INTRODUCTION
Contrast sensitivity (CS) is the ability to recognize small differences in luminance or differentiate two objects from each other and the background(1,2). CS is an important part of functional vision that is related to many activities of daily living and measuring it is one of the best ways to assess vision quality(3-5). Despite having normal visual acuity measured by a Snellen chart, the satisfaction with the results of refractive surgery may vary relative to CS, and some eye diseases cause isolated loss of CS(4,6-8). Snellen acuity tests have a limited ability to detect fine changes in contrast because high contrast letters (black on white) are used(9). Also, recent advances in knowledge about refractive surgery, optical tissues, and glaucoma and macular diseases revealed that the Snellen acuity test is inadequate for early detection of eye diseases and measurement of functional vision(6,10-12). CS decreases in all stages of glaucoma and age-related macular degeneration (AMD) have been documented using different testing methods(7,12-15). Glaucoma, cataract, and AMD patients suffer from problems in vision-related activities of daily living and the inability to recognize targets in real world, which can be better identified by CS tests than by visual acuity tests(14,16-18). The increasing importance of visual quality and the need for accurate measurement of visual acuity has led to more interest in CS tests(12,19-21).
There are several clinical tests for measuring CS with letters or gratings(5,22-26). A limitation of CS tests is low reliability associated with varying environmental conditions and the subjective nature of the tests. In particular, CS tests that use charts may be affected by inadequate or uneven lighting, fading, the subject's learning curve, and reflections(2,3). The Functional Acuity Contrast Test (FACT) assesses five spatial frequencies (1.5, 3, 6, 12, and 18 cycles per degree (cpd)) and 9 levels of contrast for each frequency. FACT uses a small increment (0.15 log unit) and a forced-choice method with three options(2). Although the FACT test has greater reliability compared with other CS testing methods, administration of the CS test in a closed system, with charts on the screen inside the device, with a Functional Visual Acuity (FVA) device has additional advantages. These advantages include the ability to display contrast charts in a random order and the administration of the test with standardized lighting, which is difficult to maintain under other conditions(3,27). A CS test is expected to have a good reliability to differentiate a small loss or detect real progression, which can be better achieved by a closed test system, which has inherently stable testing conditions.
To the best of our knowledge, there has been little research published about the comparative reliability of these devices for healthy controls and patients with eye disease. This study investigates the repeatability of the closed system FVA CS test in control subjects and in patients with glaucoma, cataracts and good Snellen visual acuity, or age-related macular degeneration (AMD).
METHODS
This prospective, observational study included patients with glaucoma, cataracts, or AMD and healthy control subjects. All subjects were recruited from the Eye Clinic at Canakkale Onsekiz Mart University. Written informed consent was obtained from all participants following a comprehensive explanation of the study. The research was approved by the local clinical research ethics committee and complied with the tenets of the Helsinki Declaration.
The study included subjects between 40 and 70 years old to facilitate enrollment of subjects with best corrected visual acuity (BCVA) of 0.00 logMAR for the groups without cataracts. One eye of each patient was included in the study. Subjects were not eligible to be included if they had ocular diseases other than glaucoma, cataracts, or AMD, refractive error <-3 or >3 diopters (D) sphere or >2.00 D cylinder, or a history of previous eye surgery or laser treatment. Patients with psychiatric or neurologic disorders, poor compliance during the CS test, or who used systemic or ocular medications could affect CS were excluded. All patients underwent an ophthalmic examination, including auto refractometry, BCVA evaluation, anterior segment biomicroscopy, funduscopy, and IOP, measured with a Goldmann applanation tonometer (GAT).
The glaucoma group included subjects who were diagnosed with primary open-angle glaucoma (POAG) or normotensive glaucoma (NTG). The inclusion criteria for patients with POAG were the characteristic visual field loss, glaucomatous optic neuropathy (having rim thinning or notching, retinal nerve fiber layer defects, or disc hemorrhage and disc asymmetry between the eyes ≥0.2), and intraocular pressure (IOP) >21 mmHg. The inclusion criteria for patients with NTG were visual field loss, glaucomatous optic neuropathy, and IOP ≤21 mmHg. Glaucomatous visual field defects, which were repeatable in at least two standard automated perimetry evaluations, included at least one of the following: nasal step, arcuate scotoma, paracentral scotoma, or temporal wedge. All glaucoma patients had a grade 3 or 4 open angle according to the Shaffer Classification System(29) and a mean deviation no worse than -6 dB.
