INTRODUCTION
As a procedure, laser-assisted in situ keratomileusis (LASIK) is not free of complications. These complications are specifically related to the creation and presence of a corneal flap. Buttonholes, incomplete flaps, free caps, and lacerations that occur during flap creation(1), as well as the postoperative onset of interface folds(2), flap displacement(3), flap delamination(4), epithelial ingrowth(5) at the interface, and diffuse lamellar keratitis(6) (DLK), remain an area of concern with respect to LASIK procedures. An early description of DLK referred to it as a sandy deposit of whitish material on the flap’s interface; as such, this nonspecific inflammatory condition was first known as “Sands of Sahara Syndrome.”
Previous studies have reported that the incidence of DLK varies from 0.67%(7) to 0.81%(8) and that it may develop in response to primary LASIK, following enhancements without the use of microkeratomes(9) or in flap creation using a femtosecond laser(10), mainly occurring during outbreaks (as was noted in 64% of cases)(7). Because this is a noninfectious condition, many factors have been proposed as causes of DLK and the etiological factors have not always been identified(11).
The Ishikawa diagram, also called a cause-and-effect diagram, Fishbone diagram, or root cause analysis, was invented by Kaoru Ishikawa (1969), who first used the technique in the 1960s. This tool is a diagram that shows the causes of a certain event, and it is considered one of the seven basic tools of quality management. A common application of the Ishikawa diagram is in product design, wherein it is used to identify desirable factors leading to an overall effect. When the fishbone diagram is drafted, one has a complete picture of all possible root causes of the designated problem(12). The purpose of this study was to determine the causes of a DLK outbreak by employing the Ishikawa diagram in a case-control analysis.
METHODS
The Ishikawa diagram was adopted for this investigation. The source of DLK outbreak served as the central effect in this visual brainstorming approach. With respect to the possible causes of DLK outbreak, we listed “staff personnel,” “materials,” “equipment,” “instruments,” “medications,” “solutions,” “patients,” and “environment” as the primary categories. Subcategories for each major cause can be visualized in figure 1.
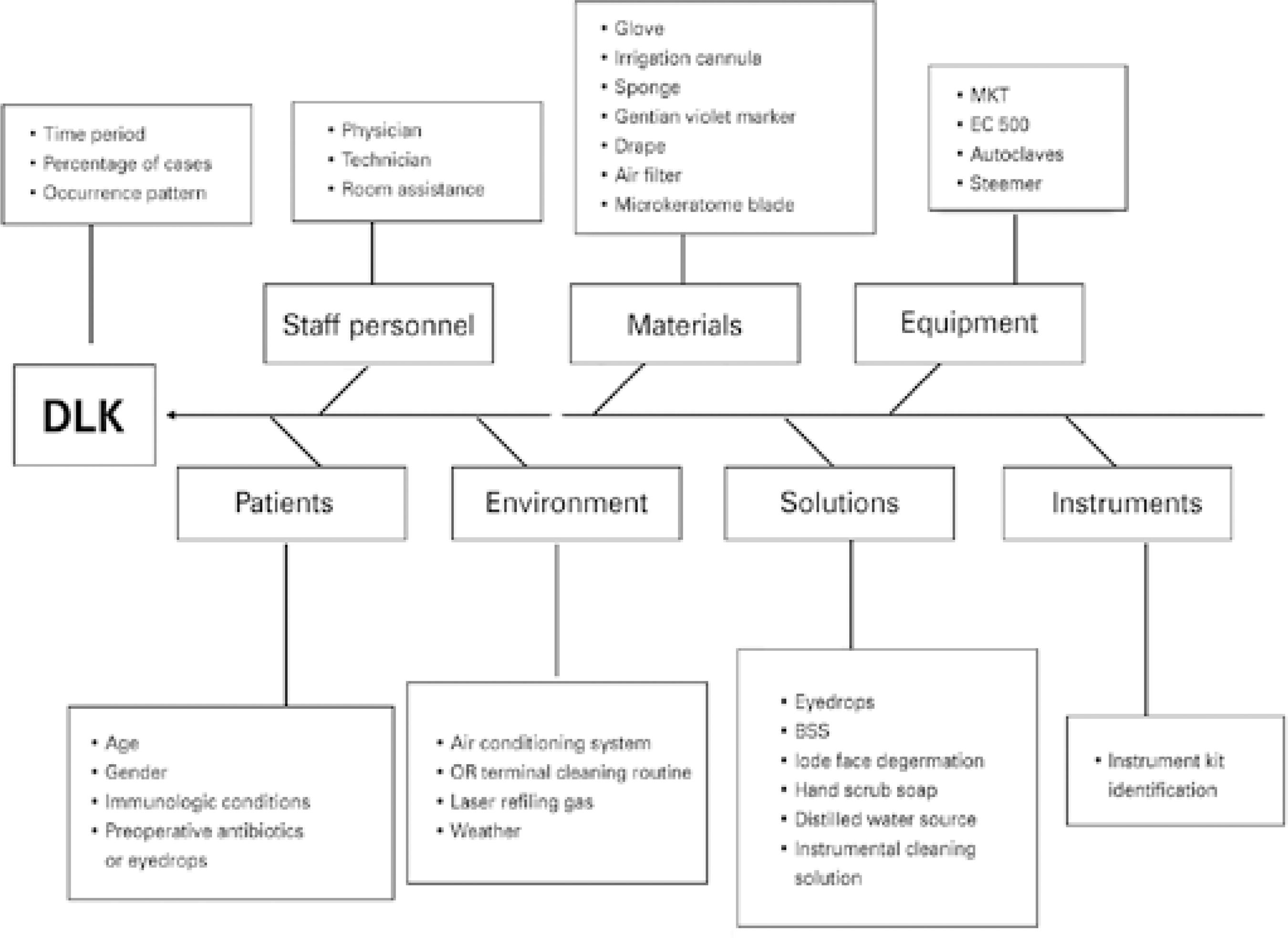
Figure 1 An Ishikawa diagram in which the focus of the analysis was a diffuse lamellar keratitis (DLK) outbreak. All probable causes of the problem are listed according to the major categories that form the spine bones of the “fish
All DLK occurrences dated within a period of 15 days before and 15 days after the first and last cases, respectively, were recorded. The percentage of occurrences among the total number of surgeries and the occurrence pattern were established.
