

Mirella Telles Salgueiro Barboni1; Claudia Feitosa-Santana1; Jackson Barreto Junior1; Marcos Lago1; Samir Jacob Bechara1; Milton Ruiz Alves1; Dora Fix Ventura1
DOI: 10.1590/S0004-27492013000500003
ABSTRACT
PURPOSE: The present study aimed to compare the postoperative contrast sensitivity functions between wavefront-guided LASIK eyes and their contralateral wavefront-guided PRK eyes. METHODS: The participants were 11 healthy subjects (mean age=32.4 ± 6.2 years) who had myopic astigmatism. The spatial contrast sensitivity functions were measured before and three times after the surgery. Psycho and a Cambridge graphic board (VSG 2/4) were used to measure luminance, red-green, and blue-yellow spatial contrast sensitivity functions (from 0.85 to 13.1 cycles/degree). Longitudinal analysis and comparison between surgeries were performed. RESULTS: There was no significant contrast sensitivity change during the one-year follow-up measurements neither for LASIK nor for PRK eyes. The comparison between procedures showed no differences at 12 months postoperative. CONCLUSIONS: The present data showed similar contrast sensitivities during one-year follow-up of wave-front guided refractive surgeries. Moreover, one year postoperative data showed no differences in the effects of either wavefront-guided LASIK or wavefront-guided PRK on the luminance and chromatic spatial contrast sensitivity functions.
Keywords: Luminance contrast sensitivity; Chromatic contrast sensitivity; Refractive surgery; WFG-LASIK; WFG-PRK
RESUMO
OBJETIVO: A proposta do presente estudo é comparar funções de sensibilidade ao contraste obtidas após wavefront-LASIK e wavefront-PRK no olho contralateral. MÉTODOS: Os participantes foram 11 sujeitos saudáveis (idade média=32,4 ± 6,2 anos) com astigmatismo miópico. As funções de sensibilidade ao contraste espacial foram obtidas antes e três vezes após a cirurgia. O programa Psycho e uma placa gráfica da Cambridge Research Systems (VSG 2/4) permitiram gerar os estímulos com contraste espacial de luminância e cromático (verde-vermelho e azul-amarelo) de 0,85 até 13,1 ciclos/grau. Análises longitudinais e comparações entre as cirurgias foram realizadas. RESULTADOS: Não houve mudança significativa da sensibilidade ao contraste durante o primeiro ano após a cirurgia para o olho que recebeu o LASIK ou para o olho que recebeu o PRK. A comparação entre as cirurgias também foi semelhante no pós-operatório de um ano. CONCLUSÕES: Os resultados apresentados mostraram sensibilidade ao contraste semelhante durante o primeiro ano após a cirurgia refrativa com o wavefront. Além disso, no pós-operatório de um ano não houve diferença nas funções de sensibilidade ao contraste de luminância e cromático entre os olhos que receberam LASIK e os que receberam PRK.
Descritores: Sensibilidade ao contraste de luminância; Sensibilidade ao contraste cromático; Cirurgia refrativa; WFG-LASIK; WFG-PR
ORIGINAL ARTICLE ARTIGO ORIGINAL
Longitudinal measurements of luminance and chromatic contrast sensitivity: comparison between wavefront-guided LASIK and contralateral PRK for myopia
Medidas longitudinais da sensibilidade ao contraste de luminância e cromático: comparação entre wavefront-LASIK e wavefront-PRK para miopia
Mirella Telles Salgueiro BarboniI,II; Claudia Feitosa-SantanaI,II; Jackson Barreto JuniorI; Marcos LagoI,II; Samir Jacob BecharaI; Milton Ruiz AlvesI; Dora Fix VenturaI,II
IPhD, Universidade de São Paulo, São Paulo (SP), Brazil
IIPsychologist, Universidade de São Paulo, Institute of Psychology, São Paulo (SP), Brazil
ABSTRACT
PURPOSE: The present study aimed to compare the postoperative contrast sensitivity functions between wavefront-guided LASIK eyes and their contralateral wavefront-guided PRK eyes.