In the cataract group, only eyes with a BCVA of 0.17 logMAR or better and a nuclear sclerosis of less than grade 2 were included. Nuclear sclerosis was graded by the slit-lamp method according to the Lens Opacities Classification System III(28). The inclusion criteria for the AMD group were retinal pigment epithelial abnormalities in the form of hypopigmentation or hyperpigmentation, without evidence of active choroidal neovascularization, and no prior treatment with any anti-vascular endothelial growth factor injections. The control subjects had normal findings on a comprehensive eye examination (including anterior segment biomicroscopy and fundoscopy of the macula and optic nerve) and IOP <21 mmHg.
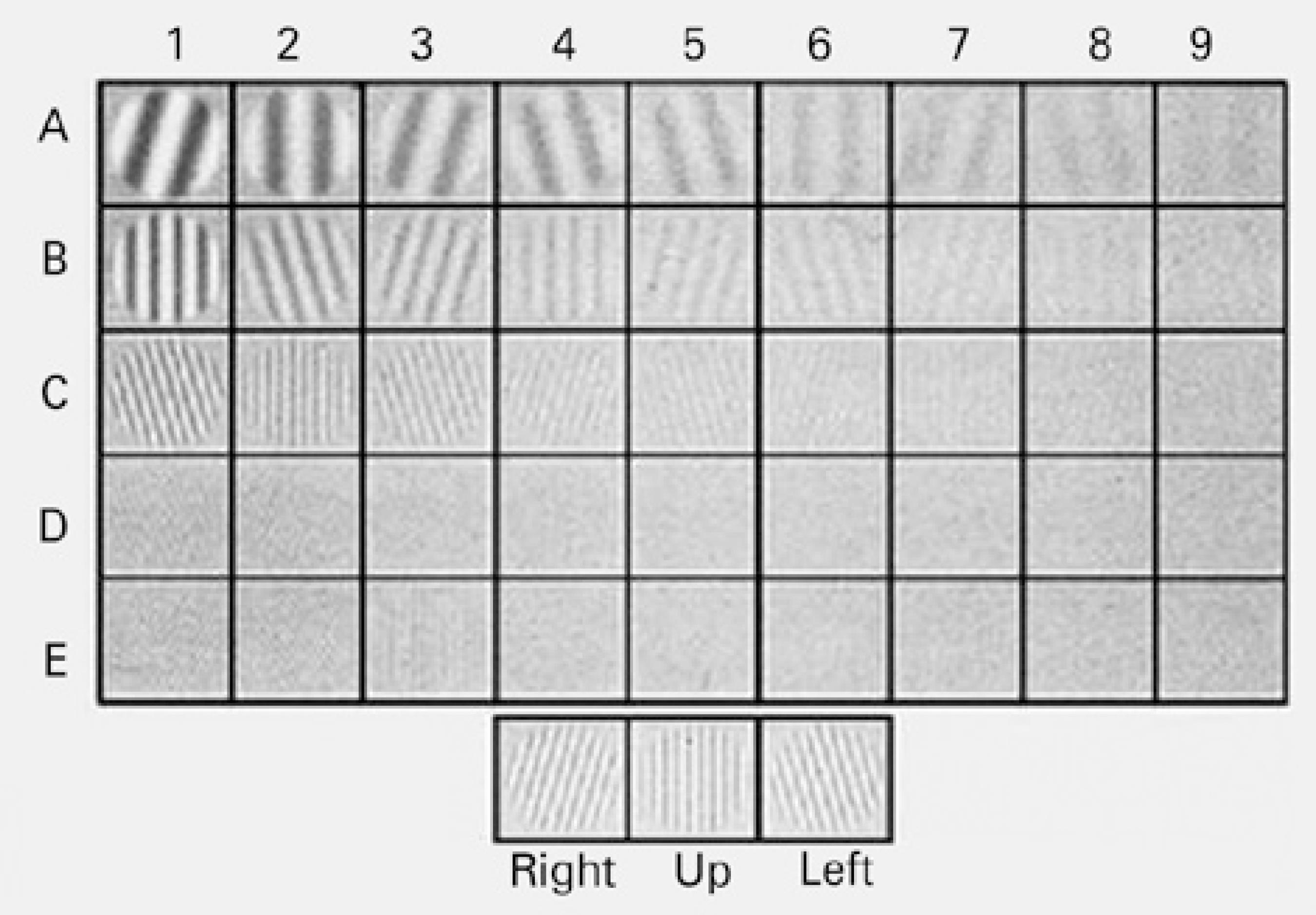
A closed-system CS testing device, the OPTEC-FVA (Stereo Optical Co, Inc., Chicago, IL, USA), was used to examine CS values under daytime without glare. Figure 1 shows the FVA CS testing device. The FVA has rotating slide packages for other visual functions, including visual acuity, disability glare, and stereo and color vision. The CS testing device contains the FACT chart, which uses three orientations for the gratings: oriented vertically or tilted 15º to the right or left. Subjects identified the orientation of each grating and were required to guess when they could not determine the orientation of gratings.
