INTRODUCTION
The measurement of central corneal thickness plays an important role in the prognosis and treatment of many corneal diseases and glaucoma. It is also critical for refractive surgery management(1,2). Central corneal thickness (CCT) can be measured using an ultrasonic pachymeter (UP) or with specular microscopy, corneal topography screening, confocal microscopy, optical coherence tomography, and the Scheimpflug imaging method(3). Many modern contact and non-contact pachymetry measurement methods have been described; however, UP is still considered the gold standard(4).
In this study, we aimed to compare CCT of healthy individuals measured by UP and non-contact specular microscopy (NCSM) and to determine the average difference between the two measurements.
METHODS
We evaluated 148 eyes from 74 healthy subjects who consented to participation in this study. The study was conducted in the Şevket Yılmaz Training and Research Hospital between March, 2015 and June, 2015. Full ophthalmological examination was performed before measuring pachymetry. The patients with ocular diseases (corneal scar, cataract, glaucoma and keratoconus, or retinal disease), history of contact lens wear, dry eye, any systemic diseases, or a history of previous ocular surgery were excluded from the study. Patients with best-corrected visual acuity of 20/20 were included.
In order to avoid the potential effect of epithelial compression on consecutive measurements at the same location, CCT measurements were first taken via non-contact specular microscope NSP-9900 (Konan Medical, Inc., Hyogo, Japan). At the second stage of the study, CCT measurement was performed using an ultrasound pachymeter SP-100 (Tomey, Nagoya, Japan), which operates at 20 MHz, for measuring thicknesses in the range of 150 to 1200 μm with calibration at speeds ranging from 1400 to 2000 m/s(5). Topical anesthetic drops (0.5% proparacaine hydrochloride Alcaine®, Alcon) were instilled in all patients 1.5 to 2 minutes(6) before UP measurements.
NCSM and UP measurements were taken three times in the center of the cornea. For both measurements, average values were taken to compare pachymetry values.
All measurements were taken by one of the two authors (SGÇ or RD) in the afternoon, between 14:00 and 16:00 during a single visit. The study was planned and conducted in accordance with the Helsinki Declaration. A patient consent form was obtained from all participants.
Statistical analysis
Descriptive statistics included mean, standard deviation, minimum values, and maximum values. The distribution of the variables was measured with the Kolmogorov Simirnov test. In the analysis of the repeated measurements, a Wilcoxon test was used. A chi square test was utilized in the analysis of qualitative data. When chi square test conditions were not met a Fischer test was applied. Intra-class analysis was undertaken for correlation. The changes across measurements were assessed using Bland-Altman graphics. For the analyses, the SPSS 22.0 program was used.
RESULTS
One hundred and forty-eight eyes from 74 patients (36 (49%) males, 38 (51%) females) were assessed in this study. The mean age of participants was 45.2 ± 18.4 (12-85) years. The mean CCT measurement of all 148 eyes was 546.9 ± 40 μm with UP and 510.8 ± 42 μm with NCSM. Ultrasonic pachymetry and NCSM measurement results were around the equality line shown in figure 1. The mean CCT was 35 μm thicker in the UP group and the difference between groups was statistically significant (p<0.001).