METHODS: The participants were 11 healthy subjects (mean age=32.4 ± 6.2 years) who had myopic astigmatism. The spatial contrast sensitivity functions were measured before and three times after the surgery. Psycho and a Cambridge graphic board (VSG 2/4) were used to measure luminance, red-green, and blue-yellow spatial contrast sensitivity functions (from 0.85 to 13.1 cycles/degree). Longitudinal analysis and comparison between surgeries were performed.
RESULTS: There was no significant contrast sensitivity change during the one-year follow-up measurements neither for LASIK nor for PRK eyes. The comparison between procedures showed no differences at 12 months postoperative.
CONCLUSIONS: The present data showed similar contrast sensitivities during one-year follow-up of wave-front guided refractive surgeries. Moreover, one year postoperative data showed no differences in the effects of either wavefront-guided LASIK or wavefront-guided PRK on the luminance and chromatic spatial contrast sensitivity functions.
Keywords: Luminance contrast sensitivity; Chromatic contrast sensitivity; Refractive surgery; WFG-LASIK; WFG-PRK
RESUMO
OBJETIVO: A proposta do presente estudo é comparar funções de sensibilidade ao contraste obtidas após wavefront-LASIK e wavefront-PRK no olho contralateral.
MÉTODOS: Os participantes foram 11 sujeitos saudáveis (idade média=32,4 ± 6,2 anos) com astigmatismo miópico. As funções de sensibilidade ao contraste espacial foram obtidas antes e três vezes após a cirurgia. O programa Psycho e uma placa gráfica da Cambridge Research Systems (VSG 2/4) permitiram gerar os estímulos com contraste espacial de luminância e cromático (verde-vermelho e azul-amarelo) de 0,85 até 13,1 ciclos/grau. Análises longitudinais e comparações entre as cirurgias foram realizadas.
RESULTADOS: Não houve mudança significativa da sensibilidade ao contraste durante o primeiro ano após a cirurgia para o olho que recebeu o LASIK ou para o olho que recebeu o PRK. A comparação entre as cirurgias também foi semelhante no pós-operatório de um ano.
CONCLUSÕES: Os resultados apresentados mostraram sensibilidade ao contraste semelhante durante o primeiro ano após a cirurgia refrativa com o wavefront. Além disso, no pós-operatório de um ano não houve diferença nas funções de sensibilidade ao contraste de luminância e cromático entre os olhos que receberam LASIK e os que receberam PRK.
Descritores: Sensibilidade ao contraste de luminância; Sensibilidade ao contraste cromático; Cirurgia refrativa; WFG-LASIK; WFG-PR
INTRODUCTION
The visual performance for perception of fine detail depends on both neural factors of the visual system and on the optical quality of the eyes(1). Conventional refractive surgeries, for defocus and astigmatism correction, are known to change the optical quality of the eye(2) by modifying corneal curvature, therefore, increasing aberrations, diffractions, and scatter light in the optical system(3). These changes may cause a reduction in the contrast sensitivity and halos, as a result, a set of symptoms such as night vision disturbances may be referred by the subjects during the postoperative evaluation(4).
It has been shown that the emerging refractive surgery technologies based on wavefront analysis avoid high order aberrations besides eliminating refractive errors(5-7). Spatial contrast sensitivity thresholds measured after refractive surgeries for myopia were significantly improved after wavefront-guided (WFG) LASIK eyes compared with the performance of conventional LASIK eyes, despite their postoperative normal visual acuity which remained similar for both techniques(5). The implication is that a more sensitive visual test, such as the measurement of contrast sensitivity thresholds for a range of spatial frequencies, has the ability to detect visual abnormalities in subjects with normal visual acuity but complaining of visual disturbances. The measurement of luminance contrast sensitivity function enables a wide spectrum of the spatial visual performance to be estimated, while visual acuity tests usually determines only one extreme point of the function(1,8). In addition, chromatic contrast sensitivity function might be measured to verify the possibility of threshold changes due to chromatic aberrations(7).
