INTRODUCTION
The lacrimal sac is a structure covered with columnar epithelium located between the anterior and posterior lacrimal crests. It forms the widest portion of the lacrimal duct and usually measures 4-8 mm anteroposteriorly and 10-12 mm vertically(1).
Chronic dacryocystitis is an infection of the lacrimal sac typically associated with nasolacrimal duct obstruction, for which the most commonly described agents are Staphylococcus (S. Aureus and S. epi dermidis) and Streptococcus pneumoniae(2). Chronic dacryocystitis primarily affects women in their third decade of life(3).
The radiological diagnostic method that uses contrast to assess the lacrimal drainage system called dacryocystography, and it is considered the gold standard for evaluating lacrimal system patency(1) and was introduced by Ewing in 1909 (apud Campbell, 1964)(4).
Ultrasonography is an imaging method capable of detecting changes in the lacrimal sac painlessly and noninvasively(5). The method can be used in preoperative evaluation to determine the size and characteristics of the lacrimal sac and for detecting abnormal dilatation, the presence of diverticula, and exudative inflammatory processes(6,7).
B-mode ultrasound imaging is a useful diagnostic method for examining the lacrimal sac in direct contact with the eye nasal canthus region, and the immersion or transocular technique is also able to yield images of the lacrimal sac(8).
The aim of the present study was to categorize the ultrasound findings of the lacrimal sac in subjects with a normal lacrimal system and in those with chronic dacryocystitis.
METHODS
This was a retrospective nonrandomized case-control study that was conducted after approval was granted by the Uni ver sidade Federal de São Paulo Ethics Committee (number 26894514. 6.0000.5505).
Twenty individuals, 10 with a normal lacrimal system (Group 1) and 10 diagnosed with chronic dacryocystitis (Group 2), were included in this study at the Federal University of São Paulo (UNIFESP). Group 1 included patients with normal lacrimal system function. Group 2 included 10 cases with chronic dacryocystitis diagnosed by the presence of tear expression test and the fluorescein dye disappea rance test (Milder test), with seven cases also presenting obstruction of the nasolacrimal duct as assessed by dacryocystography. Exclusion criteria were previous trauma, fistula, patients aged <20 years, and previous surgery of the lacrimal system.
All individuals were evaluated in the supine position 5 min after instillation of one drop of proxymetacaine hydrochloride 0.5% (Anestalcon®; Alcon, Hünenberg, Switzerland) in the conjunctival fornix of the eye to be examined.
All ultrasonography was performed by the same examiner (NA)with a 10-MHz transducer (Aviso; Quantel Medical, Cournon-d'Au vergne, France) placed directly on the skin of the lacrimal fossa (di rect-contact technique) using a conductive gel (Figure 1). Evalua tion of the lacrimal sac was performed using B-mode ultrasound and included anteroposterior and vertical scans, with qualitative assessment of the content. The left eye of each participant in Group 1 was evaluated.

Figure 1 Position of an individual with left chronic dacryocystitis during ultrasound examination of the lacrimal sac, with a 10-MHz transducer pla ced directly on the skin of the left lacrimal fossa, using a conductive gel.
For statistical analysis, quantitative variables such as the anteroposterior and vertical dimensions of the lacrimal sac were tested using Levene's test. We considered p<0.005 as statistically significant.
RESULTS
In Group 1, 10 individuals with a normal lacrimal system, including six women and with a mean age of 48.4 years (SD=19.9 range, 22-80 years), were evaluated using B-mode ultrasound (Table 1).
Table 1 Characteristics of the study population with a normal lacrimal sac as assessed by 10-MHz ultrasound
| Case | Age (years) | Laterality | Dimensions of the lacrimal sac | Content | |
|---|---|---|---|---|---|
| Anteroposterior (mm) | Vertical (mm) | ||||
| 1 | 80.0 | L | 1.67 | 10.55 | Clear |
| 2 | 22.0 | L | 2.81 | 11.47 | Clear |
| 3 | 25.0 | L | 2.13 | 12.42 | Clear |
| 4 | 45.0 | L | 1.45 | 8.37 | Clear |
| 5 | 47.0 | L | 1.92 | 6.59 | Clear |
| 6 | 49.0 | L | 1.31 | 7.80 | Clear |
| 7 | 71.0 | L | 1.77 | 9.76 | Clear |
| 8 | 54.0 | L | 1.54 | 9.44 | Clear |
| 9 | 65.0 | L | 1.73 | 10.28 | Clear |
| 10 | 26.0 | L | 2.27 | 11.26 | Clear |
| Mean | 48.4 | 1.86 | 9.79 | ||
L= left.
