INTRODUCTION
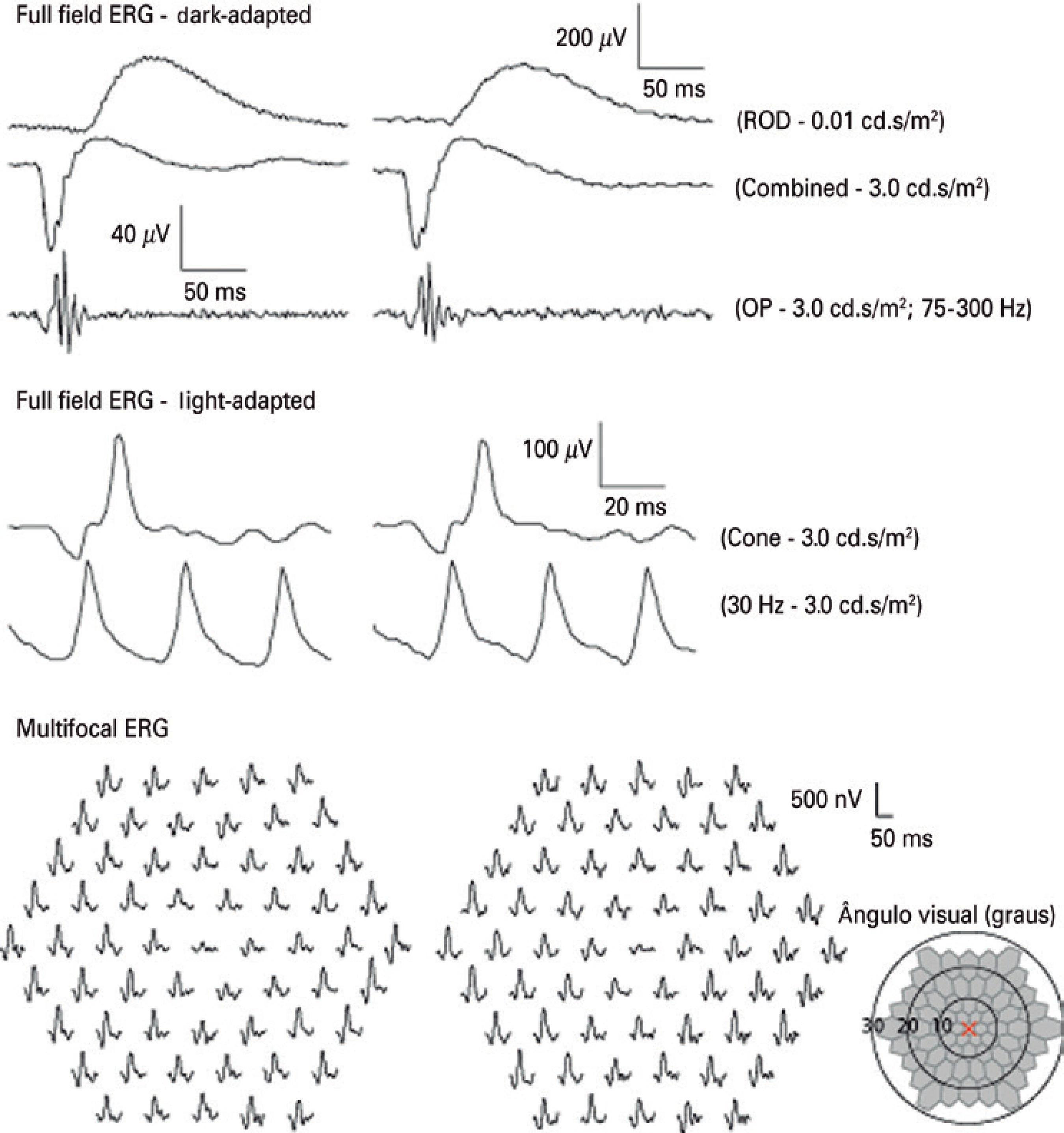
Occult macular dystrophy (OMD) is an uncommon hereditary disease characterized by the absence of fundoscopic abnormalities, which generally occur with progressive reduction of visual acuity(1). Affected patients show normal full-field electroretinogram (ERG) responses and centrally reduced multifocal ERG responses(1). This finding is the main symptom that differentiates OMD from entities such as optic neuritis, dominant optic atrophy, amblyopia, or psychological disorders(2).