A study comparing the quality of vision after conventional LASIK and PRK showed that both techniques achieved similar results in low-contrast visual acuity tests at one year postoperatively(9). Previously, we found no visual disturbance for either WFG-LASIK eyes or contralateral WFG-PRK eyes in measures of intraocular straylight and contrast sensitivity using VCTS 6500 charts one year postoperatively(10). In order to evaluate whether luminance and chromatic spatial contrast sensitivity thresholds may be impaired after WFG refractive surgeries and to indicate whether LASIK and PRK may affect differently this visual function, we performed a longitudinal evaluation - preoperative, and 3, 6, and 12 months postoperative - of luminance, red-green, and blue-yellow spatial contrast sensitivity functions after WFG-LASIK in one eye and WFG-PRK in the contralateral eye.
METHODS
The study was performed in accordance with the tenets of the Declaration of Helsinki and the procedures were approved by the Ethics Committee of the Institute of Psychology and of the Medical School (University of São Paulo). All participants provided informed consent. This is a prospective randomized study of 22 eyes of 11 participants (6 males and 5 females; mean age=32.4 ± 6.2 years) with mean preoperative spherical equivalent refraction of -2.50 (±0.99) diopters in the WFG-LASIK eyes and -2.35 (±0.93) diopters in the WFG-PRK eyes. The inclusion criteria were: corrected distance visual acuity ≥0.0 logMAR, spherical equivalent refraction <5.00 diopters, no preexisting ocular pathology, previous surgery, and ages between 21 and 40 years. The wavefront analysis was performed using the OPDCAT platform (NIDEK Co Ltd, Gamagori, Japan) with a 5.0-mm optical zone and an additional 3.5 mm transition zone(10). All participants were operated by the same physician and they were randomized to receive WFG-LASIK in one eye and WFG-PRK in the contralateral eye. The pupil size was 6 mm and all participants were at least 15 days without their contact lenses.
Psychophysical experiments were performed as described in detail in previous studies(11,12) using Psycho for Windows V2.36 software and a graphic board VSG 2/4 (Cambridge Research System, Cambridge, UK). This system generated the stimuli on a 19-inches FD Trinitron CRT monitor with 100 Hz frame rate, 800x600 pixels spatial resolution (Sony Electronics, Tokyo, Japan). The luminance stimuli consisted of horizontal sinusoidal achromatic gratings (4x4º square field) displayed on a mean luminance grey background (34.4 cd/m2) and presented at five spatial frequencies: 0.85, 2.62, 4.76, 7.93, and 13.1 cycles/degree (cpd). The red-green and blue-yellow stimuli consisted of horizontal sinusoidal equiluminant gratings (4x4º square field) presented at four spatial frequencies: 0.85, 2.62, 4.76, and 7.93 cpd displayed against a background having the same mean luminance and the mean chromaticity of the stimulus. The highest contrast was provided by the following chromaticity points: red u'=0.258, v'=0.454; green u'=0.133, v'=0.469; blue u'=0.210, v'=0.397; and yellow u'=0.188, v'=0.551 (CIE 1976).
The test consisted of a sequence of five spatial frequencies (for the luminance test) and four spatial frequencies (for the chromatic tests). The program presented a certain contrast at each spatial frequency and the subject responded "yes" if he/she perceived the stimulus and "no" if he/she did not perceive the stimulus using keyboard keys. This procedure continued until a response had been recorded for all spatial frequencies in a random sequence. In each subsequent sequence, the contrast was changed for each spatial frequency according to a staircase procedure. The contrast sensitivity was estimated using the values of the lowest contrast which produced a positive response. At the end of the test, after 35 sequences, the programme produced the contrast sensitivity threshold for each spatial frequency by taking the mean of, at least, six reversal trials. The equiluminant condition was obtained with a previous measurement of the heterochromatic flicker photometry (20 Hz). The red-green and blue-yellow stimuli were equated in luminance using this measurement.
According to Shapiro-Wilk test there was statistical difference between our data and the normal distribution, therefore, we used the nonparametric Sign Test to compare contrast sensitivity thresholds between eyes and the ANOVA with Post Hoc Tukey test to compare the longitudinal data (Stastistica 6.0, StatSoft, USA). The level of significance accepted was p<0.05.
RESULTS
All participants (22 eyes) were tested before the surgery and at 12 months follow-up. At 3 months follow-up 10 participants (20 eyes) were tested and at 6 months follow-up eight participants (16 eyes) were tested.