The CS testing device controls light levels with sensors to achieve consistent conditions for each test. This device supplies a target luminance level of 85 cd/m2 for daytime conditions in compliance with the American National Standards Institute (ANSI). It evaluates spatial frequencies using sine-wave grating charts of 1.5, 3, 6, 12, and 18 cpd. Figure 2 presents the sine-wave gratings charts for the frequencies that the CS testing device used. Contrast was defined according to the Michelson formula (C = [Lmaximum − Lminimum]/[Lmaximum + Lminimum], C: Contrast, L: Luminance)(2). CS was measured during two sessions separated by at least one week and up to one month (intersession). At each session, two measurements taken 30 minutes apart (intrasession). All tests were performed with the optimum refractive correction and a natural pupil. All the subjects performed the CS test for the first time during our study, and each test lasted approximately 10 minutes. The CS measurements were obtained by a single operator who was blinded to the patient's group.
All the CS values were converted to logarithmic values. The test-retest reliability of the CS test was examined using the intraclass correlation coefficient (ICC) and the coefficient of repeatability (COR) and the corresponding 95% confidence interval (CI). The ICC was calculated with absolute agreement. The COR is calculated as 1.96 times the standard deviation of the difference between the test and retest scores. An ICC value of 1.0 and a COR value of 0.0 represent perfect test-retest reliability(2). Reliability analyses were performed within individual sessions and between sessions for all groups. Possible floor and ceiling effects were evaluated by calculating the percentage of subjects with lowest and highest test scores, respectively, for each of the four tests at each spatial frequency and within each group.
Spearman rank-order correlations were used to investigate the possible correlation between age and changes in CS score. The Wilcoxon and Mann-Whitney U-tests were used to compare CS scores between groups. The Bonferroni correction, which applies a statistical significance level of 1/n times the "p" value (n= the number of comparisons), was used to test for multiple comparisons to ensure that an appropriate level of significance was applied to the individual tests(30). Statistical analysis was performed using SPSS software (Windows version 19.0; SPSS, Inc., Chicago, IL, USA), and statistical significance was defined as p<0.05.
RESULTS
The analysis was included 90 eyes of 90 Caucasian subjects, including healthy control (n=30; mean ± standard deviation age 47.1 ± 6.7 years; 15 males), glaucoma (n=13; age 59.6 ± 4.1 years; 8 males), cataract (n=29; age 56.3 ± 5.2 years; 14 males), and AMD (n=18; age 59.9 ± 4.6 years; 9 males) groups.
The test-retest reliability of the CS test, including ICC and COR, is shown in table 1. The reliability of the CS test in the control, glaucoma, cataract, and AMD groups were good at the first session (ICC: 0.87 [95% CI 0.84 -0.9], 0.90 [CI 0.84 -0.96], 0.76 [CI 0.65 -0.87], and 0.69 [CI 0.59 -0.79], respectively; and COR 0.24, 0.20, 0.38, and 0.25, respectively). However, at the second session, statistically significant increases were found in the reliability of the CS test, except in the glaucoma group (ICC: 0.92 [CI 0.88 -0.96], p=0.042; 0.93 [CI 0.88 -0.98], p=0.461; 0.90 [CI 0.86 -0.94], p=0.043; and 0.86 [CI 0.82 -0.9], p=0.043; and COR of 0.16, 0.16, 0.24, and 0.21 in the control, glaucoma, cataract, and AMD groups, respectively).
