INTRODUCTION
Bariatric surgery is an increasingly common treatment for morbid obesity, which is defined as body mass index (BMI) >40 or ≥35 kg/m2 when associated with comorbidities such as arterial hypertension, dyslipidemia, sleep apnea or diabetes1. Patients requesting bariatric surgery undergo a rigorous selection procedure, with a minimum of 5 years between the onset of obesity and the established failure of conventional multidisciplinary treatment including diet, pharmaceutical therapy, and regular physical exercise2. Surgical treatment of obesity includes both malabsorptive and restrictive bariatric techniques. Most currently used procedures combine both techniques, with vertical banded gastroplasty-Roux-en-Y gastric bypass, the Capella technique, being the most frequently performed. This procedure results in a mean 35% loss of body mass over the long term and is considered a safe technique with a low morbidity rate2.
Many obese individuals have low levels of vitamin B6, vitamin C, 25-hydroxyvitamin D, and vitamin E prior to bariatric surgery. As bariatric surgery results in anatomical and physiological changes in the digestive tract, patients become more prone to developing severe vitamin and mineral deficiencies3. Nutritional deficiencies following bariatric surgery occur because of the restricted diet, reduction in bowel transit time, and reduction in the surface area available to absorb nutrients. Food intolerance and a lack of vitamin supplementation further contribute to this process4. Deficiencies of lipid soluble vitamins, that is, A, D, E, and K, develop following the surgical procedure because of reduced production of gastric and pancreatic lipases resulting from the absence of contact of the duodenum with dietary fat and the detrimental effect of the surgical procedure on cholecystokinin, which is essential for the release of the enzymes involved in lipolysis5.
Vitamin A is an essential lipid soluble vitamin acquired in the diet and is responsible for both homeostasis of the ocular surface and the retina's adaptation to light1,6. The incidence of vitamin A deficiency following bariatric surgery has been estimated at around 52% at 1 year and 69% at 4 years after biliopancreatic diversion with a duodenal switch technique. The incidence of related ocular complications included an estimated 10% rate of xerophthalmia and night blindness. Other investigators have reported a reduction of only 10% in vitamin A level, with variations depending on the surgical technique used4,7,8. All types of surgery, including gastric reduction and gastric bypass, are associated to a greater or lesser extent with vitamin A deficiency and potentially capable of damaging the ocular surface through quantitative and qualitative alterations of the tear film7,9. The tear film helps maintain the homeostasis of the ocular surface by supplying oxygen to the cornea and conjunctiva, promoting cell renewal, removing products of cell metabolism and microorganisms, in addition to regulating the refractive properties of the corneal epithelium10. Xerophthalmia, squamous metaplasia of the conjunctiva, anatomical and functional alterations of the corneal epithelium, ocular thinning and perforations are potential consequences of vitamin A deficiency and ocular dryness7,9.
A diagnosis of dry eyes is based on the patient's clinical history, dry eye-specific questions, and clinical tests such as evaluating tear-film breakup time (BUT), Schirmer's test, tear ferning test, ocular surface staining with vital dyes such as rose Bengal and fluorescein, conjunctival impression cytology, and others11. Other tests used to diagnose dry eyes, such as tear film osmolarity, measurement of the protein levels in the film, tear interferometry, and tear evaporation, are of little use in daily practice, as they are costly and impractical12. Few randomized studies of the association of alterations of the ocular surface and bariatric surgery have been published. The study objective was to analyze the results of tests to evaluate the ocular surface and to identify correlations of the presence and intensity of ocular alterations with bariatric surgery.
METHODS
This cross-sectional, analytical, observational, blinded study was conducted between November 2012 and April 2015 following approval by the internal review board, reference CAAE 06275212.6.0000.54799. Patients were recruited at the bariatric surgery outpatient clinic, Department of Surgery, and the Ocular Surface and Tear outpatient clinic, Department of Ophthalmology, Irmandade da Santa Casa de Misericórdia de São Paulo, São Paulo, Brazil.