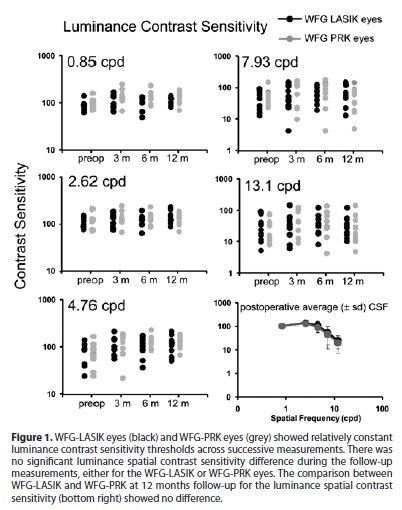
Figure 1 shows longitudinal results of luminance contrast sensitivity thresholds at five spatial frequencies. At the lowest spatial frequency (0.85 cpd) the thresholds remained very similar throughout the follow-up for the WFG-LASIK eyes (black) while the WFG-PRK eyes showed higher thresholds and more variability (grey). At 2.62 cpd and 4.76 cpd the results showed higher thresholds in the 12 months measurements for both WFG-LASIK eyes and WFG-PRK eyes. At higher spatial frequencies (7.93 cpd and 13.1 cpd) WFG-LASIK eyes showed relatively constant contrast sensitivity thresholds and WFG-PRK eyes showed a fluctuation across measurements, with no significant difference between the results from WFG-LASIK eyes and WFG-PRK eyes (p>0.05; Sign test). In addition, there were no significant differences in the luminance contrast sensitivity follow-up for either WFG-LASIK or WFG-PRK eyes (preoperative vs three months: p>0.7; preoperative vs six months: p>0.6; and three months vs six months: p>0.8; ANOVA with Post Hoc Tukey test). The comparison between WFG-LASIK and WFG-PRK one year after the surgeries (Figure 1, last graph) also showed no differences in the luminance contrast sensitivity function (p>0.05; Sign test).
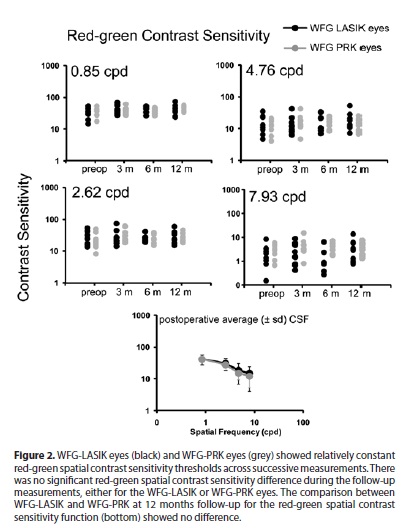
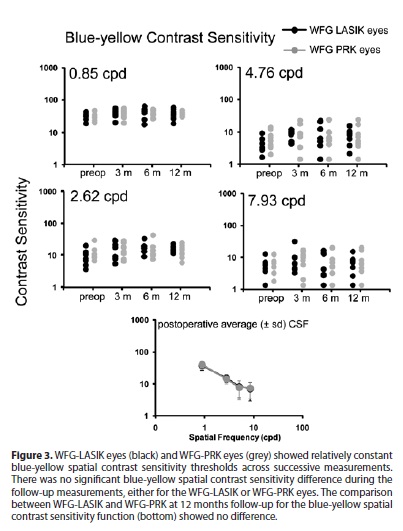
Red-green (Figure 2) and blue-yellow (Figure 3) contrast sensitivity thresholds were also quite similar throughout the follow-up with no statistical differences for both techniques (p>0.05; Sign test). There were no significant changes in the red-green contrast sensitivity thresholds for WFG-LASIK eyes (preoperative vs three months: p>0.8, preoperative vs six months: p>0.6, and three months vs six months: p>0.9; ANOVA with Post Hoc Tukey test) or WFG-PRK eyes (preoperative vs three months: p>0.2, preoperative vs six months: p>0.7, and three months vs six months: p>0.3; ANOVA with Post Hoc Tukey test). Blue-yellow contrast sensitivity thresholds did not show statistical differences for WFG-LASIK eyes (preoperative vs three months: p>0.2, preoperative vs six months: p>0.2, and three months vs six months: p>0.7; ANOVA with Post Hoc Tukey test) or WFG-PRK (preoperative vs three months: p>0.2, preoperative vs six months: p>0.6, and three months vs six months: p>0.3; ANOVA with Post Hoc Tukey test) during the follow-up. The comparison between WFG-LASIK eyes and WFG-PRK eyes one year after the surgeries showed similar red-green and blue-yellow thresholds (p>0.2; Sign test; Figures 2 and 3, last graphs), as found for the luminance thresholds.