Trials were conducted to establish a relationship between the occurrence of DLK and the physician, technician, or room attendant present in the operating theater. Further, we verified the specific microkeratome machine used, the operating room (OR), and the sequence position in the period during which the surgeries were performed for these cases.
The logistic routine of the surgical asepsis of the patient and medical team was also reviewed. Methodical changes of all materials, medications , and solutions used during the surgical procedure (Figure 1) were carried out under careful observation.
Environmental analysis consisted of examining air, workstation surface, and floor samples of the three ORs, material centers, and hand-scrubbing sites. All specimens were forwarded to a specialized laboratory for analysis. The air conditioner filter and ducts were also cleaned. During the outbreak, 228 different doctors utilized our facilities for surgery; 58 of them had patients with DLK. Finally, an analysis of the air quality and quantification of the particles in the suspension were performed.
A case patient was defined as a patient who developed DLK within 48 h of undergoing a flap-related refractive procedure (i.e., a flap-lift enhancement or myopic or hyperopic LASIK). Cases were ascertained through ophthalmic examination. All individuals who underwent the same procedures on the same dates as the selected cases but did not develop DLK were chosen as controls.
Statistical analysis
The total number of at-risk eyes for developing DLK was used to calculate the proportion of affected eyes. Each individual contributed only one eye in the statistical analysis; for those with both affected eyes, one eye was randomly chosen as a case, and if only one eye was affected, this eye was chosen to be a case. For controls, one eye from each non-affected person was randomly chosen. If only one eye was submitted to surgery during this period, it was chosen as a control.
Chi-square and Fisher’s exact tests were performed to compare categorical variables, and t-tests were used to compare continuous variables. Multivariate analysis was performed with logistic regression to determine the independent effect of risk factors, and confounders and test interactions were controlled for.
Ethics committee approval was obtained from the Research Ethics Committee of Universidade Federal de São Paulo.
RESULTS
Period overview
All 3,698 procedures that were performed during the study period were classified as either “Flap Involving” or “Non-Flap.” A baseline count of the number of surgeries performed during the analysis period was extracted, which spanned from January to June 2007. Of a mean number of 791 procedures per month, 686 (86.7%) involved flaps (68.8%, myopic LASIK; 25.8%, hyperopic LASIK; and 5.5%, flap-lifting enhancements).
The outbreak began on June 13, 2007 and ended on December 21, 2007. During this time, 204 eyes of 141 individuals presented with DLK (12.0%); this was of a total of 1,682 eyes that underwent refractive surgery involving a flap-related procedure.
