INTRODUCTION
Drusen are extracellular deposits between the basal lamina of the retinal pigment epithelium (RPE) and the inner collagenous layer of Bruch's membrane. Although drusen occur more frequently in people above 50 years of age, some drusen patterns, e.g., cuticular drusen, Malattia Leventinese (ML), and large colloid drusen (LCD) can occur earlier(1,2). LCD are large (200-300 microns) yellowish, bilateral lesions with hyperpigmented borders scattered throughout the posterior pole. The LCD are found outside of the RPE as is common with conventional drusen(3-5). Reticular pseudodrusen also occur in the sub-retinal rather than in the sub-RPE space(2,3).
Optical coherence tomography (OCT) is an important tool for diffe rentiating between various drusen patterns(6,7). In most cases, LCD appear on OCT B-scans as multiple convex or dome-shaped structures with medium and homogeneous internal reflectivity and marked attenuation of the ellipsoid zone overlaying the LCD(1,8). These drusen are homogenously hyperfluorescent in late-phase fluorescein an giography images. In late-phase indocyanine green angiography (ICGA) images, LCD are either hyperfluorescent or hypofluorescent and surrounded by a discreet hyperfluorescent halo(8).
This report presents structural en face OCT findings of LCD and correlations of these with findings with fluorescein angiography and ICGA.
CASE REPORT
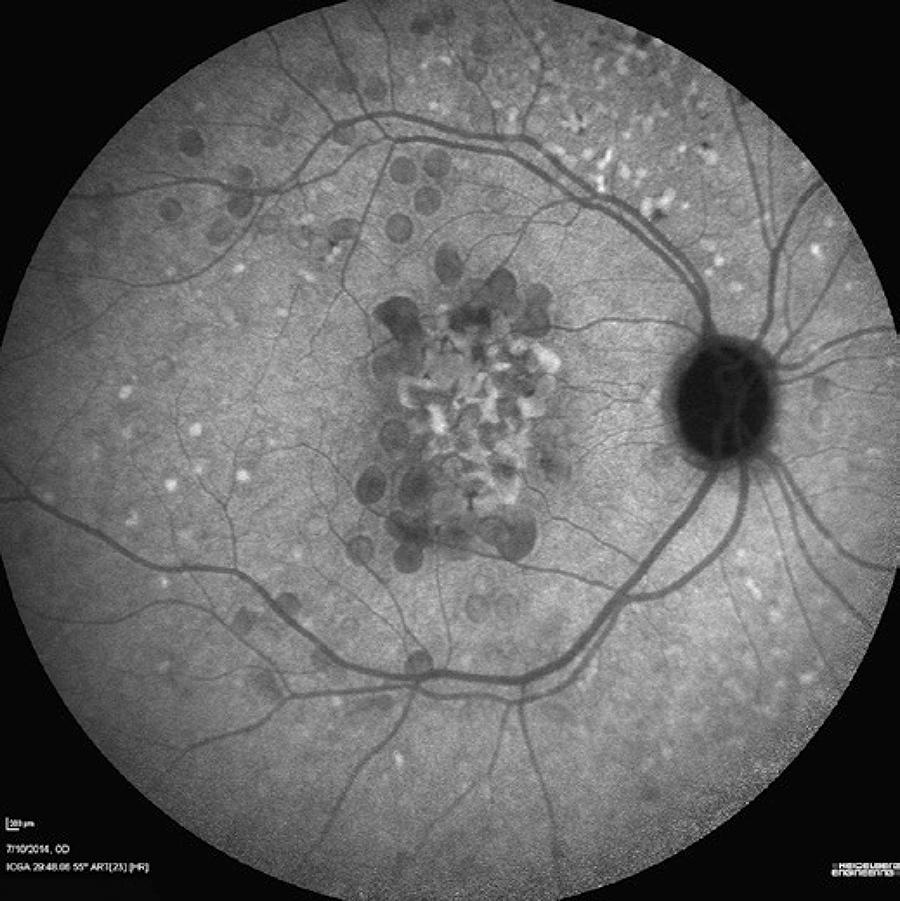
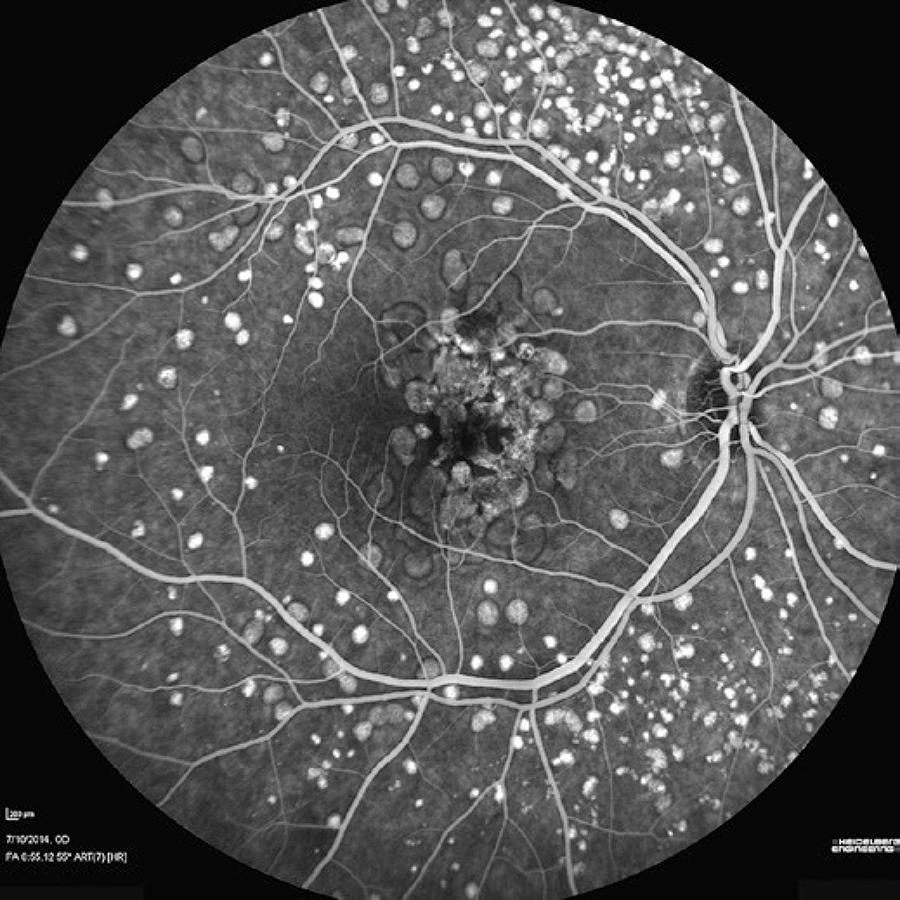
A 55-year-old Caucasian woman from São Paulo, Brazil, presented with the chief complaint of a 5-year history of progressively worsening vision, particularly in the left eye. She had a 70-pack/year smoking history and a diagnosis of emphysema. She had not had any previous ocular surgeries, and there was no history of other familial diseases. Her best-corrected visual acuity levels were 20/40 in the right eye and 20/400 in