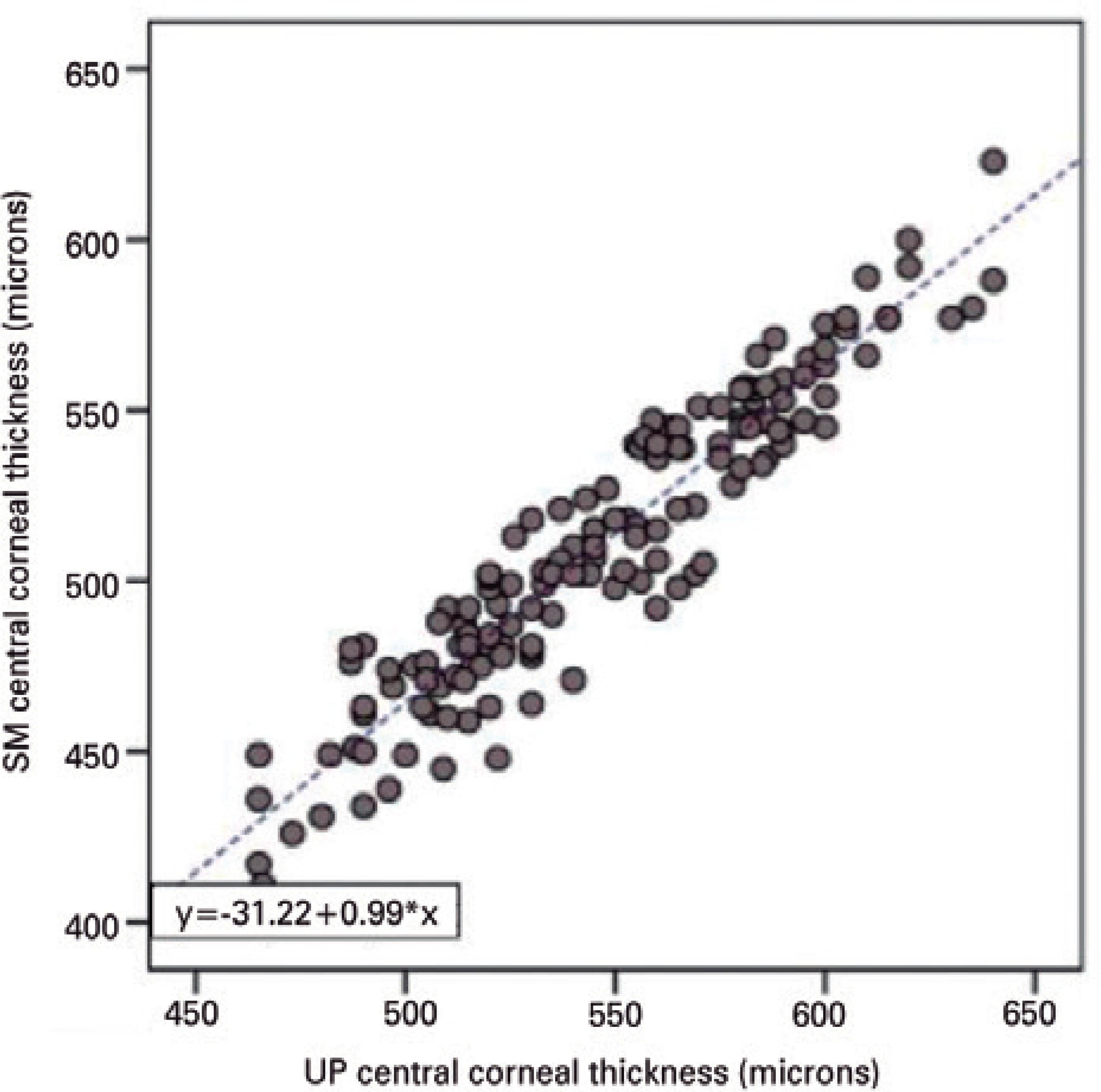
Figure 1 Scatter plots between central corneal thickness measurements (microns) acquired with non-contact specular microscope NCSM and ultrasound pachymetry (UP) showing a linear regression of y=31.22 + 0.99x.
Among the 148 eyes, corneal thickness measured with NCSM and UP devices showed significant and strong correlation (r=0.942/p<0.001). In all 148 eyes, the NCSM device measured corneal thickness as significantly (p<0.001) more thin than the UP device.
