtidas pelo TAG (padrão ouro) e TPA, TCD e Tono-Pen®parece não se correlacionar com a maioria das características biométricas. A única exceção foi a ceratometria, a qual se correlacionou de forma positiva e moderada com a PIO Delta do Tono-Pen®. Estes resultados indicam que o aumento da diferença entre a PIO obtida com TAG e Tono-Pen®aumenta com o encurvamento da curvatura corneana.
Descritores: Tonometria ocular/métodos; Biometria/métodos; Glaucoma/congênito; Pressão intraocular
INTRODUCTION
Intraocular pressure (IOP) reduction is currently the only effective treatment for glaucoma(1-4); thus, good tonometric accuracy is of great importance in the majority of cases. IOP measurement may be affected by some factors, such as corneal curvature, thickness and biomechanical characteristics (hysteresis).
Goldmann applanation tonometry (GAT) is considered the gold standard for IOP measurement; however, the characteristics of this equipment restrict its use in children who are not cooperative and must be examined under general anesthesia in an operating room. Other tonometers, such as electronic applanation tonometers (EAT), like the Tono-Pen®, and Handheld applanation tonometers (HAT), like the Perkins® tonometer, can be used in clinical practice to minimize these restrictions. These instruments may help to examine children under these conditions.
Tonometry in eyes with congenital glaucoma (CG) is more susceptible to misinterpretation because of the extreme corneal alterations found in many CG patients(5-7).
Previous studies have demonstrated that central corneal thickness and keratometric changes can lead to false results in adults(5-8). The dynamic contour tonometer (DCT) was developed with the aim of minimizing corneal effects in IOP readings(9).
Because considerable pachymetric and keratometric changes are frequently found in patients with CG(10-12), the purpose of this study was to identify the correlations between IOP measurements obtained with the GAT, HAT, DCT and Tono-Pen® with biometric characteristics (central corneal thickness, mean keratometry, axial length and corneal diameter) in patients with CG.
METHODS
Patients aged 12 to 40 years who had the diagnosis of congenital glaucoma and were followed by the Ophthalmology Department of the University of São Paulo Medical School were eligible to participate in this study. Subjects with diffuse, moderate or severe local edema or moderate or severe corneal opacification were excluded. Institutional Review Board approval was obtained for the study protocol. Informed consent was obtained from all of the subjects or their parents. All 46 patients presented reasonable or good corneal transparency conditions, although Haab's striae or slight sectorial edema was observed in some patients. All eyes underwent IOP measurements using four different instruments: GAT (Haag-Streit®, Koeniz, Switzerland), DCT (Pascal®, SMT® Swiss microtechnology, Port, Switzerland), HAT (Perkins® Tonometer, Haag-Streit® AG, Koeniz, Switzerland) and Tono-Pen® (Tono-Pen®, Medtronic Solan®, Jacksonville, FL, USA) at the same appointment. The order of the exams was randomized. Keratometry, pachymetry, biometry and corneal diameter measurements were performed after the IOP measurement.
Descriptive analyses were performed for all tonometry types and biometric characteristics. Correlation between the difference of IOP values from GAT and the other tonometers (Delta-IOP) with the biometric parameters was performed.
The Pearson product-moment coefficient was used to evaluate correlation. Values were defined as follows: weak (0 to 0.4), moderate (0.4 to 0.75) and strong (greater than 0.75).
Paired t test was performed to analyze statistical differences between the tonometric mean obtained with each tonometer.
Scatter plot of the difference between GAT and other tonometer versus biometric parameters were presented.
The statistical analyses were performed with Microsoft Excel for Windows (Microsoft®, Redmond, Washington, USA). Results are presented as Mean ± Standard Deviation and Range.
RESULTS
The ocular biometric characteristics of the sample are described as follow: central corneal thickness (585.9 ± 87.89 µm, 432 to 861 µm), average keratometry (42.01 ± 2.45 D, 34.6 to 46.4 D), axial length (25.44 ± 2.01 mm, 21.54 to 34.06 mm) and corneal diameter (12.81 ± 1.29 mm, 10 to 15.5 mm).