the left eye. The pupillary reflexes were preserved and the anterior segment was normal. Indirect ophthalmoscopy revealed large sub-retinal yellowish lesions in the macular area and the mid periphery of the retina bilaterally. Fluorescein angiography showed early hyperfluorescence; ICGA showed that most drusen appeared hypofluorescent. En face OCT showed a hyper-reflective center surrounded by a hypo-reflective halo, which was bordered by hyper-reflective and hypo-reflective rings. In OCT B-scans, all drusen appeared convex with medium and homogenous internal reflectivity, marked attenuation of the ellipsoid zone overlaying the LCD, and RPE atrophy. Posterior segment findings can be seen in figure 1, while figure 2-4 display image findings. A conservative approach was adopted, and the patient was instructed to quit smoking and perform the Amsler Grid test routinely.
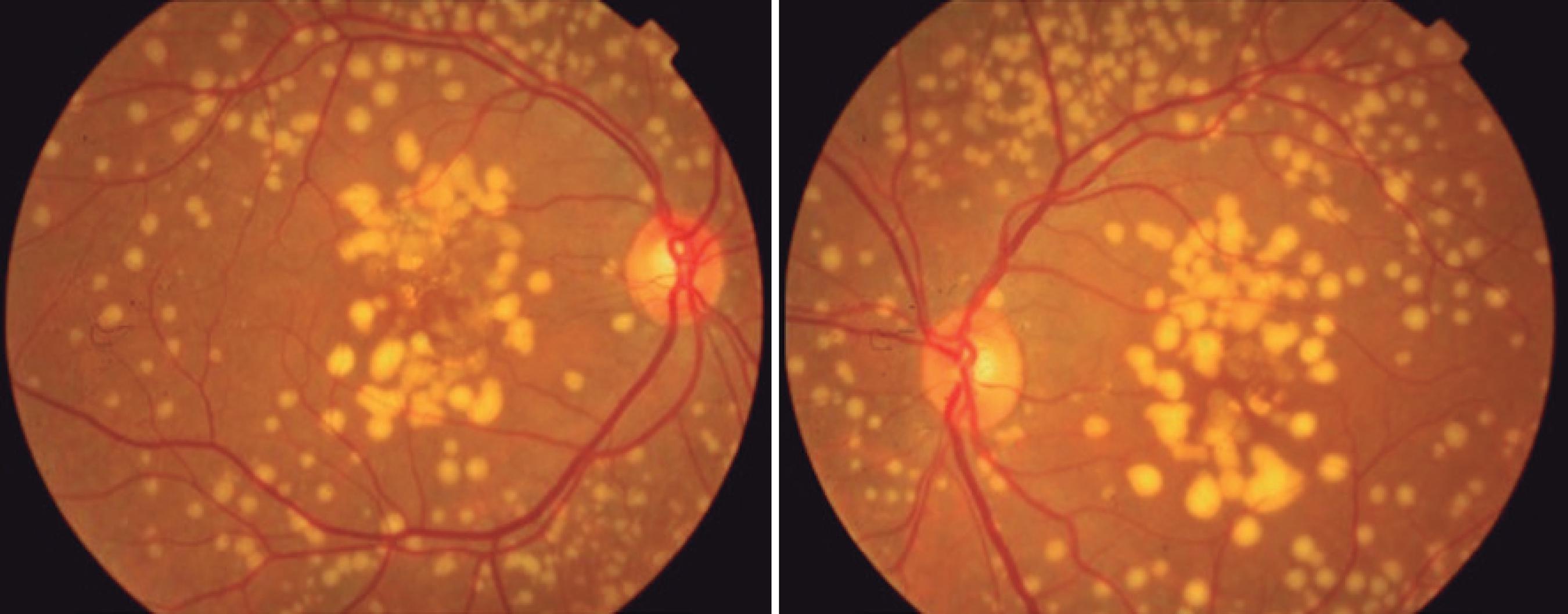
Figure 1 A fundus photograph showing large, bilateral, yellowish lesions in the macular area and retinal periphery.
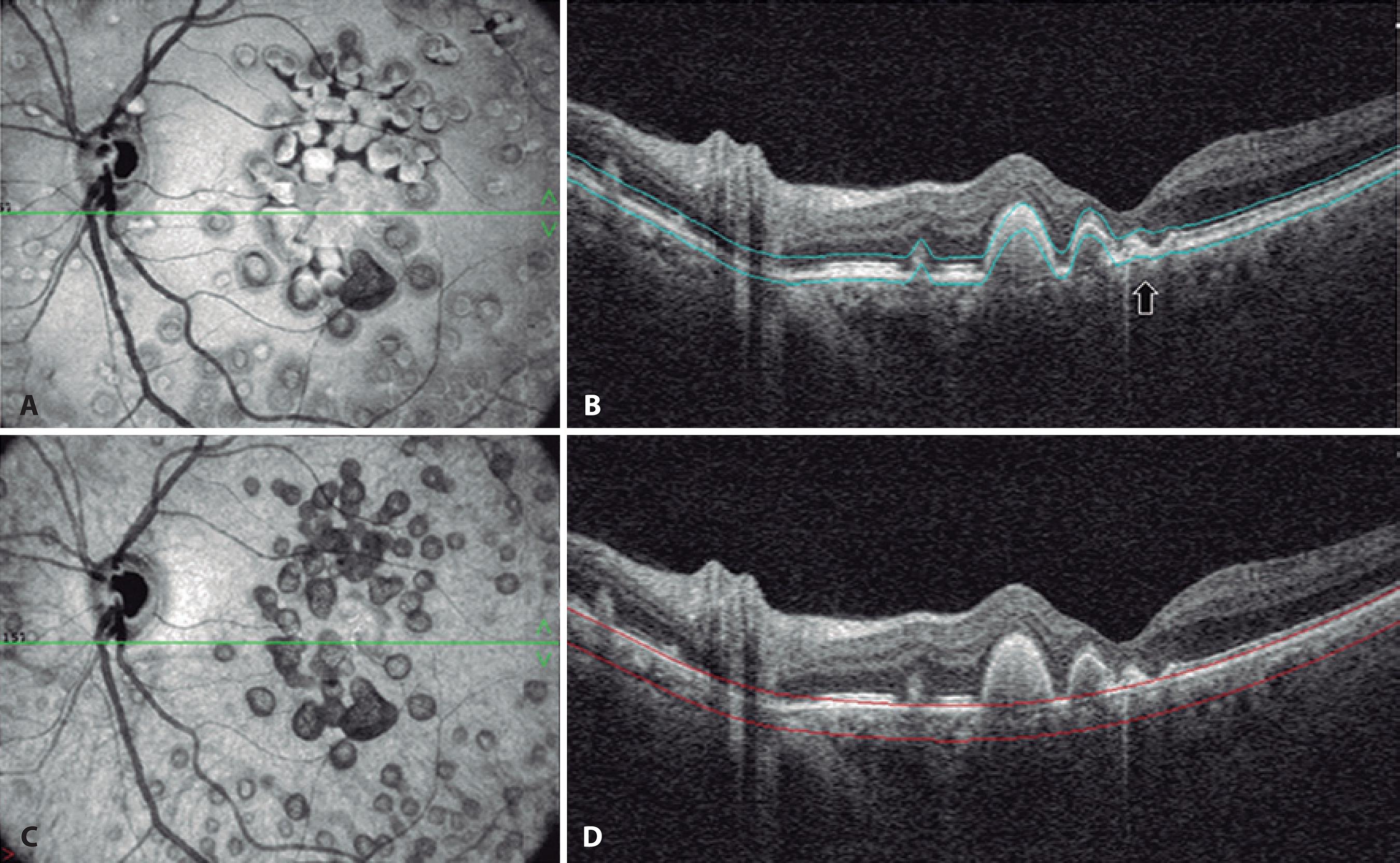
Figure 2 Optical coherence tomography (OCT) images obtained from a 55-year-old woman with large colloid drusen (LCD). A) Structural en face OCT with upper segmentation line located at the avascular outer retina and lower segmentation line placed at the sub-retinal pigment epithelium (RPE) space showing a hyper-reflective center surrounded by a hypo-reflective halo, bordered by hyper-reflective and hypo-reflective rings, similar to the donut effect. B) Corresponding OCT B-scan of (A) showing the convex contour of LCD with medium and homogeneous internal reflectivity under the RPE, as well as marked thinning of the outer nuclear and ellipsoid layers. A small area of RPE atrophy as seen under the horizontal foveal scan, identified as reverse shadowing (black arrow). No fluid accumulation is observed. C) Structural en face OCT on a choroid slab showing a hyper-reflective center surrounded by a hypo-reflective halo. D) Choroidal features on the OCT B-scan were not well defined due to signal blockage caused by the colloid drusen.