In Group 2, 10 patients with a total of 10 eyes affected by chronic dacryocystitis, including eight women and with a mean age of 50.7 years (SD=15.5; range, 25-75 years), were examined with B-mode ultrasound (Table 2).
Table 2 Characteristics of the study population with chronic dacryocystitis as assessed by 10-MHz ultrasound
| Case | Age (years) | Laterality | Dimensions of the lacrimal Sac | Content | |
|---|---|---|---|---|---|
| Anteroposterior (mm) | Vertical (mm) | ||||
| 1 | 50.0 | R | 5.13 | 10.82 | Punctate, partial |
| 2 | 47.0 | L | 12.74 | 9.67 | Punctate, total |
| 3 | 26.0 | L | 23.64 | 22.67 | Punctate, partial |
| 4 | 75.0 | R | 9.85 | 16.63 | Punctate, total |
| 5 | 49.0 | R | 9.24 | 12.18 | Punctate, partial |
| 6 | 55.0 | L | 14.15 | 19.61 | Punctate, partial |
| 7 | 63.0 | L | 10.61 | 17.61 | Punctate, partial |
| 8 | 25.0 | R | 6.64 | 5.32 | Punctate, partial |
| 9 | 55.0 | L | 7.42 | 11.28 | Punctate, partial |
| 10 | 60.0 | R | 10.51 | 15.47 | Punctate, total |
| Mean | 50.5 | 10.99 | 14.13 | ||
R= right; L= left.
There were no cases of bilateral involvement. In all cases in group 2, ultrasound showed dilation of the lacrimal sac.
Anteroposterior and vertical dimensions of the lacrimal sac were measured in both groups. There was a significant difference between the two groups in terms of the anteroposterior dimension: Group 1=1.86 mm (Figures 2 A and 2 B) and group 2=10.99 mm (Figures 2 C and 2 D; p<0.0001). There was also a significant difference in the vertical dimension of the lacrimal sac between the groups (Group 1=9.79 mm and Group 2=14.13 mm; p=0.049). The most significant difference was observed in the anteroposterior dimension.
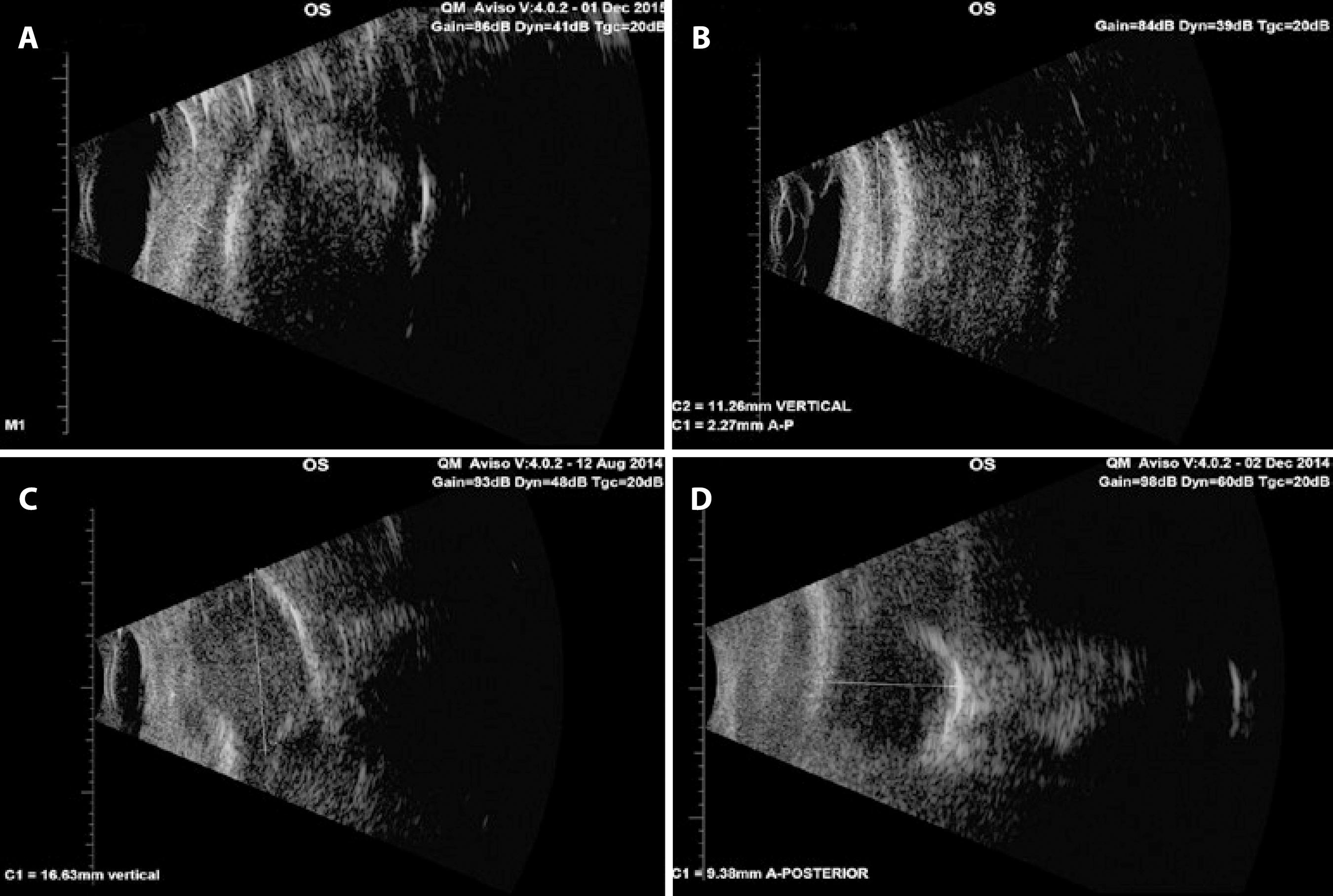
Figure 2 A and B) Normal lacrimal sac. A) Oval shape, hypoechogenic content. B) Oval shape, vertical diameter=11.26 mm, hypoechogenic content. C and D) Chronic dacryocystitis. Note the different shapes, sizes, and contents that an affected lacrimal sac can have. C) Oval shape, vertical diameter=16.63 mm, dense punctate content. D) Circular shape, anteroposterior diameter=9.38 mm, homogeneous, hypoechogenic punctate content.
Qualitative evaluation of the lacrimal sac content was also assessed using ultrasound. Normal lacrimal sacs contain hypoechogenic, homogeneous content (Figures 2 A and 2 B). A compromised lacrimal sac in chronic dacryocystitis may be partially or completely filled with punctate echoes, which are associated with inflammatory material (Figures 2 C and 2 D).
DISCUSSION