The mean IOP measurements were 12.95 ± 4.63 mmHg (GAT), 12.49 ± 4.85 mmHg (HAT), 13.26 ± 4.28 mmHg (DCT) and 13.06 ± 4.9 mmHg (Tono-Pen®).
There were no significant differences in tonometric values between the DCT and GAT (p=0.30) or between the Tono-Pen® and GAT (p=0.68). There was a significant difference between the means of the GAT and HAT (p=0.0001).
Table 1 shows all of the Pearson product-moment correlation coefficients obtained from the analysis of the Delta-IOPs with biometric parameters.
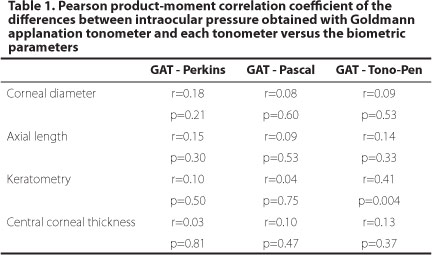
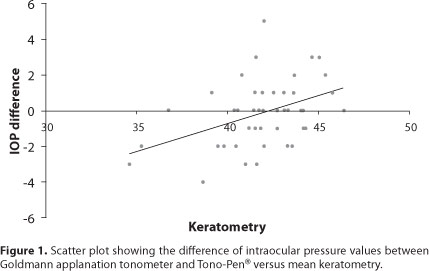
The majority of correlations between Delta-IOP and central corneal thickness, keratometry, axial length and corneal diameter were weak or not significant. The only exception was the positive moderate correlation between Tono-Pen® Delta-IOP and keratometry (Figure 1).
DISCUSSION
Correct IOP measurement is important for the diagnosis and follow-up of the majority of congenital glaucoma cases. However, it is often very difficult to determine the IOP in these patients because of the common corneal abnormalities found in this disease, or their inability to cooperate adequately with tonometry. These situations often require the use of others tonometers.
The HAT has operating characteristics similar to those of GAT. The contact and applanation systems of both are virtually identical. Therefore, the IOP measurements obtained with both tonometers are expected to have similar results with respect to the modification of ocular conditions.
The DCT was designed to fit the corneal contour and produce continuous, real IOP values through its central electromechanical reading system, thus minimizing the error related to corneal changes (mean keratometry and thickness) in the tonometric measurements.
The Tono-Pen® was developed to allow IOP measurement with the patient in any position. It uses a central tip that requires contact with the corneal surface, activating its reading microprocessor. In this case, for each touch on the corneal surface, repeated electronic measurements (4 to 10) are considered to provide the final IOP result. This procedure was repeated three times, revealing the mean of these measurements and its variation in percentage (5-20%).
Patients with severe corneal abnormalities and dense or generalized edema were excluded from this study because these characteristics could lead to major and non-quantifiable measurement errors.
Patients younger than 12 years of age were excluded from this study because underage individuals often do not cooperate with the examination or require examination under anesthesia. These situations could contribute to inaccurate tonometric values.
Differences in central corneal thickness are one of the main sources of error in applanation tonometry(13-16). There is no agreement about the adjustment factor. Studies have demonstrated errors from 0.19 to 0.7 mmHg for each 10 µm of deviation at the 520 µm mean(6,17), but the obtained IOP was correlated with pachymetry in an extensive number of studies. Our results indicate no correlation between the central corneal thickness and the Delta-IOP of each tonometer. The DCT did not reveal any difference in the results of pachymetry compared with the GAT results. This finding can be attributed to the considerable changes in the corneal biomechanical characteristics (stromal abnormalities) in this sample.
A positive correlation between the IOP and axial length or increased myopia has been reported(18-20). The corneal diameter is the other biometric parameter mentioned as a factor that influences the IOP, but few studies have examined this issue(8,21,22).