Table 1 Test-retest reliability of the contrast sensitivity test in the groups of control, glaucoma, cataract, and age-related macular degeneration groups
| Spatial | 1st session | 2nd session | Intersession | ||||||
|---|---|---|---|---|---|---|---|---|---|
| frequency (cpd) | ICC | COR | ICC | COR | p-value | ICC | COR | ||
| Control group |
|||||||||
| 1.5 | 0.86 | 0.19 | 0.91 | 0.13 | 0.92 | 0.14 | |||
| 3 | 0.86 | 0.18 | 0.89 | 0.16 | 0.95 | 0.10 | |||
| 6 | 0.83 | 0.23 | 0.87 | 0.20 | 0.042*a | 0.91 | 0.16 | ||
| 12 | 0.91 | 0.23 | 0.96 | 0.15 | 0.043*b | 0.94 | 0.18 | ||
| 18 | 0.87 | 0.38 | 0.96 | 0.18 | 0.94 | 0.23 | |||
| Mean | 0.87 | 0.24 | 0.92 | 0.16 | 0.93 | 0.16 | |||
| Glaucoma group |
|||||||||
| 1.5 | 0.92 | 0.14 | 0.83 | 0.22 | 0.96 | 0.10 | |||
| 3 | 0.80 | 0.24 | 0.92 | 0.15 | 0.95 | 0.11 | |||
| 6 | 0.85 | 0.22 | 0.94 | 0.14 | 0.461a | 0.86 | 0.20 | ||
| 12 | 0.95 | 0.20 | 0.97 | 0.11 | 0.194b | 0.96 | 0.15 | ||
| 18 | 0.98 | 0.18 | 0.98 | 0.18 | 0.98 | 0.19 | |||
| Mean | 0.90 | 0.20 | 0.93 | 0.16 | 0.94 | 0.15 | |||
| Cataract group |
|||||||||
| 1.5 | 0.86 | 0.22 | 0.88 | 0.17 | 0.94 | 0.14 | |||
| 3 | 0.84 | 0.23 | 0.94 | 0.14 | 0.96 | 0.10 | |||
| 6 | 0.86 | 0.25 | 0.93 | 0.18 | 0.043*a | 0.96 | 0.14 | ||
| 12 | 0.56 | 0.56 | 0.85 | 0.37 | 0.043*b | 0.81 | 0.34 | ||
| 18 | 0.70 | 0.67 | 0.92 | 0.33 | 0.96 | 0.22 | |||
| Mean | 0.76 | 0.38 | 0.90 | 0.24 | 0.93 | 0.19 | |||
| AMD group |
|||||||||
| 1.5 | 0.72 | 0.17 | 0.88 | 0.14 | 0.93 | 0.09 | |||
| 3 | 0.74 | 0.19 | 0.84 | 0.16 | 0.91 | 0.10 | |||
| 6 | 0.62 | 0.23 | 0.80 | 0.23 | 0.043*a | 0.88 | 0.13 | ||
| 12 | 0.83 | 0.18 | 0.90 | 0.20 | 0.141b | 0.90 | 0.15 | ||
| 18 | 0.56 | 0.50 | 0.90 | 0.32 | 0.68 | 0.42 | |||
| Mean | 0.69 | 0.25 | 0.86 | 0.21 | 0.86 | 0.18 | |||
AMD= age-related macular degeneration; ICC= Intraclass correlation coefficient; COR= coefficient of repeatability; cpd= cycle per degree.
*statistically significant p<0.05.
ap-value of Wilcoxon signed-rank test for ICC of 1st and 2nd sessions.
bp-value of Wilcoxon signed-rank test for COR of 1st and 2nd sessions.
Figure 3 illustrates the mean CS score for all groups as a function of spatial frequency. The CS scores for the AMD group were significantly lower than for those in the control group at all frequencies (significance of Bonferroni correction 0.012, p<0.001). In the glaucoma group, except at a frequency of 1.5 cpd, the CS scores were significantly lower compared with control group (significance of Bonferroni correction 0.012, p<0.012). There was also a statistically significant correlation between age and changes in CS scores of subjects at all spatial frequencies (1st session p<0.001, r=-0.399, -0.484, -0.484, -0.386, and -0.395 at 1.5, 3, 6, 12, and 18 cpd, respectively; 2nd session p<0.001, r=-0.424, -0.450, -0.495, -0.432, and -0.444 at 1.5, 3, 6, 12, and 18 cpd, respectively).