The adaptive optics (AO) system permits detection of changes in the photoreceptor layer(3). In the present case, the photoreceptor layer was evaluated using the rtx Adaptive Optics Retinal Camera (Imagine Eyes; Orsay, France). This system is based on En-face reflectance imaging illuminated using a central illumination wavelength of 850 nm (infrared) with a 4 × 4-degree image field (1.2 × 1.2 mm on the retina) and a 600-mm focus interval, acquiring high-resolution cone images. The images were processed using the CK software (V 0.1) and AO detect (V 0.1) (Imagine Eyes). The spatial distribution of points was analyzed according to intercellular spacing, focal cell density, and the number of closely neighboring cells.
Microperimetry was proposed as a more suitable technique to do cument visual field changes in OMD compared with conventional perimetry because of small and oftentimes relative scotoma(4). In the present study, we examined the correlation between spectral-do main optical coherence tomography (SD-OCT) images, AO, micrope rimetry, and multifocal electroretinography (mfERG) in a patient with OMD.
CASE REPORT
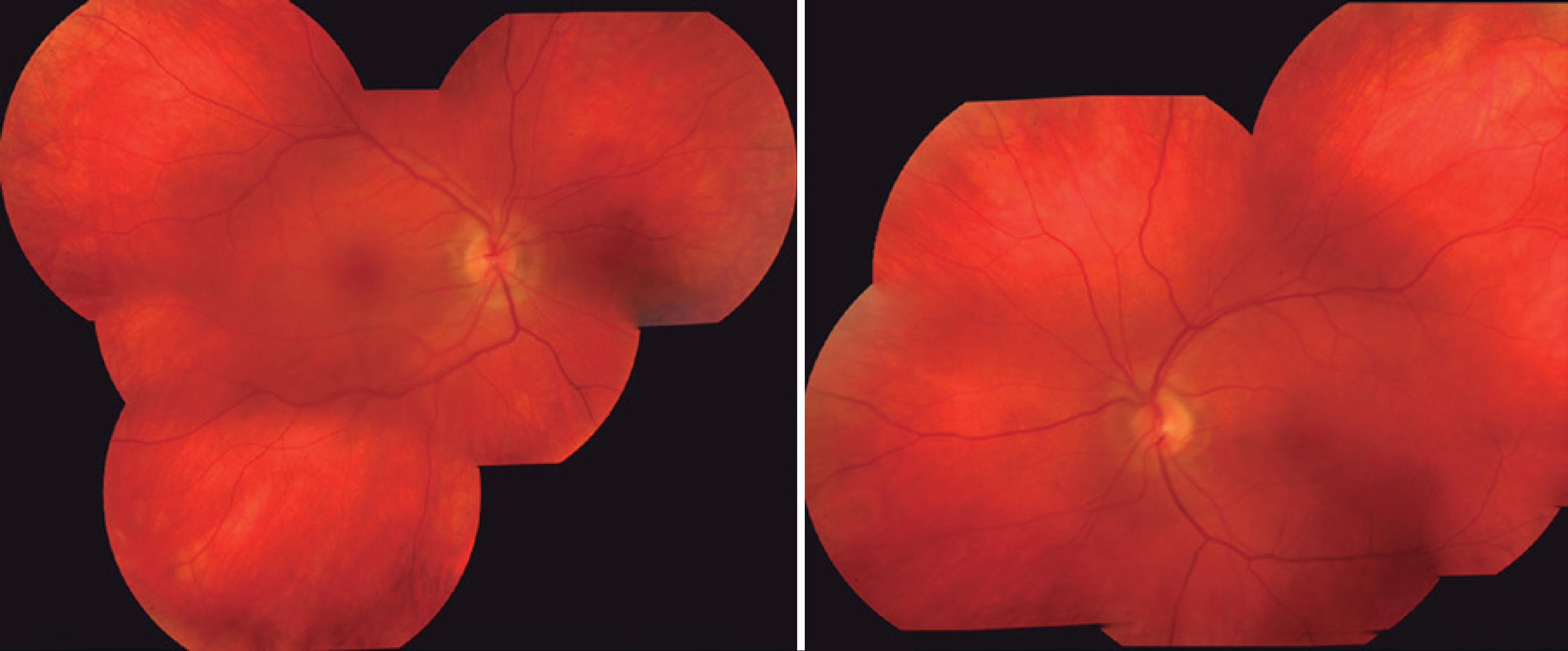
A 40-year-old man admitted to the neuro-ophthalmology service of our institution reported bilateral, painless loss of visual acuity that started during childhood and worsened during the last 7 years. His corrected visual acuity was 20/80 in the right eye (OD) and 20/50 in the left eye (OS). Biomicroscopy revealed a transparent cornea, a trophic iris, and a transparent crystalline lens. Intraocular pressures were 14 mmHg OD and 13 mmHg OE. Fundoscopy revealed an optic nerve with precise limits, physiological excavation, vessels of preserved ca liber, and macula with preserved brightness in both eyes (Figure 1). Microperimetry revealed loss of sensitivity at the fovea, but preserved bilateral central fixation. Average thresholds were OD: 20.2 dB; OS: 23.9 dB; fixation stability index P1, OD: 72% and OS: 89% (Figure 2). Optical coherence tomography (OCT) revealed discontinuity of the photoreceptor layer in the foveal region of both eyes (Figure 2).