One subject showed contrast sensitivity thresholds decreased at 12 months follow-up compared with preoperative measurements for the higher spatial frequencies in both eyes in the luminance, red-green, and blue-yellow contrast sensitivity functions. A participant had lower thresholds in the WFG-LASIK eye and another participant had lower thresholds in the WFG-PRK eye at 12 months after the surgeries for the luminance test. Two other participants showed lower thresholds in the red-green contrast sensitivity function in both WFG-LASIK and WFG-PRK eyes comparing the preoperative measurement with the 12 months postoperative measurement. These changes were not statistically significant. Six participants (54.5% of the subjects) had equal or better contrast sensitivity thresholds comparing preoperative and 12 months postoperative measurements in both eyes at all spatial frequencies tested for the luminance, red-green, and blue-yellow tests.
DISCUSSION
Contrast sensitivity functions may be considered a more detailed measurement to study the quality of vision since it provides information that is not accessible by standard clinical visual acuity tests(8). The present study showed that WFG refractive surgeries (LASIK and PRK) did not significantly impair luminance or chromatic contrast sensitivity thresholds in the range of spatial frequencies tested (0.85 cpd to 13.1 cpd). Moreover, the psychophysical performance after WFG-LASIK and WFG-PRK surgery did not differ for luminance and chromatic spatial contrast sensitivity at 12 months follow-up. From 11 subjects tested in the present study, six showed equal or higher contrast sensitivity thresholds at all spatial frequencies tested one year after the surgeries, either in the luminance or in the chromatic protocols. The other five participants showed similar results but with lower thresholds at some spatial frequencies tested. However these differences were not statistically significant.
The radial keratotomy (RK) and the conventional PRK were shown to reduce contrast sensitivity thresholds(13). The conventional LASIK, known to provide a better visual outcome and shorter recovery time than RK and conventional PRK techniques, shows temporary depression of contrast sensitivity thresholds(14). A previous study(15) performed measurements of luminance contrast sensitivity using the same stimulus generator and software used in the present study. They also studied longitudinal measurements (one year follow-up) testing seven spatial frequencies (from 0.3 cpd to 20.5 cpd), nevertheless a higher mean luminance compared to the present study was used. The authors only tested luminance contrast sensitivity thresholds in conventional LASIK eyes and they found significantly depressed thresholds after surgery with a return to normal values after six months.
In the present study of WFG surgeries no significant contrast sensitivity depression was found after WFG-LASIK for any spatial frequency tested, even in the first measurement after the surgery (three months postoperative), indicating that conventional LASIK and WFG-LASIK may have different effect on luminance contrast sensitivity function. This is in agreement with one study showing significantly improved contrast sensitivity thresholds after WFG-LASIK compared to conventional LASIK one month after surgery(5). The wavefront analysis enabled to measure individual patterns of optical aberrations and allowed their correction during refractive surgical procedures(16,17). Here we showed that it also has an effect in the quality of vision.
The use of luminance stimuli to measure contrast sensitivity thresholds is more typical and it has shown to be a valuable tool for testing the quality of vision after refractive surgeries(4,18), however, less is known about the effects of refractive surgeries on chromatic contrast sensitivity thresholds. Red-green and blue-yellow contrast sensitivity for a range of spatial frequencies can be measured by matching the luminance content of the two colors in the stimulus and in this case it is possible to obtain an equiluminant condition(19). As found for the luminance domain, the human visual system depends on the optical integrity, besides the neural factors, to present the expected performance in chromatic visual tasks. The present study showed that WFG-LASIK and WFG-PRK did not affect red-green and blue-yellow contrast sensitivity functions in the range of spatial frequencies tested and among the follow-up measured, in agreement with luminance contrast sensitivity results.