In this study, the differences between the IOP results obtained with the three tonometers compared with those obtained with the GAT did not present any correlation with pachymetry, biometry and corneal diameter, meaning that the increase or decrease of any parameter did not influence the difference in tonometry readings.
The corneal curvature appears to influence the IOP reading (an increase of 3 diopters overestimates 1 mmHg)(14,23) because the greater the corneal curvature, the higher the pressure needed to applanate the corneal surface. Our study detected a moderate positive correlation between keratometry and Tono-Pen® Delta-IOP.
Using mathematic simulation models, other authors have demonstrated that the IOP can be influenced by corneal biomechanical variations of up to 17 mmHg. Those authors have demonstrated that pachymetry was responsible for 2.87 mmHg of this entire variation and that keratometry was responsible for 1.76 mmHg. These results suggest that biomechanical properties have more influence on the IOP than central corneal thickness and corneal curvature isolated in the normal population(24).
Our results suggest that the modifications in the corneal stroma biomechanical structure (such as Haab's striae formation) may lead to changes in the expected correlations between the IOP and biometric parameters.
IOP differences between GAT (gold standard) and GAT, HAT, DCT or Tono-Pen tonometers seem not to correlate with majority of ocular biometric characteristics. The only exception was the keratometry, which correlated in a positive and moderate way with Tono-Pen® Delta-IOP. This result suggests that the differences of IOP values of Tono-Pen® and GAT increase with the steepness of the cornea. Therefore, the use of these three other tonometers can be accepted without restrictions attributed to the often biometric characteristics alterations found in these patients.
REFERENCES
1. Kass MA, Heuer DK, Higginbotham EJ, Johnson CA, Keltner JL, Miller JP, et al. The Ocular Hypertension Treatment Study: a randomized trial determines that topical ocular hypotensive medication delays or prevents the onset of primary open-angle glaucoma. Arch Ophthalmol. 2002;120(6):701-13; discussion 829-30.
2. Comment in Arch Ophthalmol. 2003;121(7):1070; author reply 1070. Arch Ophthalmol. 2004;122(7):1088-9; author reply 1089.
3. The Advanced Glaucoma Intervention Study (AGIS): 7. The relationship between control of intraocular pressure and visual field deterioration. The AGIS Investigators. Am J Ophthalmol. 2000;130(4):490-1.
4. Shields MB, Ricth R, Krupin T. Classifications of the glaucomas. In: Ritch R, Shields MB, Krupin T. The glaucomas. 2nd ed. St. Louis: CV Mosby; 1989. Vol. 2, p. 717-25.
5. Dickens CS, Hoskins HD. Diagnosis and treatment of congenital g laucoma. In: Ritch R, Shields MB, Krupin T. The glaucomas. 2nd ed. St. Louis: CV Mosby; 1989.Vol. 2, p.739-52.
6. Doughty MJ, Zaman ML. Human corneal thickness and its impact on intraocular pressure measures: a review and meta-analysis approach. Surv Ophthalmol. 2000; 44(5):367-408.
7. Wolfs RC, Klaver CC, Vingerling JR, Grobbee DE, Hofman A, de Jong PT. Distribution of central corneal thickness and its association with intraocular pressure: the Rotterdam Study. Am J Ophtalmol. 1997;123(6):767-72.
8. Whitacre MM, Stein RA, Kassanein K. The effect of corneal thickness on applanation tonometry. Am J Ophthalmol. 1993;115(5):592-6.
9. Brandt JD, Beiser JA, Kass MA, Gordon MO. Central corneal thickness in the Ocular Hypertension Treatment Study (OHTS). Ophthalmology. 2001;108(10):1779-88.
10. Martinez-de-la-Casa JM, Garcia-Feijoo J, Vico E, Fernandez-Vidal A, Benitez del Castillo JM, Wasfi M, et al. Effect of corneal thickness on dynamic contour, rebound, and goldmann tonometry. Ophthalmology. 2006;113(12):2156-62.