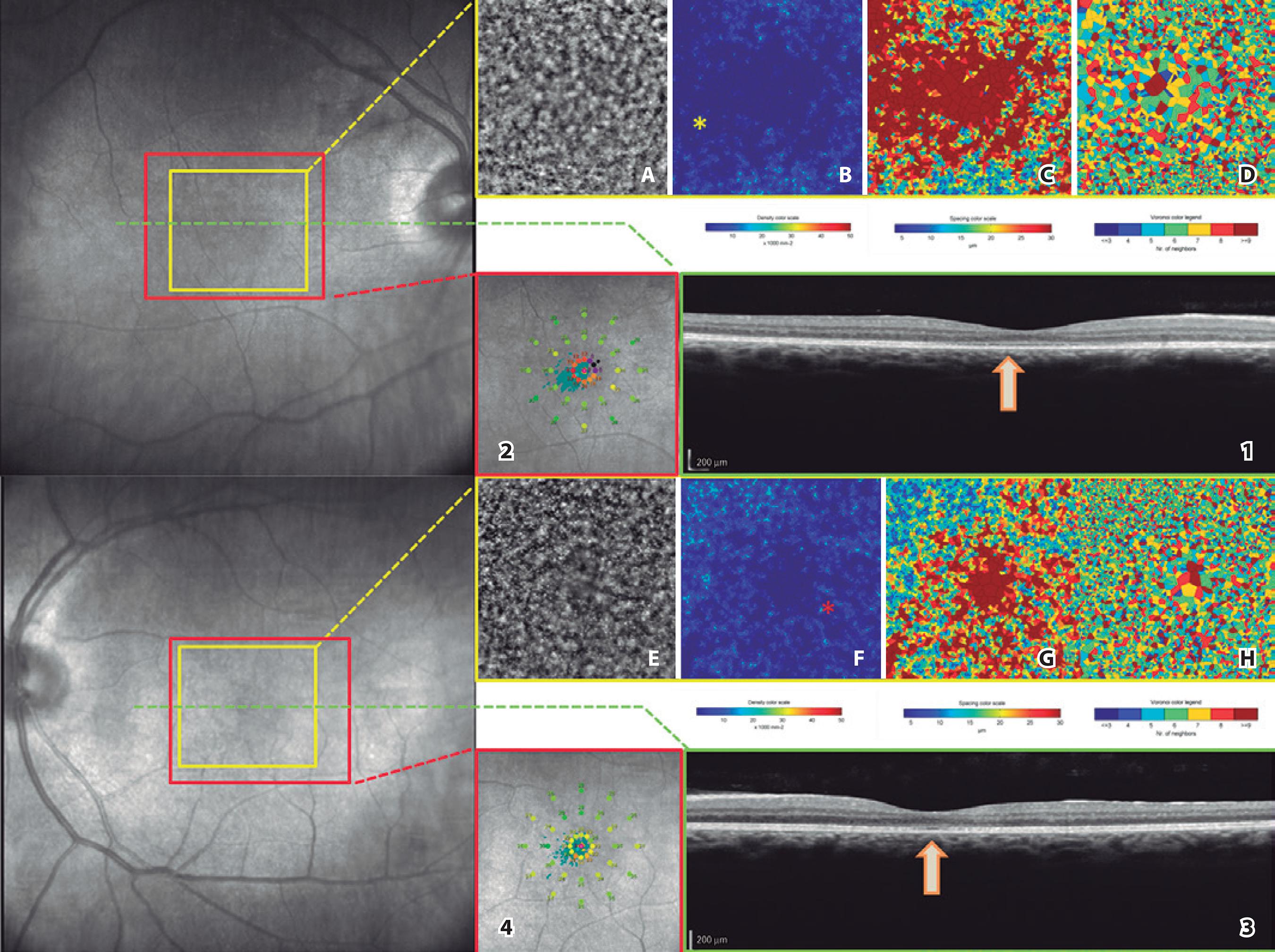
Figure 2 Optical coherence tomography (1-3), adaptive optics (A-H), and microperimetry (2-4) images of a patient with occult macular dystrophy. (Arrows) Loss of continuity of the outer photoreceptor layer in the central foveal region. (yellow asterisk) Reduced ring photoreceptor density in the foveal region. (2) Reduction of ring sensitivity in the central foveal region. (Red Asterisk) Reduced photoreceptor density in a central foveal region. (4) Reduced central sensitivity in the fovea.
Using adaptive optics, we obtained a mean density of 2,754 cones/mm2 in OD and 4,204 cones/mm2 in the central area (reference value, 20,000-30,000). The proportion of neighboring cells (Voronoi polygons) was 6 (29.5%) in OD and 6 (30.8%) in OS (reference value, 6). Spacing between cells was 18.90 µm in OD and 15.83 µm in OS (reference value, 15-20 µm) (Figure 2). Full-field ERG revealed a normal response amplitude (Figure 3) and multifocal ERG showed reduced amplitude of photoreceptor central responses (Figure 3).
DISCUSSION
OMD is a hereditary disease that involves retinal dysfunction only in the fovea, causing altered responses to multifocal ERG without changing the full-field ERG or causing apparent changes in ophthalmoscopy or fluorescein angiography(1). SD-OCT analyses reveal detailed retinal structures and abnormal morphology in patients with OMD(5), including thinning of the fovea and the outer nuclear layer, as well as interruption of the inner and outer segment junction (IS/OS line). The thickness of the photoreceptor layer and the interruption detected using SD-OCT correlate with visual function and disease progression(6). In the present patient, we