Inclusion criteria
Postoperative groups
Eligible patients were adults with bariatric surgery using the Capella technique. The patients had not used contact lenses for at least 7 days prior to evaluation and voluntarily signed the informed consent form provided by the investigators.
Preoperative group
The preoperative patient group comprised obese adults with a BMI >40 or ≥35 kg/m2 with systemic complications such as arterial hypertension, diabetes, sleep apnea and dyslipidemia. As in the postoperative groups, patients had not used contact lenses for at least 7 days prior to evaluation and had voluntarily signed the informed consent form provided by the investigators.
Exclusion criteria
In both preoperative and postoperative groups, patients with previously diagnosed eye diseases; currently using, or had used medications capable of affecting tear production and drainage within 7 days of evaluation, >60 years of age, and pregnant or breastfeeding women were excluded.
Test sequence
The patients in both preoperative and postoperative groups who fulfilled all the inclusion criteria and with none of the exclusion criteria were evaluated at the Ocular Surface and Tear outpatient clinic of the hospital's Department of Ophthalmology, always in the same order and always by the same investigator (NPNM). Postoperative patients were stratified by the time that had elapsed since surgery to groups of 0-12 or >12 months and ≤5 years. All the patients were evaluated by tests given in the following sequence.
Dry eye-specific questionnaire
The survey included questions about dry eye symptoms included in the Ocular Surface Disease Index (OSDI; Allergan Inc., Irvine, CA)13. This questionnaire was translated and validated for the Portuguese language and consists of 12 questions, answered by the participants, on events that occurred in the previous 7 days. The questions address ocular symptoms, environmental stimuli that caused eye discomfort, and limitation of daily activities because of clinical eye conditions. The overall score ranged from 0 to 100 and was calculated from the score each response and the total number of questions answered. Higher scores indicated more dry eye-related symptoms14.
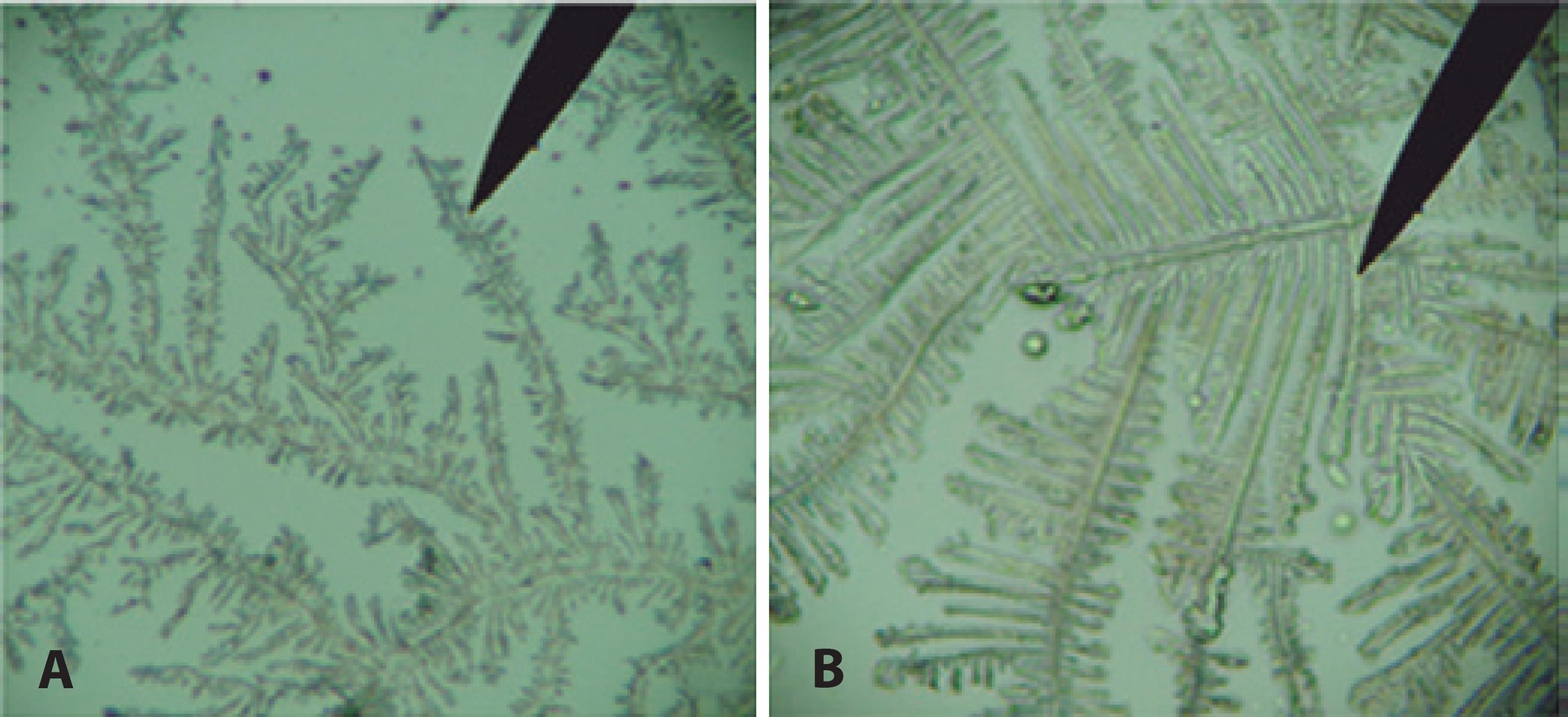
Tear ferning test
In this qualitative tear film evaluation, patients were placed in the same position that is used for slit-lamp evaluation, and varying amounts of tear fluid were collected from the lower tear meniscus of both eyes using a non-heparinized glass capillary tube (Shanghai Allcan Medical Co, China). A blue pen was used to mark six circles on a clean glass slide (Microscope slides, ground edges, 25.4 × 76.2 mm × 1-1.2 mm), three on the upper part of the slide and three on the lower part, corresponding to the right and left