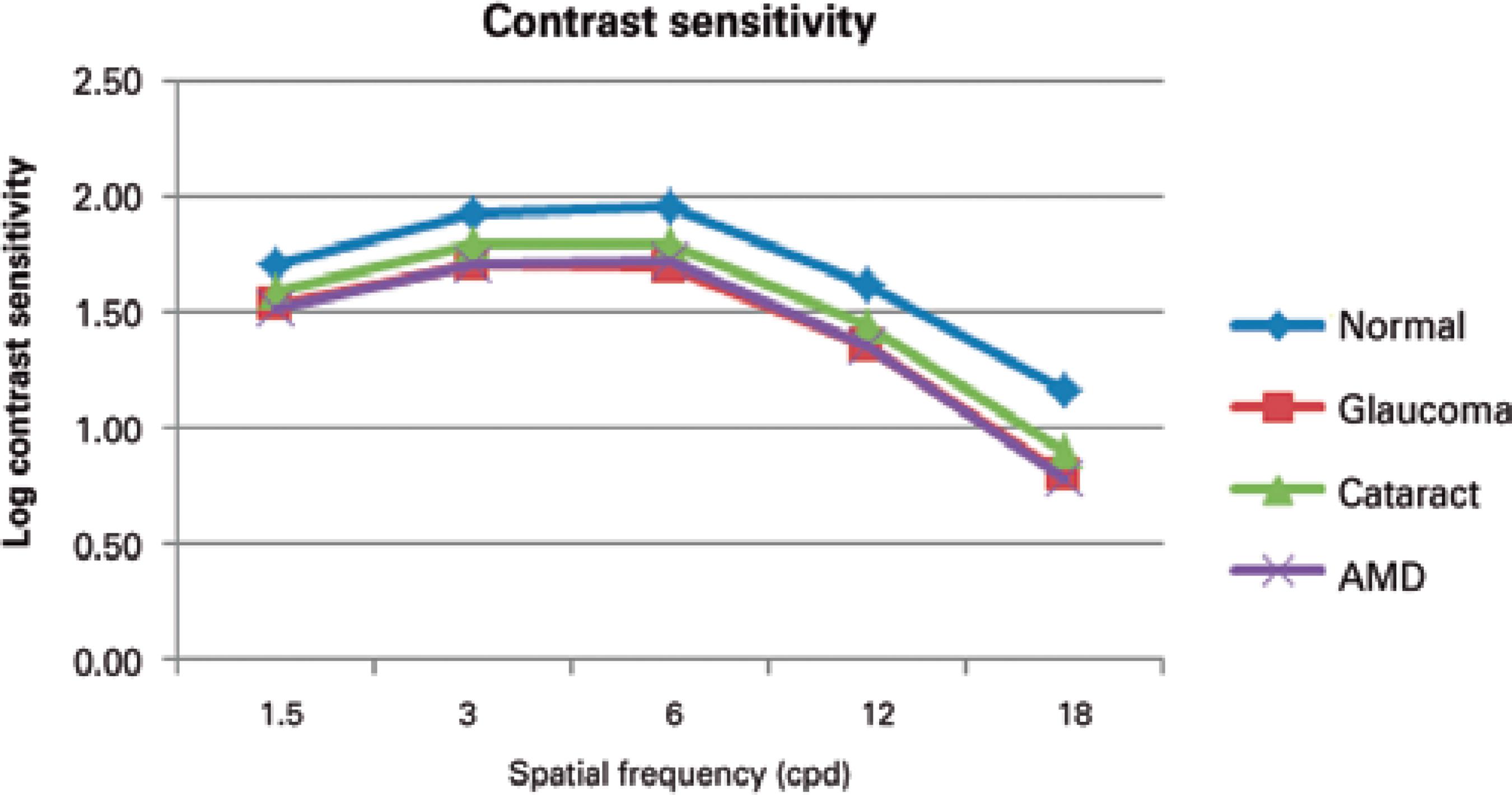
Figure 3 Contrast sensitivity for the control, glaucoma, cataract, and age-related macular degeneration (AMD) groups as a function of spatial frequency.
Table 2 summarizes the results of the analysis of possible floor and ceiling effects at each spatial frequency and for each group. There was a prominent floor effect at the highest frequency (18 cpd) in all groups. In healthy eyes, a floor effect, except in the second test, only occurred at 18 cpd. However, in the glaucoma group, the floor effect was greatest for the first two tests and decreased for the last CS tests. There was no ceiling effect in the glaucoma or AMD groups at any of the tested frequencies. In healthy and cataract eyes, a low ceiling effect (3.3%-10%), with a slight decrease during the last two tests, was detected.