DLK demographics
Sixty-two patients presented with bilateral DLK (124 eyes; 7.3%). Among these, 118 eyes (59 patients) had the surgeries performed simultaneously, whereas 6 eyes (3 patients) underwent the operation on different days for each eye.
Eighty patients had monocular DLK. Among these, 26 individuals had both eyes operated simultaneously, 23 underwent the operation on different days for each eye, and 31 had only one eye operated.
The number of “flap-involving” procedures gradually dropped over the study period; overall, 78 surgeries were performed in December. July experienced a peak in the incidence of DLK cases, and in absolute numbers, there were 74 cases in total in this month (16%). However, during the relative analysis, it was determined that the incidence of DLK cases peaked in September, during which, 25 cases (18%) of the 140 flap-involving surgeries presented with DLK (Graph 1).
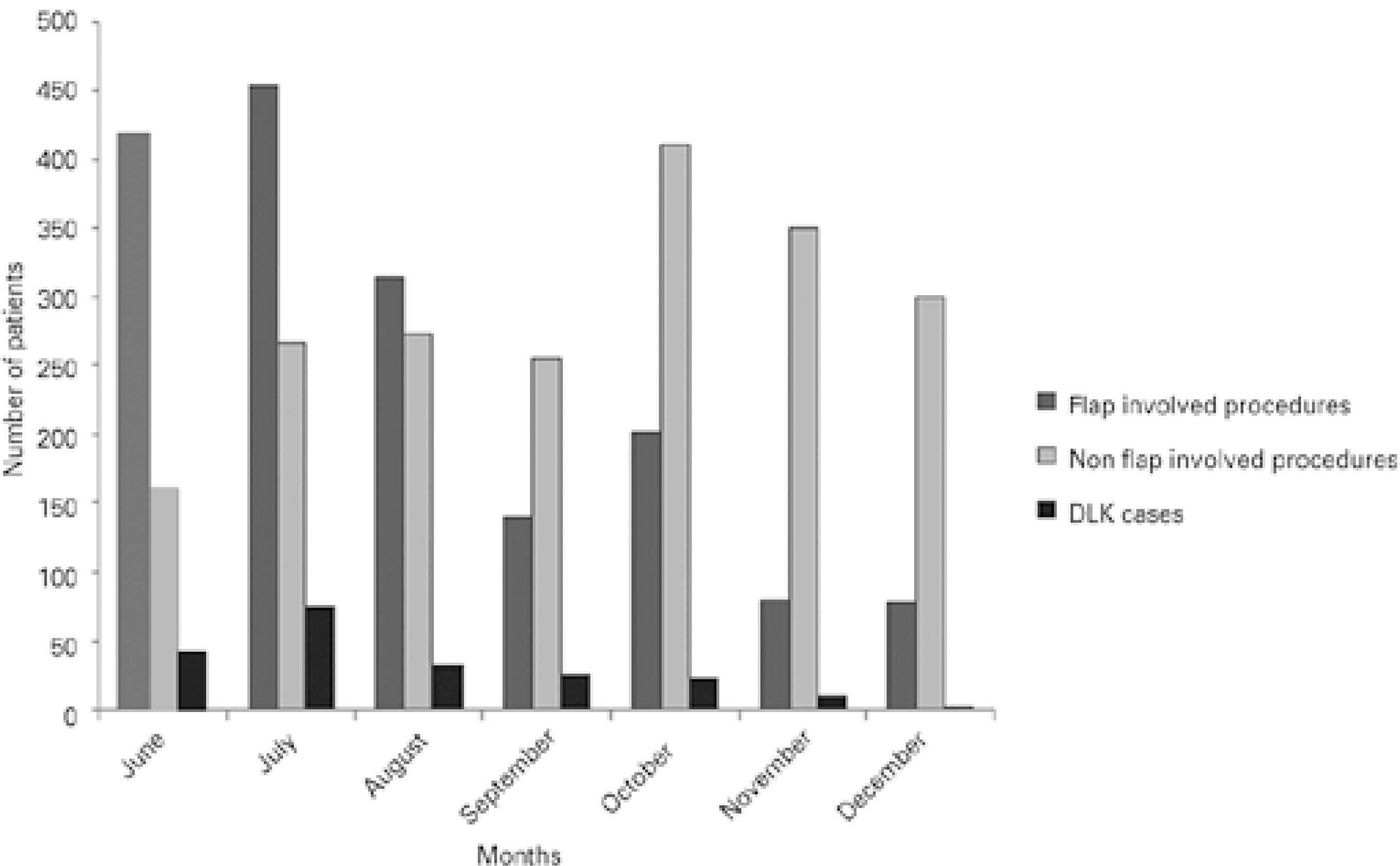
Graph 1 Note the decrease in the number of “flap-involving” procedures over the period of the outbreak, which is in stark contrast to the increase in the numbers of surface treatments that were performed from June to December 2007. Although, in terms of absolute numbers, July showed a peak in the incidence of diffuse lamellar keratitis (DLK), with 74 cases, September yielded the greatest percentage of DLK cases, with 25 cases (18%) of the 140 performed surgeries developing DLK. In the graph, the dark gray columns represent “flap-involving” procedures, the light gray columns represent “non-flap” procedures, and the black columns represent DLK cases
The patients’ mean age was not statistically different between positive and negative cases for DLK (p=0.36). A slightly higher proportion of males was observed among the cases (p=0.23). Most surgeries were performed during the evening, and myopic LASIK was the most frequently performed surgery.