Even with no depression of contrast sensitivity thresholds, or any other ophthalmological abnormality after WFG refractive surgeries, some subjects may complain of visual disturbances. A transitory straylight elevation that may persist for some months postoperatively has been previously found in the same subjects studied here(10). In this case, the intraocular straylight may be a more sensitive test to characterize and quantify the subjective visual experiences after refractive surgical procedures.
The data presented here may be considered as a preliminary result, since 11 is a limited number of subjects. Nevertheless, one should consider the homogeneity of the sample tested. The investigators team and the equipments as well as the surgical procedures and the application of the tests were not changed during the follow-up. The contrast sensitivity thresholds obtained after refractive surgical procedures were compared with their own preoperative results instead of comparing with a database of normal subjects, since there is potential interindividual threshold variability. In addition, one eye was compared with the fellow eye. In this case it was possible to compare the individual fluctuation of thresholds and the subjective visual symptoms individually. Another consideration is that the subjects tested in the present study had an average age of 32.4 (±6.2) years old and an average refractive error of -2.50 ± 0.99 diopters (WFG-LASIK eyes) and -2.35 ± 0.93 diopters (WFG-PRK eyes). Different results might have been found in another age group or in subjects with higher spherical equivalent refraction.
Some consideration may be taking into account when comparing the benefits of WFG-PRK and WFG-LASIK. In surface ablation, the benefits of the WFG treatment may be masked by epithelial hyperplasia. Micro sculptures are made on the anterior surface of the cornea in order to provide an asymmetric and customized correction. However, the customized ablation can be penalized by the action of compensatory epithelial hyperplasia, a common finding in the surface ablations healing process which may mask the effects of such micro sculptures(20). On the other hand, LASIK may induce new ocular aberrations only by making the flap(21). In the present study it was not determinative to favor one or another technique since the luminance and chromatic spatial contrast sensitivity were similar for both LASIK and PRK eyes.
The present study reported the effects of WFG refractive surgeries on spatial contrast sensitivity functions and showed no luminance and chromatic spatial contrast sensitivity impairment in subjects who underwent simultaneous WFG-LASIK and contralateral WFG-PRK. Moreover, one year postoperative data showed no difference between WFG-LASIK eyes and WFG-PRK eyes in the luminance and chromatic spatial contrast sensitivity functions.
REFERENCES
1. Campbell FW, Green DG. Optical and retinal factors affecting visual acuity. J Physiol. 1965;181(3):576-93.
2. Holladay JT, Dudeja DR, Chang J. Functional vision and corneal changes after laser in situ keratomileusis determined by contrast sensitivity, glare testing, and corneal topography. J Cataract Refract Surg. 1999;25(5):663-9.
3. Seiler T, Kaemmerer M, Mierdel P, Krinke HE. Ocular optical aberrations after photorefractive keratectomy for myopia and myopic astigmatism. Arch Ophthalmol. 2000; 118(1):17-21.
4. McLeod SD. Beyond snellen acuity: the assessment of visual function after refractive surgery. Arch Ophthalmol. 2001;119(9):1371-3.
5. Kaiserman I, Hazarbassanov R, Varssano D, Grinbaum A. Contrast sensitivity after wave front-guided LASIK. Ophthalmology. 2004;111(3):454-7.
6. Mrochen M, Kaemmerer M, Seiler T. Clinical results of wavefront-guided laser in situ keratomileusis 3 months after surgery. J Cataract Refract Surg. 2001;27(2):201-7.
7. Schwiegerling J. Theoretical limits to visual performance. Surv Ophthalmol. 2000; 45(2):139-46.
8. Arden GB. Importance of measuring contrast sensitivity in cases of visual disturbance. Br J Ophthalmol. 1978;62(4):198-209.
9. Neeracher B, Senn P, Schipper I. Glare sensitivity and optical side effects 1 year after photorefractive keratectomy and laser in situ keratomileusis. J Cataract Refract Surg. 2004;30(8):1696-701.