Table 2 The floor and ceiling effect for each spatial frequency and group (measured by the percentage of maximum and minimum CS scores in the control (n=30), glaucoma (n=13), cataract (n=29), and AMD (n=18) groups)
| Percentage with the minimum CS score for each spatial frequency (%) |
Percentage with the maximum CS score for each spatial frequency (%) |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Test | Group | 1.5 | 3 | 6 | 12 | 18 | 1.5 | 3 | 6 | 12 | 18 | |
| 1 | Control | 0.0 | 0.0 | 0.0 | 0.0 | 6.7 | 6.7 | 3.3 | 3.3 | 0.0 | 0.0 | |
| Glaucoma | 0.0 | 0.0 | 0.0 | 7.7 | 46.1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||
| Cataract | 0.0 | 0.0 | 0.0 | 3.6 | 25.0 | 7.1 | 3.6 | 0.0 | 0.0 | 0.0 | ||
| AMD | 0.0 | 0.0 | 0.0 | 0.0 | 16.7 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||
| 2 | Control | 0.0 | 0.0 | 0.0 | 6.7 | 10.0 | 10.0 | 6.7 | 10.0 | 3.3 | 0.0 | |
| Glaucoma | 0.0 | 0.0 | 0.0 | 7.7 | 38.4 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||
| Cataract | 0.0 | 0.0 | 0.0 | 0.0 | 28.6 | 3.6 | 7.1 | 10.7 | 0.0 | 0.0 | ||
| AMD | 0.0 | 0.0 | 0.0 | 5.6 | 22.2 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||
| 3 | Control | 0.0 | 0.0 | 0.0 | 0.0 | 6.7 | 10.0 | 6.7 | 10.0 | 0.0 | 3.3 | |
| Glaucoma | 0.0 | 0.0 | 0.0 | 0.0 | 30.7 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||
| Cataract | 0.0 | 0.0 | 0.0 | 3.6 | 25.0 | 0.0 | 0.0 | 7.1 | 3.6 | 0.0 | ||
| AMD | 0.0 | 0.0 | 0.0 | 0.0 | 33.3 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||
| 4 | Control | 0.0 | 0.0 | 0.0 | 0.0 | 10.0 | 6.7 | 6.7 | 6.7 | 0.0 | 3.3 | |
| Glaucoma | 0.0 | 0.0 | 0.0 | 0.0 | 23.1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||
| Cataract | 0.0 | 0.0 | 0.0 | 7.1 | 32.1 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||
| AMD | 0.0 | 0.0 | 0.0 | 5.6 | 22.2 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | ||
AMD= age-related macular degeneration; CS= contrast sensitivity.
DISCUSSION
This study showed that the FVA CS test has good reliability, as shown by ICC and COR analysis. The CS test is useful for patients with good visual acuity who have healthy eyes without glaucoma, cataracts, or AMD. Although there are other commercially available CS tests using letters, symbols, or sine-wave gratings, these tests are not clearly standardized for performing a common CS evaluation such as visual field analyses(2,23). Sine-wave gratings permit sensitive testing of individual visual channels and are part of spatial frequency for evaluating CS function in vision science(12). The FACT chart also uses sine-wave gratings, which have been chosen at given luminance and glare levels for the ANSI by the United States Food and Drug Administration(5). Although the FACT chart is a modified version of the Vistech, it uses smaller increments (0.15 log units) and subjects must choose from three options. Previous CS studies with sine-wave gratings reported insufficient scores for reliability analyses (ICC 0.28-0.64 and COR 0.26-0.58)(2). Despite having poor reliability with FACT wall charts, closed systems using the standard FACT luminance and glare values were reported to exactly match the ANSI standards, thereby providing better reliability(3, 27). Hohberger et al.(27) reported average reliability coefficients of 0.80-0.96 for each cpd with an OPTEC 6500 CS test. Using the same device, Hong et al.(3) reported ICC 0.85 and COR 0.20, which are comparable to our results with the FVA closed system CS test (intersession ICC 0.86-0.94 and COR 0.16-0.19).