DISCUSSION
Large colloid drusen develop most often in women without a fa milial history of retinal problems. Drusen do not seem to be related to an increased risk of choroidal neovascularization or significant loss of mean visual acuity(3). The precise incidence and prevalence of cho roidal neovascularization in LCD is not well characterized, but most clinicians believe its incidence is significantly lower than in age-re lated macular degeneration(9).
The images obtained from this patient showed features of LCD. In the late-phase ICGA images, the larger drusen appeared hyperfluorescent with a hypofluorescent halo, traditionally described as the donut effect(3) (Figure 3). Drusen are lipid-rich, and the relative hydrophobicity of the commonly used angiographic dyes differs. A difference in the lipid composition between the core and the periphery of LCD has been reported, which might be responsible for the typical donut shape observed in the ICGA images(1).
The structural en face OCT images showed a hyper-reflective center surrounded by a hypo-reflective halo bordered by two rings, one of which was hyper-reflective and the other hypo-reflective, similar to the donut effect seen on the ICGA images (Figure 2). OCT is noninvasive and can help differentiate LCD from other early-onset drusen, such as Malattia Leventinese and cuticular drusen. In OCT images, LCD have been described as having a sawtooth pattern, with the height of each LCD approximately equal to its basal diameter. The neurosensory retina appears to be spared in the area overlaying the drusen, although the overlaying RPE is much thinner at the apex of each druse than between the drusen. In Malattia