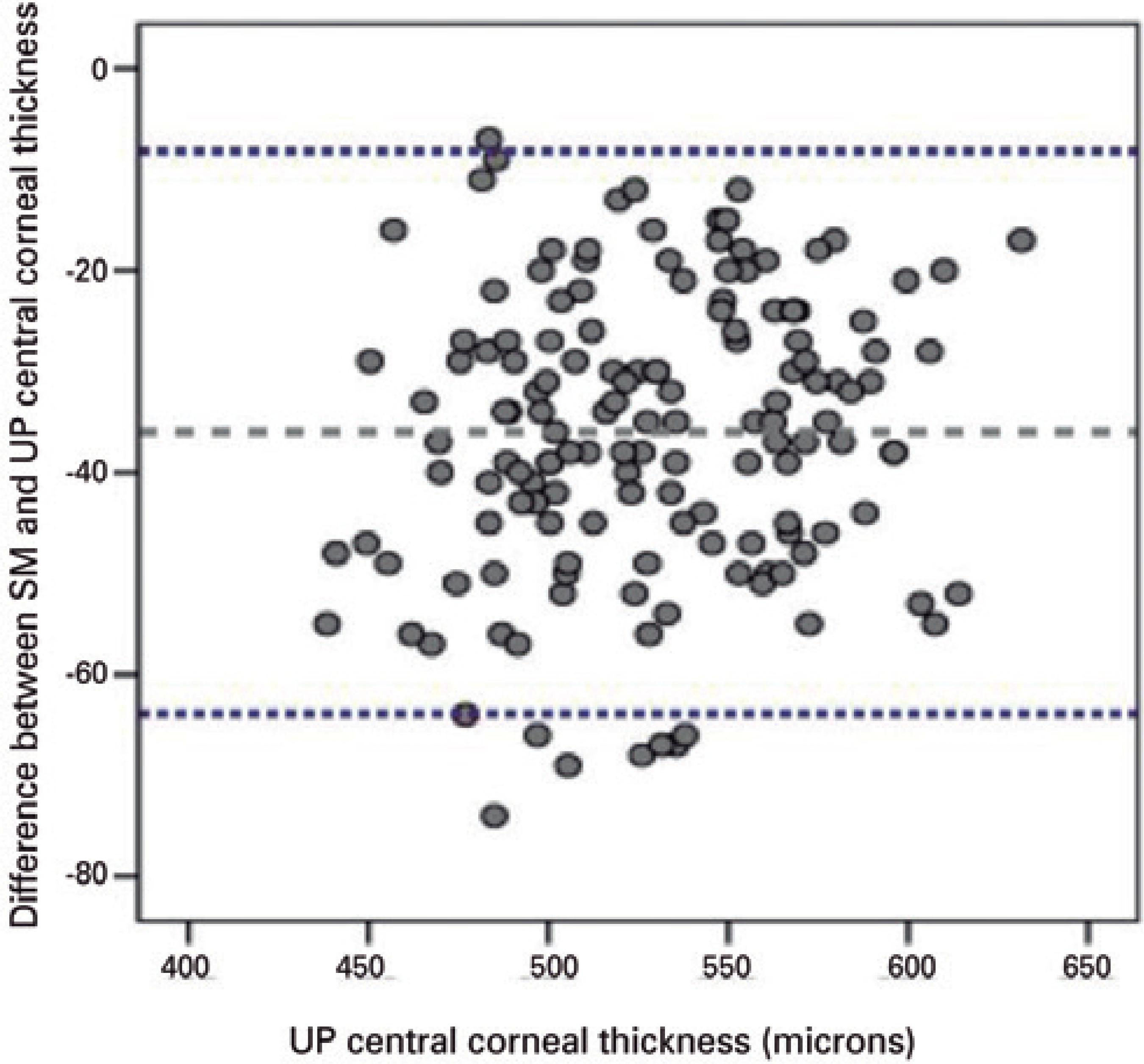
The equation, y=32.2 + 0.99x (R2=0.887), was attained via a regression model according to the CCT measurements with NCSM (x) and UP (y). The assumption that the values taken with the NCSM device will be 32 units lower than the UP per measurement has been proven to be a strong premise. Figure 2 presents the Bland-Altman plot demonstrating good agreement between the UP and NCSM methods for measurement of CCT.
DISCUSSION
CCT is a parameter that has a very wide range of applications for diagnosis and treatment of ocular diseases. In particular, when considering the clinical impact of the smallest changes in refractive surgery and glaucoma follow-up, the importance of measuring CCT in the most reliable way cannot be understated(1,4,7).
Although UP is the gold standard method, several non-contact measurement methods are sometimes preferred to ensure accurate measurement, need for contact with the cornea, and the capability to make measurements on multiple areas simultaneously(8,9). On the other hand, UP is currently the cheapest and most widely used method for CCT measurement. In this study, we compared UP, which only measures corneal thickness, and NCSM, which has the capacity to evaluate the endothelium and measure CCT at the same time.