eye, respectively. A teardrop was deposited in each circle and then dried at room temperature for around 10 min before being stored in an appropriate box for transportation. The slides were examined by light microscopy and the dry tear spots were photographed (Sony Cybershot model DSC-W630) at ×10, ×20, and ×40 magnification. The photographs were independently examined by blinded investigators as previously described by Rolando15. The tear samples were classified into one of the four types by the quantity and angulation of the crystals. Types I and II indicated absence of ocular surface disease; types III and IV reflect ocular surface abnormalities (Figure 1 A and B).
Tear film BUT
This was performed immediately following the previous test. One drop of 1% sodium fluorescein (Allergan® São Paulo, Brazil) was applied to the lower tear meniscus of both eyes. The patients were asked to blink a few times and stop when requested. A chronometer was then started and the time until appearance of the first spot of tear film break-up on the surface of the cornea was observed. Three measurements were taken in each eye and the mean value was recorded. A tear film BUT >10 sec= was considered normal.
Schirmer's test I
About 10 min after the previous test, patients were evaluated with Schirmer's test I, also referred to as Schirmer's test without anesthesia. The test was performed simultaneously in both eyes by placing a standard millimeter strip of Whitman No. 41 filter paper (Ophthalmos®, São Paulo, Brazil) into the lateral third of each of the lower eyelids. Patients were instructed to keep their eyes closed for 5 min, the amount of moisture visible on the paper from each eye was mea su red immediately. This value can range from 0 to 35 mm, with >10 mm being considered normal.
Evaluation of the ocular surface by 1% rose Bengal staining
Immediately after performing the Schirmer's test, the ocular surface was evaluated for damage by 1% rose Bengal staining (Ophthalmos®, São Paulo, Brazil). Three microdrops were placed in the upper bulbar conjunctiva of each eye with the aid of a plastic capillary tube. Then a slit lamp with illumination and a green filter was used to estimate the dye taken up by dead and degenerating cells. The eyes were scored using a method previously described by van Bijsterveld16, to quantify damage to the ocular surface. Scores ranged from 0 to 9, with 0 indicating no damage and 9 the most severe damage. The interpalpebral zone was divided into the nasal bulbar conjunctiva, temporal bulbar conjunctiva, and cornea. The staining intensity was quantified as varying from 1° to 3° with 0.5° intervals within each region. If the sum of intensity scores for the three regions in at least one of the eyes was ≥3.5, then it was considered positive for dry eye.