11. Tai TY, Mills MD, Beck AD, Joos KM, Ying GS, Liu C, et al. Central corneal thickness and corneal diameter in patients with childhood glaucoma. J Glaucoma. 2006;15(6):524-8.
12. Henriques MJ, Vessani RM, Reis FA, de Almeida GV, Betinjane AJ, Susanna R Jr. Corneal thickness in congenital glaucoma. J Glaucoma. 2004;13(3):185-8.
13. Mendes MH, Sakata L, Betinjane AJ. Espessura corneana central e suas correlações com outros dados biométricos oculares em pacientes portadores de glaucoma congênito. Arq Bras Oftalmol. 2011;74(2):85-7.
14. Martinez-de-la-Casa JM, Garcia-Feijoo J, Fernandez-Vidal A, Mendez-Hernandez C, Garcia-Sanchez J. Ocular response analyzer versus Goldmann applanation tonometry for intraocular pressure measurements. Invest Ophthalmol Vis Sci. 2006; 47(10):4410-4.
15. Mark HH. Corneal curvature in applanation tonometry. Am J Ophthalmol. 1973;76(2): 223-4.
16. Argus WA. Ocular hypertension and central corneal thickness. Ophthalmology. 1995;102(12):1810-2. Comment in Ophthalmology. 2001;108(8):1364-6.
17. Herndon LW, Choudhri SA, Cox T, Damji KF, Shields MB, Allingham RR. Central corneal thickness in normal, glaucomatous, and ocular hypertensive eyes. Arch Ophthalmol. 1997;115(9):1137-41. Comment in Arch Ophthalmol. 1998;116(4):544-5. Arch Ophthalmol. 1998;116(5):701. Arch Ophthalmol. 1998;116(9):1263.
18. Ehlers N, Bramsen T, Sperling S. Applanation tonometry and central corneal thickness. Acta Ophthalmol (Copenh). 1975;53(1):34-43.
19. David R, Zangwill L, Stone D, Yassur Y. Epidemiology of intraocular pressure in a population screened for glaucoma. Br J Ophthalmol. 1987;71(10):766-71.
20. Tomlinson A, Philips CI. Applanation tension and axial length of the eyeball. Br J Ophthalmol. 1970;54(8):548-53.
21. David R, Zangwill LM, Tessler Z, Yassur Y. The correlation between intraocular pressure and refractive status. Arch Ophthalmol. 1985;103(12):1812-5.
22. Bhan A, Browning AC, Shah S, Hamilton R, Dave D, Dua HS. Effect of corneal thikness on intraocular pressure measurements with the pneumotonometer, Goldmann applanation tonometer and Tono-Pen. Invest Ophthalmol Vis Sci. 2000;43(5):1389-92.
23. Bron AM, Creuzot-Garcher C, Goudeau-Boutillon S, d'Athis P. Falsely elevated intraocular pressure due to increased corneal thickness. Graefes Arch Clin Exp Ophthalmol. 1999;237(3):220-4.
24. Morad Y, Sharon E, Hefetz L, Nemet P. Corneal thickness and curvature in normal-tension glaucoma. Am J Ophthalmol. 1998;125(2):164-8. Comment in Am J Ophthalmol. 1998;126(2):326-8.
25. Liu J, Roberts CJ. Influence of corneal biomechanical properties on intraocular pressure measurement: quantitative analysis. J Cataract Refract Surg. 2005;31(1):146-55. Comment in J Cataract Refract Surg. 2006;32(7):1073-4; author reply 1074.
 Correspondence:
Correspondence:
Marcio H. Mendes
Rua Barata Ribeiro, 380/36 São Paulo (SP)
01308-000 - Brazil
E-mail: [email protected]
Submitted for publication: March 4, 2013
Accepted for publication: August 21, 2013
Funding: No specific financial support was available for this study.
Disclosure of potential conflicts of interest: M.H.Mendes, None; A.J.Betinjane, None; V.A.Quiroga, None.
Study carried out at Department of Ophthalmology, Faculdade de Medicina, Universidade de São Paulo - USP - São Paulo (SP), Brazil.