observed similar changes in SD-OCT and reduction of visual acuity. We examined the correlations between SD-OCT, adaptive optics images, and the sensitivity potentials of the photoreceptors using microperimetry and observed that the region with loss of IS/OS continuity exhibited a lower density of the photoreceptor mosaic, sensitivity loss, and reduction of the response potentials using mfERG.
This close topographical correspondence between the functional and structurally damaged retina is important because it might help to differentiate OMD from other macular dystrophies such as Stargardt disease, in which this correlation might be absent(7).
The pathological changes that characterize OMD seem to be lo calized to the posterior retinal layers, and "in-vivo" investigation of pho toreceptors using AO seems to be interesting. For example, Kita guchi et al. used AO to detect irregular dark areas in the eyes of patients with OMD(8) and Nakanishi et al. concluded that a significant reduction in cone density in a sparse array of photoreceptors of the ma cula should be considered a feature of OMD(9).
In the present patient, cone densities were lower around the fovea compared with those in the paracentral retina in both eyes. Further, the temporal paracentral area of the right eye exhibited reduced cone density compared with that of the nasal paracentral retina, consistent with findings reported by Tojo et al.(10).
AO imaging can be useful for monitoring changes in photore ceptors in patients with OMD. Future studies should use AO to deter mine photoreceptor densities of a larger number of patients with OMD as a function of time to evaluate longitudinal photoreceptors changes and their correlation to other imaging findings, allowing diagnoses that are more precise and contributing to a better understanding of disease progression and prognosis.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