Leventinese, confluent sub-RPE accumulation on OCT has been reported. The smaller drusen of this condition have a radial distribution and a confluence of large drusen with sub-retinal fibrous plaque occurs. The typically pale drusen are adjacent to the optic disc(3). Furthermore, OCT allows observation of focal loss of cellular visibility, which has a mosaic pattern in patients presenting with drusen(6,7). The smallest LCD do not affect the ellipsoid zone(5). This imaging approach might serve as the foundation for valuable imaging-based biomarkers for detecting the earliest disease stages, tracking progression, and monitoring treatment response(9).
On fluorescein angiography images, drusen hyperfluorescence increased quickly, especially in the middle periphery. The areas of hy perfluorescent lesions did not vary among the capillary, venous, and washout angiography phases(4) (Figure 4). One study reported that large visible drusen in a group of adults with early-onset drusen were concentric to regions of hyperfluorescence, suggesting that drusen might have clinically detectable, substructural domains(9). Similarly, in another study, the measurements of the drusen areas on OCT were smaller than the measurements obtained from color fundus images(10).
These results led us to conclude that structural en face OCT is a useful noninvasive tool that facilitates better morphologic evaluation and quantification of structural changes in LCD on high-resolution images. While traditional OCT produces longitudinal cross-sectional images, en face OCT produces transverse images of the retinal and choroidal layers at any specified depth. This provides an extensive overview of the pathological structures in one image. Thus, combining dye-based angiographic images with structural en face OCT may provide a better understanding of this retinal entity.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