Previous studies with FACT charts in closed systems omitted any comparison with earlier and latter CS test scores that might have explained possible improvements in test reliability. We think that such comparisons are important to establish a reliable clinical application of the CS test. In this study, the mean ICCs of the closed system CS test were better at the second session (0.86-0.94) than the first session (0.69-0.90) in all groups. Furthermore, the CORs improved at the second session (first session 0.20-0.38; second session 0.16-0.24). There may be a learning effect, which possibly arises from cognitive abilities or getting familiar with the test procedure during the repeated tests. It has been reported that using letter charts for CS tests result in learning effects according to variable abilities to recognize letters. The FACT charts that use sine-wave gratings eliminate these problems(2,31). However, subjects high probability of correct guessing with the FACT charts, so repetitive tests are needed to reduce this effect(27,31). Subjects' responses may become more reliable after learning the FVA CS test procedure so it is important to conduct multiple CS tests to obtain more reliable clinical results.
It has been well documented that the spatial and temporal types of CS decrease in people with glaucoma(11,32,33). Grating CS tests are promising for the detection of early glaucoma and its progression(32,34). Klein et al.(17) suggested that spatial CS were a sensitive indicator of early glaucomatous loss in the presence of cataracts. Although visual acuity was good, the CS of the eyes with glaucoma was significantly less than among healthy subjects except at 1.5 cpd (p<0.012). This result was compatible with that previously reported by Onal et al.(7) using the FACT wall chart. The authors suggested that the FACT chart was useful for early diagnosis of patients with glaucoma, accompanied by a short-wavelength automated perimetry. This may be associated with early degeneration in the magnocellular ganglion cells, which are important for CS, in glaucoma(35).
The CS of eyes with AMD was worse than among healthy subjects at all frequencies (p<0.001), similar to previous studies(6,36). As there are limited options for treatment of AMD, early detection of the disease and prevention of progression are very important. Visual discomfort in performing daily activities often occurs in patients with AMD even though they have a BCVA of 0.00 logMAR on Snellen charts. This vision quality loss is seen in early AMD before any detectable retinal changes occur(18,37). CS reduction in AMD patients becomes more evident and uncomfortable under conditions of low illumination, which provides a low contrast environment(16).
It was reported previously that the closed system FACT chart had a lower ceiling effect than the wall chart test, which might increase its ability to detect small changes. In our study, no ceiling effect was observed in eyes with glaucoma or AMD using the FVA closed system CS test, and the ceiling effect was acceptable in healthy and cataract eyes(3). Even after a gap of at least one week between the first and second CS tests, the ceiling effect in normal and cataract eyes tended to decrease. These results suggest that the FACT chart in a closed system has the potential to detect small decreases in high CS scores in healthy, cataract, and AMD eyes and otherwise healthy eyes with early stages of glaucoma. A more pronounced floor-effect emerged in glaucoma and AMD eyes at higher frequencies, which may represent the effects of early retinal or ganglion cell defects on the loss of CS.
It is critical to know if the patients are affected by glaucoma, cataracts, or AMD in their daily lives when considering treatment options. CS has become more important for quality of life assessments, which have been receiving increase attention in recent years(37-39). CS is involved with differentiating low-contrast objects, such as human faces, and recognizing movement(37,40). Because of the close relationship between CS and the ability to perform activities of daily living, despite normal BCVA, CS testing is a useful clinical method to assess how ocular disease affects what patients can do. The present study found that FVA closed system CS evaluation provided reliable results with an easy method and standardized luminance.
It should be noted that there are several limitations of this study. The numbers of patients with eye disease and healthy controls were small. Reliability was evaluated by only two sessions with CS test each, so more sessions are required to strengthen the results. In addition, the interval between sessions varied from one week to one month.
CS measures visual quality and can provide detailed information by spatial frequency assessment. Thus, it can be used to detect early subclinical findings or changes during treatment for visual-system-related eye diseases. However, to differentiate healthy from abnormal characteristics and to detect real disease progression, the CS test must have strong clinical reliability. In this study, we found good reliability of the FVA closed system CS test in all groups and reliability improved during the second session. Therefore, to get more reliable results, repeated measurements are needed. Although, there was an acceptable floor-effect with the closed system test in patients with glaucoma and AMD, we found no ceiling effect; consequently, the view-in test has potential to detect fine changes at high frequencies.
In summary, to the best of our knowledge, this is the first study reporting the repeatability of FACT test scores using a closed system in patients with AMD and glaucoma. Hopefully, the reliability of this FACT will encourage clinicians to incorporate contrast sensitivity into their thorough evaluation of the early changes that accompany glaucoma, cataract, and AMD.





 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