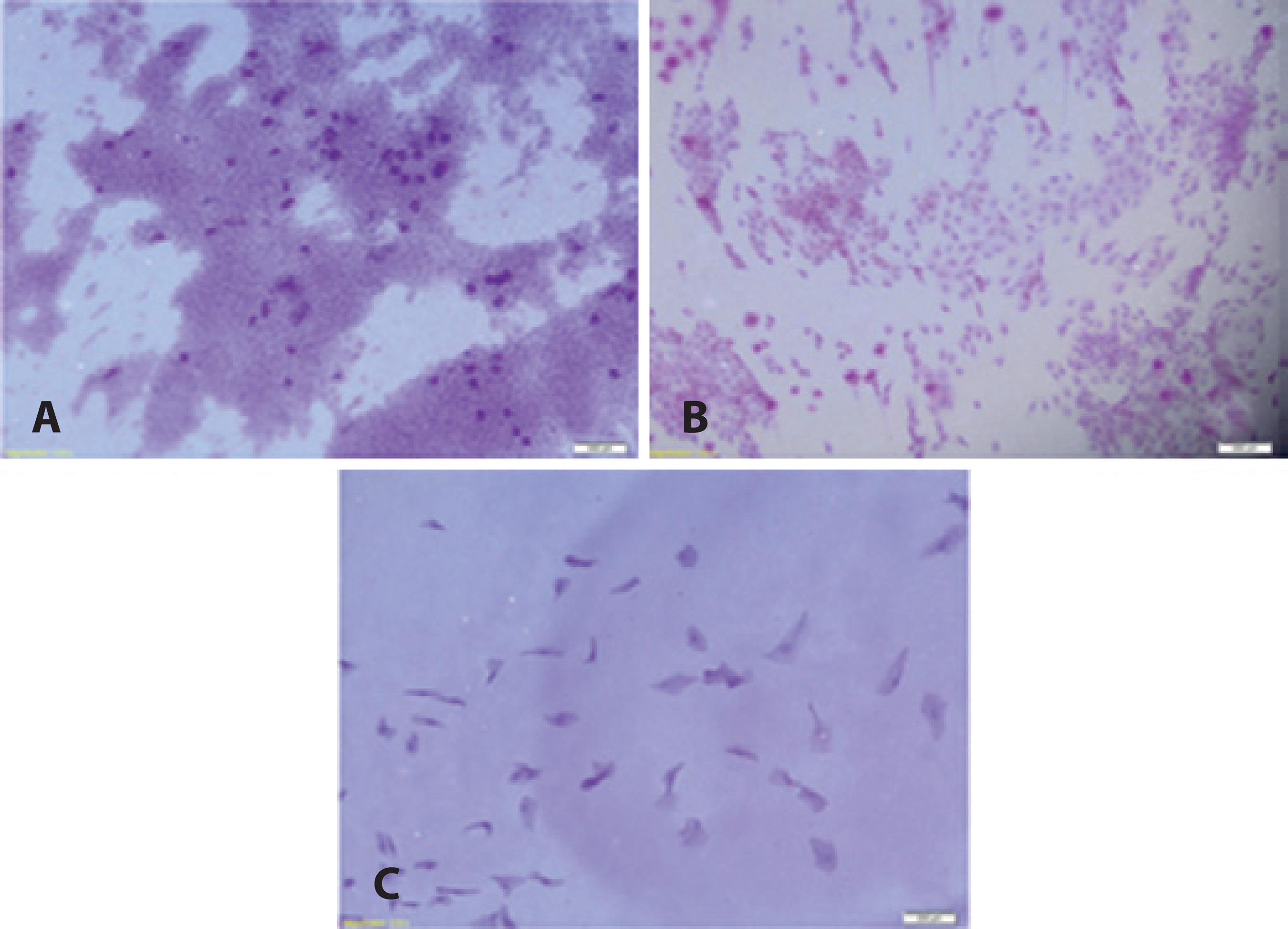
Impression cytology
Immediately following on the previous test, and after applying topical anesthetic, a small piece of Millipore filter paper measuring approximately 5 × 7 mm was used, with a different shape for each of the areas evaluated, a square end for the upper region and a tapered end for the temporal region. The paper was pressed against the bulbar conjunctiva in the upper and lateral quadrants of the right eye for 2-5 sec using blunt smooth-ended forceps. The filter paper was then removed and placed in a screw-topped test tubes marked with the patient's identifying number and containing a small quantity of fixative sufficient to cover the filter paper. The fixative was prepared in advance by combining 100 cc 70% ethanol, 5 cc of glacial acetic acid, and 5 cc of 37% formaldehyde. For staining, the paper was removed with tweezers and placed in a well of a tissue culture plate. Staining was analyzed by a blinded investigator11. The preparations were assessed for cellularity, cell adhesion, the presence of goblet cells, nucleus-to-cytoplasm ratio, and cell keratinization. Samples (Figures 2 A-2 C) were graded as type 1-normal (0-3), type B-moderate (4-6), or type C-abnormal (>6).
Vitamin A supplementation
Patients were questioned about compliance with nutritional supplements and graded as 1(always forget), 2 (never forget), or 3 (sometimes forget).
Statistical analysis
Statistical analysis was conducted using SPSS statistical software, version 13.0. Patient age and BMI were reported as means and standard deviation and medians and range and compared by analysis of variance (ANOVA)17. The sex distribution was reported by absolute and relative frequency18. Mean OSDI scores, mean tear film BUT, Schirmer, and rose Bengal scores were reported by group means and standard deviation and medians and range and compared by ANOVA or the Kruskall-Wallis test, as appropriate. Impression cytology and tear ferning were reported by absolute and relative frequencies and compared using the chi-square test18. Results were shown for each group using tables and bar graphs. The tests were conducted with a significance level of 5%.