Of a total of 1,142 myopic LASIK procedures, DLK occurred in 144 eyes (12%), and of a total of 414 hyperopic LASIK procedures, 31 eyes presented with DLK (7%). Finally, among the 128 flap-lift enhancements, 29 eyes (22%) developed DLK. In one case, DLK occurred in an incomplete keratomileusis, which led to the cessation of laser ablation. No significant difference in the rate of DLK was observed between these two procedures (p=0.06). Moreover, flap-lift enhancements were strongly related to DLK occurrence (p=0.01). Table 1 shows the results of the multivariate analysis.
Table 1 Odds ratios and 95% confidence intervals of the associations between risk factors and the development of diffuse lamellar keratitis (DLK)
| Risk factors | Yes (n=141) | No (n=789) | P-value |
|---|---|---|---|
| Age (years) | 34.29 ± 10.6 | 35.23 ± 11.6 | 0.360 |
| Sex, male (%) | 45.6 | 40.1 | 0.230 |
| Period | 0.170 | ||
| Morning | 39.7 | 31.7 | |
| Afternoon | 15.6 | 16.6 | |
| Evening | 44.7 | 51.7 | |
| Procedures | 0.002 | ||
| Enhancements | 16.3 | 09.0 | |
| Myopic LASIK | 68.8 | 64.8 | |
| Hyperopic LASIK | 14.9 | 26.2 | |
| Microkeratome | 0.007 | ||
| Hansatome | 72.4 | 81.1 | |
| Nidek | 11.3 | 10.8 | |
| Flap lifts | 16.3 | 08.1 | |
| Anesthetics | 0.110 | ||
| Anestalcon | 78.0 | 67.4 | |
| Oxinest | 18.4 | 26.5 | |
| Others | 03.6 | 02.4 | |
| Hand scrub solution | 0.050 | ||
| Clorexidine | 75.9 | 67.4 | |
| Dr. Clean | 24.1 | 32.6 | |
| 0.110 | |||
| None | 13.5 | 09.8 | |
| Supermax | 24.1 | 19.4 | |
| Polimax | 62.4 | 70.8 | |
| Facial cleaning | 0.020 | ||
| PVPI | 21.3 | 30.2 | |
| Water and soap | 23.4 | 27.2 | |
| Cetrimide | 55.3 | 42.2 | |
| Drape | 0.270 | ||
| 70101 SN | 41.1 | 42.2 | |
| 70201 SN | 26.9 | 21.5 | |
| Inda 157 | 12.8 | 10.9 | |
| Others | 19.2 | 25.4 | |
| Corneal marker | 0.018 | ||
| Yes | 93.6 | 86.5 | |
| Sponge | 0.060 | ||
| Merocel | 49.6 | 63.7 | |
| Excel | 41.8 | 30.1 | |
| Meroalcon | 08.6 | 06.2 | |
| Alcohol rinsing of instruments | 0.300 | ||
| Yes | 30.5 | 26.2 | |
| Tube air filter | 0.034 | ||
| Yes | 82.3 | 73.8 | |
| Water source for hand scrubbing | 0.080 | ||
| Tap | 19.9 | 28.5 | |
| Filtered | 49.6 | 45.9 | |
| Mineral | 30.5 | 24.6 | |
| Premix gas | 0.060 | ||
| Original | 82.9 | 75.7 | |
| Other suppliers | 17.1 | 24.3 | |
| Therapeutic contact lenses | 0.004 | ||
| Yes | 06.4 | 15.2 | |
Data are presented as the mean ± standard deviation or percentage.