There are many studies in the literature comparing CCT measurements methods and devices for normal corneas. Most of these studies reported that UP measurements were thicker than NCSM measurements(10-13). Modis et al. examined 73 eyes from 44 patients (mean age 66 years) with normal corneas comparing three different devices: NCSM (Topcon SP-2000P; Topcon Corporation, Tokyo, Japan), UP (AL-1000; Tomey, Erlangen, Germany), and contact specular microscope (CSM) (EM-1000; Tomey, Tokyo, Japan). The normal mean CCT was measured as 542 ± 46 μm with NCSM, 570 ± 42 μm with UP, and 638 ± 43 μm with CSM. The NCSM measurement was found to be significantly lower than the UP measurement(10). Al-Ageel and Al Muammar reported that CCT was significantly thinner when measured with specular microscope (SM) (511.9 ± 38.6) (SP-2000P, Topcon Corporation, Tokyo, Japan) than when measured with UP (533.3 ± 37.9) (SP-3000, Tomey Corporation, Nagoya, Japan) and that the two instruments were in good correlation while measuring 94 normal eyes of 47 patients, with a mean age of 33 years(12). In a multicenter study in Japan, both Orbscan and UP measurements were significantly higher than NSCM (SP-2000P, Topcon Corporation, Tokyo, Japan) measurements and ultrasonic pachymetry correlated with NCSM(13). In contrast, Khaja et al. reported lower values when comparing measurements made by UP vs. SM. The authors compared CCT measurements of 4 different devices in 32 healthy eyes of 32 subjects (mean age: 31 years). The authors compared, UP, slit-lamp optical coherence tomography (OCT), SM (Konan Medical Corporation, Fairlawn, NJ, USA), and Orbscan, and found that the mean CCT was 557 ± 49.92 μm on SM and 548 ± 48.68 μm on UP. However, they did not find this difference significant. This was in contrast with our findings, although it is possible that our studies limited sample size may have influenced our findings. It has also been reported that UP correlates with SM(14). Wu et al. measured the CCT of 322 eyes in 173 normal subjects using the Konan non-contact specular microscope to determine whether this method was reliable or not and was able to confirm this method's efficacy(15). Differences in measurement between UP and NCSM devices may be caused by the different working systems of each device. In cases of ultrasound pachymetry, the exact posterior corneal reflection point is not known; it may be located between the Descemet membrane and the anterior chamber(16). One other factor potentially influencing CCT measurement is tear film. Some authors have claimed that tear film thickness might be added into corneal thickness when non-contact optical devices measure CCT; however, tear film is compressed by the pachymeter probe when using UP(17-19). Reproducibility of the applications is also important, and some studies have shown that the reproducibility of the optical devices is high(20,21). However, with UP, it is difficult to maintain the same points and the perpendicularity of the ultrasound probe in sequential measurements.
Measuring corneal thickness remains a challenge for several devices and methods. In one study, De Bernado et al. using Topcon SP3000 specular microscopy, recorded thinner measurements than an Oculus Pentacam(22). In another study, the Pentacam and SP2000P Topcon NCSM were compared and the measurements obtained with the SP2000P were significantly smaller than those obtained with the Pentacam(19). Fujioka et al. compared the Pentacam with NCSM (Noncon Robo; Konan medical, Japan). Measurements taken with NCSM (552.04 ± 42.95 μm) were significantly smaller than those obtained with the Pentacam (559.49 ± 38.44 μm)(23). Other studies have measured CCT with the Konan NCSM; however, to the best of our knowledge this study examines the greatest number of healthy eyes while comparing CCT measurements for UP and NCSM.
In this study, one of the aims was to provide a regression formula to translate one measurement into another. We detected a strong and meaningful correlation between NCSM and the gold standard, UP. We found a difference of 32 units between measurements of the two devices, which may exist on the grounds of the change in possible reference points. We also think that a regression model can be used to convert the measurements of both devices and thus established the equation y=32.2 + 0.99x. This conversion may help assess patients who are referred to a clinic that uses a different measurement device (e.g., UP is used and NCSM measurements from other clinic have to be converted). However, this does not mean that these measurement methods are interchangeable. Bourges et al. reported that non-contact methods are reproducible and interchangeable with each other; however, interchangeability with UP has been found to be limited(21).
In conclusion, in this study we obtained thinner CCT measurements with NCSM compared to UP, widely regarded to be the gold standard. We think the differences between the devices is due to the different reference points these devices use for the measurements. In addition, the impact of the drops used for anesthesia and the reference points taken from the posterior cornea for the measurements could not be precisely explained.
These results confirm that SM measures significantly thinner corneas compared to UP. This could be due to the fact that the two machines measure different corneal points. This means that it is hard to estimate which of the two systems generates more accurate results in finding the closest value to the real value of CCT. The regression formulas given in this study could help more easily translate one measurement into another and this helps us to compare and evaluate CCT and intraocular pressure (IOP) from the former CCT and IOP history. As mentioned by Bourges et al.(21), we also believe that reproducibility and interchangeability in methods without contact to the cornea, in relation to ultrasound pachymetry, may allow for the non-contact devices to become gold standards for measuring CCT.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