10. Barreto J Jr, Barboni MT, Feitosa-Santana C, Sato JR, Bechara SJ, Ventura DF, et al. Intraocular straylight and contrast sensitivity after contralateral wavefront-guided LASIK and wavefront-guided PRK for myopia. J Refract Surg. 2009;26(8):588-93.
11. Ventura DF, Quiros P, Carelli V, Salomao SR, Gualtieri M, Oliveira AG, et al. Chromatic and luminance contrast sensitivities in asymptomatic carriers from a large Brazilian pedigree of 11778 leber hereditary optic neuropathy. Invest Ophthalmol Vis Sci. 2005; 46(12):4809-14.
12. Ventura DF, Simoes AL, Tomaz S, Costa MF, Lago M, Costa MT, et al. Colour vision and contrast sensitivity losses of mercury intoxicated industry workers in Brazil. Environ Toxicol Pharmacol. 2005;19(3):523-9.
13. Ghaith AA, Daniel J, Stulting RD, Thompson KP, Lynn M. Contrast sensitivity and glare disability after radial keratotomy and photorefractive keratectomy. Arch Ophthalmol. 1998;116(1):12-8.
14. Mutyala S, McDonald MB, Scheinblum KA, Ostrick MD, Brint SF, Thompson H. Contrast sensitivity evaluation after laser in situ keratomileusis. Ophthalmology. 2000;107(10):1864-7.
15. Chan JW, Edwards MH, Woo GC, Woo VC. Contrast sensitivity after laser in situ keratomileusis. One-year follow-up. J Cataract Refract Surg. 2002;28(10):1774-9. Comment in: J Cataract Refract Surg. 2003;29(9):1650-1; J Cataract Refract Surg. 2002; 28(10):1717-18.
16. Chalita MR, Chavala S, Xu M, Krueger RR. Wavefront analysis in post-LASIK eyes and its correlation with visual symptoms, refraction, and topography. Ophthalmology. 2004;111(3):447-53. Comment in: Ophthalmology. 2005;112(6):1171; author reply 1171.
17. Schallhorn SC, Farjo AA, Huang D, Boxer Wachler BS, Trattler WB, Tanzer DJ, Majmudar PA, Sugar A; American Academy of Ophthalmology. Wavefront-guided LASIK for the correction of primary myopia and astigmatism a report by the American Academy of Ophthalmology. Ophthalmology. 2008;115(7):1249-61.
18. Montes-Micó R, Charman WN. Choice of spatial frequency for contrast sensitivity evaluation after corneal refractive surgery. J Refract Surg. 2001;17(6):646-51.
19. Mullen KT. The contrast sensitivity of human colour vision to red-green and blue-yellow chromatic gratings. J Physiol. 1985;359:381-400.
20. Netto MV, Wilson SE. Corneal wound healing relevance to wavefront guided laser treatments. Ophthalmol Clin North Am. 2004;17(2):225-31.
21. Porter J, MacRae S, Yoon G, Roberts C, Cox IG, Williams DR. Separate effects of the microkeratome incision and laser ablation on the eye's wave aberration. Am J Ophthalmol. 2003;136(2):327-37.
 Correspondence address:
Correspondence address:
Mirella Telles Salgueiro Barboni.
Instituto de Psicologia - Universidade de São Paulo.
Av. Prof. Mello Moraes, 1.721 - Bloco D - Sala 206
São Paulo (SP) - 05508-030 - Brazil
E-mail: [email protected]
Submitted for publication: April 2, 2012
Accepted for publication: July 31, 2013
Study carried out at Universidade de São Paulo, São Paulo (SP), Brazil
Funding: This research was supported by grants from Brazilian research funding agencies: FAPESP, CNPq, CAPES; and FINEP IBN-Net. MTSB, CFS, and JB Jr were supported by doctoral FAPESP fellowships and CFS by a postdoctoral fellowship: NIH EY-04802. CFS is an IMB fellow (University of Chicago) research fellow. DFV is a CNPq research fellow.
Disclosure of potential conflicts of interest: M.T.S.Barboni, None; C.Feitosa-Santana, None; J.Barreto Junior, None; M.Lago, None; S.J.Bechara, None; M.R.Alves, None; D.F.Ventura, None.