Eyes that received flap-lift enhancement were approximately three times more likely to develop DLK than eyes that underwent hyperopic LASIK (p=0.001), after adjusting for several confounders [odds ratio (OR): 3.09 (95% confidence interval (CI): 1.58-6.06)].
Individuals who underwent surgery during the morning shift had a 50% greater chance of developing DLK than those who underwent surgery in the evening [OR:1.51 (95% CI: 1.00-2.27)]. The use of contact lenses in the postoperative period diminished the chance of DLK development by 65% [OR: 0.35 (95% CI: 0.14-0.85)] after controlling for confounders. Furthermore, the incidence of DLK was not related to the expertise of the professional who performed the LASIK procedure.
None of the seven Hansatome microkeratomes or the Nidek MK2000 systems contributed to the occurrence of DLK. Similarly, glove use or glove brand, gentian violet corneal markers, hand-scrubbing products, surgical instrument cleaning solutions, facial cleaning solutions, sponge brands, water sources, biofilms in autoclave water reservoirs, intraoperative medications, and solutions did not seem to be related to DLK occurrence.
The fact that there were new occurrences of DLK, irrespective of the systematic and routine changes in the performed surgeries, suggested that there was no relationship between the development of DLK and any of the primary factors, including equipment, materials, instruments, medications, solutions, staff personnel, and environment.
DISCUSSION
The use of the Ishikawa diagram provided a clear view of the entire surgical logistics and facilitated even more rigid management of the main factors involved in the process and, thus, highlighted factors that deserved attention.
These processes included air drying the surgical instruments and the autoclave reservoirs at the end of each surgical day, rigorously cleaning or discarding all materials in a controlled manner, performing medicine contamination checkups, mindfully introducing any new brands of materials, engaging in environmental control, ensuring patient and staff asepsis, and performing proper sterilization of the surgical instruments and equipment.
The rate of DLK after microkeratome LASIK flap creation has been estimated to be 0.4-7.7%(13,14). In comparison, the rate of DLK after femtosecond LASIK flap creation ranges from 0.4% to 19.4%(15,16). There is increasing interest in understanding this phenomenon. Studies have shown that high laser energy levels and the ensuing photodisruption-induced tissue injury and accumulation of gas bubbles can lead to an increased inflammatory response and DLK(17-19).
Different elements have been attributed as the trigger for inflammation in DLK, including surgical glove powder and silicon; Sphingomonas paucimobilis/Burkholderia pickettii endotoxins; gonococcal keratoconjunctivitis; toxic chemicals; ophthalmic sponges; recurrent epithelial erosion; cleaning solutions(20); trauma; uveitis; and iritis.
Histological and confocal microscopy findings of the cells recovered from interface scrapings in DLK have shown the presence of lymphocytes, eosinophils, and neutrophils(21). Degenerated cells have also been observed as the inflammatory process progresses. The immunological response during the inflammatory process involves interleukin-8, which may be found in the stromal keratocytes and infiltrating neutrophils(22), thus endorsing the theory that an immune-mediated inflammatory mechanism is involved.
Differential diagnoses of DLK include epithelial ingrowth at the interface, infectious infiltrates, sponge residues, tear film debris, and central toxic keratopathy.
No major consequences are typically seen in the corneas following the resolution of DLK. Neither corneal irregularities nor induced refractive errors are commonly observed; as such, the late resolution results are predictable(9). However, complications associated with untreated and naturally progressing DLK include corneal melting and tissue consumption. Further, a hyperopic shift in the final refraction of eyes after severe DLK has been previously reported(23).
Following the present analysis, the authors concluded that flap-lift enhancement procedures, procedures performed during the morning shift, and discontinuing the use of therapeutic contact lenses immediately after the surgery are highly related to DLK occurrence. Interestingly, commonly suspected factors such as glove powder, ophthalmic sponges, corneal marker pens, cleaning solutions, biofilms in autoclave water reservoirs, and air-conditioning filters, as well as microkeratome engine oil leaks, were not found to be possible causes of the DLK outbreak.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