RESULTS
The study included 89 participants. Eighty-one (91.0%) were women. There were more women than men in each study group, but the percentage of women was slightly lower in the preoperative than the postoperative groups. Thirty-five patients (39.3%) had not yet undergone surgery, 32 (36.0%) had undergone surgery within the previous 12 months, and 22 (24.7%) had undergone surgery between 12 months and 5 years previously. As shown in table 1, there were no statistically significant differences in mean age among the groups (p=0.082), but BMI was significantly different (p<0.001). The mean BMI of the postoperative patients was significantly lower than that of the preoperative patients (p<0.05).
Table 1 Bariatric surgery patient characteristics and study groups
| Variable | Group | Mean | Median | SD | Range | p-value |
|---|---|---|---|---|---|---|
| Age | Preoperative | 41.3 | 44.0 | 9.3 | 25.0-58.0 | <0.082 |
| 1-12 months after surgery | 43.4 | 42.5 | 8.1 | 31.0-60.0 | ||
| >12 months after surgery | 46.5 | 48.0 | 7.3 | 36.0-58.0 | ||
| BMI | Preoperative | 47.7 | 48.1 | 7.2 | 29.9-64.7 | <0.001 |
| 1-12 months after surgery | 36.7 | 37.2 | 7.8 | 26.5-60.4 | ||
| >12 months after surgery | 31.8 | 31.1 | 7.8 | 14.3-46.8 |
BMI= body mass index; SD= standard deviation.
As shown in table 2, all test values were within the normal range, and there was no significant difference in OSDI scores observed in the preoperative and postoperative periods. It was noted that the mean tear film BUT was consistently lower than normal (10 sec), with no significant differences between the groups. As indicated in tables 3 and 4, the Schirmer's test and rose Bengal staining scores results showed a trend toward improvement of the ocular surface following surgery, but the differences were not statistically significant. Despite the variations found in ferning and impression cytology, there was no evidence of any significant differences between the groups,. Compliance with nutritional supplementation was poor; 73% of postoperative patients forgot, on average 2-3 times a week, and 92% of obese patients neglected, to use vitamin supplements.