Currently, the diagnosis of chronic dacryocystitis is routinely per formed through clinical examination, which includes the test of digital expression of the lacrimal sac to evaluate the retrograde ex ter nalization of mucopurulent secretion through the puncta and dacryocystography with contrast material(4).
Ultrasound can be used for evaluation of the lacrimal sac and the adjacent lacrimal fossa tissue. Dacryocystography stands out as a better diagnostic test than ultrasonography for evaluating lacrimal flow.
Obstructions and/or congenital absence of lacrimal ducts that may affect puncta and lacrimal canaliculi make it difficult to evalua te the lacrimal sac by dacryocystography because they create an anatomical barrier to the passage of the contrast material(9). In these cases, ultrasonography can play a key role in the evaluation of the la crimal sac, especially when the obstruction occurs in the common canaliculus and in amnioceles(10).
In this paper, we present images of the lacrimal sac in patients with chronic dacryocystitis obtained using B-mode ultrasonography, revealing its dimensions and content, and compare these to those of normal cases. This information can help in surgical planning. If the lacrimal sac is atrophic, endonasal dacryocystorhinostomy is contraindicated because this procedure would make it difficult to locate structures anatomically(11).
There was a statistically significant clinical difference between the groups (normal and chronic dacryocystitis) regarding the quantitative parameters of the lacrimal sac, namely the anteroposterior and vertical measurements. In terms of the qualitative parameters evalua ted in this study, the content of the lacrimal sac could be correlated to the clinical presentation.
Ultrasonography using a 10-MHz transducer is more suitable for the evaluation of the lower lacrimal system, and the larger dimensions of the lacrimal sac in patients with chronic dacryocystitis allowed easier detection with this method. The upper lacrimal system can be evaluated using high-frequency ultrasound or ultrasound biomicroscopy with a 35-50-MHz transducer.
Other diagnostic methods that can be used to assess the nasola crimal duct, are computed tomography and magnetic resonance ima ging with or without contrast(12). Ultrasonography has some advantages over contrast-based exams, because it is a simple, fast, low-cost imaging method that does not expose the patient to radiation or contrast sensitivity.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