Table 2 Test assessment scales and comparative results observed in the study groups
| Variable | Group | Mean | Median | SD | Range | p-value |
|---|---|---|---|---|---|---|
| OSDI | Preoperative | 34.8 | 33.1 | 24.3 | 2.1-100.0 | P=0.139 |
| 1-12 months after surgery | 29.8 | 26.3 | 22.7 | 0.2-91.7 | ||
| >12 months after surgery | 43.1 | 46.9 | 24.7 | 0.8-93.2 | ||
| BUT/right eye | Preoperative | 09.7 | 8.0 | 04.9 | 3.0-23.0 | P=0.684 |
| 1-12 months after surgery | 08.7 | 7.0 | 04.9 | 2.0-20.0 | ||
| >12 months after surgery | 09.5 | 9.0 | 05.1 | 0.0-19.0 | ||
| BUT/left eye | Preoperative | 10.9 | 9.0 | 06.3 | 4.0-33.0 | P=0.531 |
| 1-12 months after surgery | 09.7 | 8.0 | 04.7 | 4.0-19.0 | ||
| >12 months after surgery | 11.6 | 10.0 | 08.2 | 2.0-44.0 | ||
| Schirmer/right eye | Preoperative | 17.4 | 15.0 | 11.3 | 0.0-35.0 | P=0.478 |
| 1-12 months after surgery | 20.7 | 19.0 | 10.6 | 2.0-35.0 | ||
| > 12 months after surgery | 19.8 | 18.5 | 13.6 | 2.0-35.0 | ||
| Schirmer/left eye | Preoperative | 15.2 | 12.0 | 11.2 | 0.0-35.0 | P=0.097 |
| 1-12 months after surgery | 21.1 | 23.0 | 11.1 | 2.0-35.0 | ||
| >12 months after surgery | 18.8 | 19.0 | 11.4 | 4.0-35.0 | ||
| Rose Bengal/right eye | Preoperative | 01.9 | 02.0 | 01.4 | 0.0-5.0 | P=0.461 |
| 1-12 months after surgery | 01.8 | 01.5 | 01.5 | 0.0-6.0 | ||
| > 12 months after surgery | 01.5 | 01.0 | 01.5 | 0.0-5.0 | ||
| Rose Bengal/left eye | Preoperative | 01.7 | 01.0 | 01.6 | 0.0-6.0 | P=0.421 |
| 1-12 months after surgery | 01.6 | 01.0 | 01.3 | 0.0-5.0 | ||
| >12 months after surgery | 01.1 | 01.0 | 01.0 | 0.0-3.0 |
OSDI= ocular surface disease index; BUT= tear-film break-up time; SD= standard deviation.
Table 3 Tear ferning test results by study group
| Variable | Group | Number of patients normal | Number of patients altered |
|---|---|---|---|
| Tear ferning test right eye | Preoperative | 19 | 12 |
| 1-12 months after surgery | 22 | 08 | |
| >12 months after surgery | 12 | 08 | |
| Tear ferning test left eye | Preoperative | 18 | 13 |
| 1-12 months after surgery | 20 | 10 | |
| >12 months after surgery | 12 | 08 |
Table 4 Impression cytology of the upper and lateral conjunctiva by study group
| Number of patients | ||||
|---|---|---|---|---|
| Variable | Group | 0-3 | 4-6 | >6 |
| Impression cytology of upper conjunctiva | Preoperative | 24 | 2 | >0 |
| 1-12 months after surgery | 21 | 3 | >0 | |
| >12 months after surgery | 17 | 0 | >0 | |
| Impression cytology of lateral conjunctiva | Preoperative | 16 | 7 | >2 |
| 1-12 months after surgery | 13 | 6 | >3 | |
| >12 months after surgery | 14 | 1 | >0 | |
DISCUSSION
There were more women than men in all three study groups. Overall, 91.0% of the participants were women, which is in agreement with previous epidemiological studies showing a predominance of women requesting or being evaluated for obesity surgery. The percentage of men in the preoperative group was larger than that in the postoperative groups. BMI decreased progressively with the time since surgery from an initial median of 48.1 kg/m2 in the preoperative group to 31.1 kg/m2 in patients whose surgery had taken place more than 12 months previously. Despite the significant decrease in BMI, four patients (20%) remained obese, with BMIs >35 kg/m2. Slater et al.19 reported similar results, with a median BMI that decreased from 49.28 kg/m2 prior to surgery to 32.4 kg/m2 after surgery despite 27.3% of the patients with a postsurgery BMI >35 kg/m2. The absence of observed ocular surface changes can be explained by the presence of a large proportion of patients undergoing bariatric surgery who remained obese.
Vitamin A deficiency is a known consequence of Roux-en-Y gastric bypass, occurring in 11% of cases20. All patients in this study underwent Roux-en-Y gastric bypass, which is the most frequently used technique in both the United States and in Brazil. Additional study is needed to assess the role of routine vitamin A screening and replacement in the postbariatric surgery patient. In our institution, patients in the Department of Surgery receive vitamin replacement therapy on an irregular basis, and a high rate of noncompliance with use of nutritional supplement was observed. Considering patient food restriction, reduced gastrointestinal transit time, and decreased nutrient absorption, all of which are consequences of bariatric surgery, multivitamin use is essential. Patient education on compliance with nutritional supplements is essential after bariatric surgery21.
Cheung et al.22 emphasized the importance of investigating the association between bariatric surgery and xerophthalmia in view of a possible increase in risk of iatrogenic damage to the eyes in parallel to an increase in the number of bariatric surgeries performed. Several case reports1,6,21 have described changes in ocular health following obesity surgery. Donaldson et al.21 reported a patient who underwent bariatric surgery and was diagnosed 10 years later with corneal melt after laser in situ keratomileusis. At that time, the patient's vitamin A level was low, and he admitted noncompliance with nutritional supplements. Systemic or ocular factors other than bariatric surgery can cause xeropthalmia, but were excluded in that report. Ocular hyperemia and complaints of a foreign body sensation were reported in this study, but the com p laints following surgery did not differ among the obese patients, as reflected in the answers to the OSDI questionnaire. Previous studies report improvement in quality of life following bariatric surgery9. In other studies, ophthalmological examinations have shown conjunctival xerosis, Bitot's spots and diffuse punctate keratitis in bariatric surgery patients, but symptoms improved following intramuscular vitamin A supplementation (10,000 IU)1,6. In this study, no changes were found in the ocular surface of any patients following bariatric surgery, which is in line with a recent study that found no correlation between serum vitamin A, visual function, and ocular surface changes23. Previous investigators have reported reductions in vitamin A level after bariatric surgery, with differences depending on the surgical technique used. In this study, the roux-en-Y procedure was performed in all patients. This bariatric surgery technique may cause less reduction in vitamin A level than other procedures. Standard Roux-en-Y gastric bypass is known to cause vitamin B12, iron and folate deficiencies more often than some other procedures8.
In this patient series, there were no changes in tear film BUT, Schirmer's test, rose Bengal staining, tear ferning, or impression cytology, all of which are tests of the utmost importance when a diagnosis of dry eyes is suspected11,24,25. Although the mean tear film BUT score was below the value considered normal both prior to and following surgery, no changes were found in the ocular surface, as rose Bengal staining and impression cytology scores were normal. The preservation of ocular health following surgery can be demonstrated by the absence of quantitative or qualitative changes in tears, as shown by both Schirmer's test and the ferning test. The current study would be more conclusive if it were a longitudinal study and if vitamin A level had been measured. Additional study is needed to assess the role of routine vitamin A screening, and longer follow-up is required to conduct a complete investigation.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

