INTRODUCTION
Functional vision loss (FVL) is a condition in which the patient's subjective visual symptoms do not corroborate the results of a clinical examination and diagnostic workup(1). In general, FVL is a clinical diagnosis made when the physician demonstrates that the patient's visual acuity (VA) is better than alleged(2). The terminology associated with this condition varies considerably, and includes descriptors such as non-organic visual loss, psychogenic visual loss, malingering, hysterical visual loss, and ocular conversion reaction(1,3,4). Decreased VA, one of the most common functional complaints, may be either psychogenic or caused by malingering; with the former, subjects are unconscious of dissembling, whereas with the latter, subjects consciously dissemble the disease(5).
In order to distinguish between a potential psychogenic disorder and malingering, it is important to conduct a thorough search for evidence and establish a well-documented understanding of the patient's context(6). Malingering usually occurs when the patient seeks benefits associated with illness such as an evasion of criminal prosecution, escape from military service, compensation from social security agencies or insurance companies, and/or access to unnecessary free medications or medical equipment(7,8). In contrast, patients with psychogenic disorders tend to seek sympathy, family assistance, or social adjustment, and such cases usually present evidence of previous emotional trauma or stressful life events prior to the symptoms onset(7).
A comprehensive examination must be performed to rule out organic causes of vision loss(9). Measurement of visual function is a valuable step toward objectively explaining a patient's report of visual loss with no visible damage, and defending against subjective decision-making(10). The visual evoked potential (VEP) test has been used to evaluate functionality of the visual pathway, and the pattern-reversal (PR)-VEP has been used as an objective assessment of VA. Previous studies have used the PR-VEP to objectively assess the visual pathway by comparing the results achieved with normative amplitude and latency values(11).
The present study investigated the contributions of pattern-reversal transient VEPs to diagnose malingering in patients treated at a university hospital in Brazil.
METHODS
This retrospective study was performed in the Laboratory of Clinical Electrophysiology of Vision, Universidade Federal de São Paulo (UNIFESP), Hospital São Paulo, São Paulo, Brazil. This study's procedures complied with the tenets of the Declaration of Helsinki, and the study's protocol was approved by the UNIFESP Committee on Ethics in Research.
All participants were asked about their clinical histories, with an emphasis on the visual loss characteristics (e.g., bilateral or unilateral) and onset (e.g., sudden or progressive). In an attempt to gather detailed information about the motivation for FVL, questions were asked regarding medical leave from work, financial compensation for work accidents, and eventual use of medications for psychiatric disorders. The inclusion criteria were (1) unexplained visual loss according to findings from a previous ophthalmic exam (including visual acuity, refraction, biomicroscopy, intraocular pressure, direct and indirect fundoscopy evaluations) and (2) an age of ≥18 years. The exclusion criterion was the presence of neurological disorders that might affect VEP recording (e.g., epilepsy, intracranial tumor).
Procedures
Pattern-reversal visual evoked potential (PR-VEP)
Transient PR-VEP recording was performed according to the recommendations of the International Society for Clinical Electrophysiology of Vision (ISCEV)(12). PR-VEPs of each eye were obtained using electroencephalograph electrodes placed according to the 10-20 system. The active, reference, and ground electrodes were placed at Oz, Fpz, and Cz, respectively. Pattern-induced visual stimulation was provided by a pattern generator monitor with a mean luminance of 50 cd/m2. The reversal frequency of the frame-locked pattern was 1.9 Hz. At the viewing distance used in this study (100 cm), the display screen subtended angles of 17º x 17º at the eye. Black and white checks with visual subtenses of 15' and 60' were used as stimuli, and the spatial frequency in the 45º direction was calculated for both sizes of stimuli using a previously described formula(13). The spatial frequencies (cycles/degree) were 0.44 and 1.79 for larger and smaller checks, respectively. These spatial frequencies corresponded to checkerboard resolution visual acuity thresholds of approximately 20/1400 for larger checks and 20/300 for smaller checks. Because the resolution acuity thresholds could exceed the optotype acuity scores by up to 1 octave, the minimum visual acuity required to evoke responses to the larger and smaller checks would be 20/700 and 20/150, respectively. The contrast was set to maximum, and the luminance remained constant.
Occipital responses were averaged using the UTAS E-3000 system (LKC Technologies, Inc., Gaithersburg, MD, USA). The average response to 100 reversals was analyzed. Latencies (ms) of the major positive component (P100) and the negative peaks (N75 and N135) were determined for both stimuli. The P100 latency was compared with normal values obtained in our laboratory after setting the 97.5th percentile as the upper limit of normal(14). The Amplitude (μV) was defined as the difference in potential between the N75 and P100 peaks. For each eye and using the two checkerboard sizes, VEPs were classified as normal, reduced amplitude, prolonged latency, and non-recordable. Normal PR-VEP parameters (P100 latency and amplitude) for both stimulus sizes and in both eyes were indicative of malingering.
To improve accuracy and compliance, a direct observation of the examined eye was performed, during which the subject was continuously asked to pay attention to the center of the stimulus monitor. In addition, evaluations were performed by experienced examiners and the developing average waveform was carefully observed.
Visual acuity testing
The participants' best corrected visual acuity was measured using a retro-illuminated ETDRS Chart with Tumble "E" optotypes; glasses and pinhole correction were used when necessary. Each score was recorded as the 4-m logarithm of the minimum angle of resolution (logMAR) acuity.
RESULTS
The study subjects comprised 20 adults, including 11 (55%) women, with ages ranging from 21 to 61 years (mean= 45.05 ± 11.76 years; median= 49 years). The age distributions of men and women were similar; men's ages ranged from 21 to 58 years (mean= 44.44 ± 11.91 years; median= 49 years), and women's ages ranged from 30 to 61 years (mean= 45.54 ± 12.19 years; median= 49 years). A total of 39 eyes were tested (1 female subject had a right ocular prosthesis).
Figure 1 shows the distributions of individual PR-VEP parameters (P100 latency and amplitude) for 8 patients who met the criteria for malingering. The demographics, complaints of visual loss, informed optotype acuities, and motivations for FVL are listed in table 1. Informed optotype acuity ranged from no light perception (NLP) to 20/50. Previous ocular or head trauma was present in 3 cases. Two female patients had no apparent cause of malingering; these cases most likely involved psychogenic functional visual loss, and one patient (patient #4) was referred for psychiatric assessment.
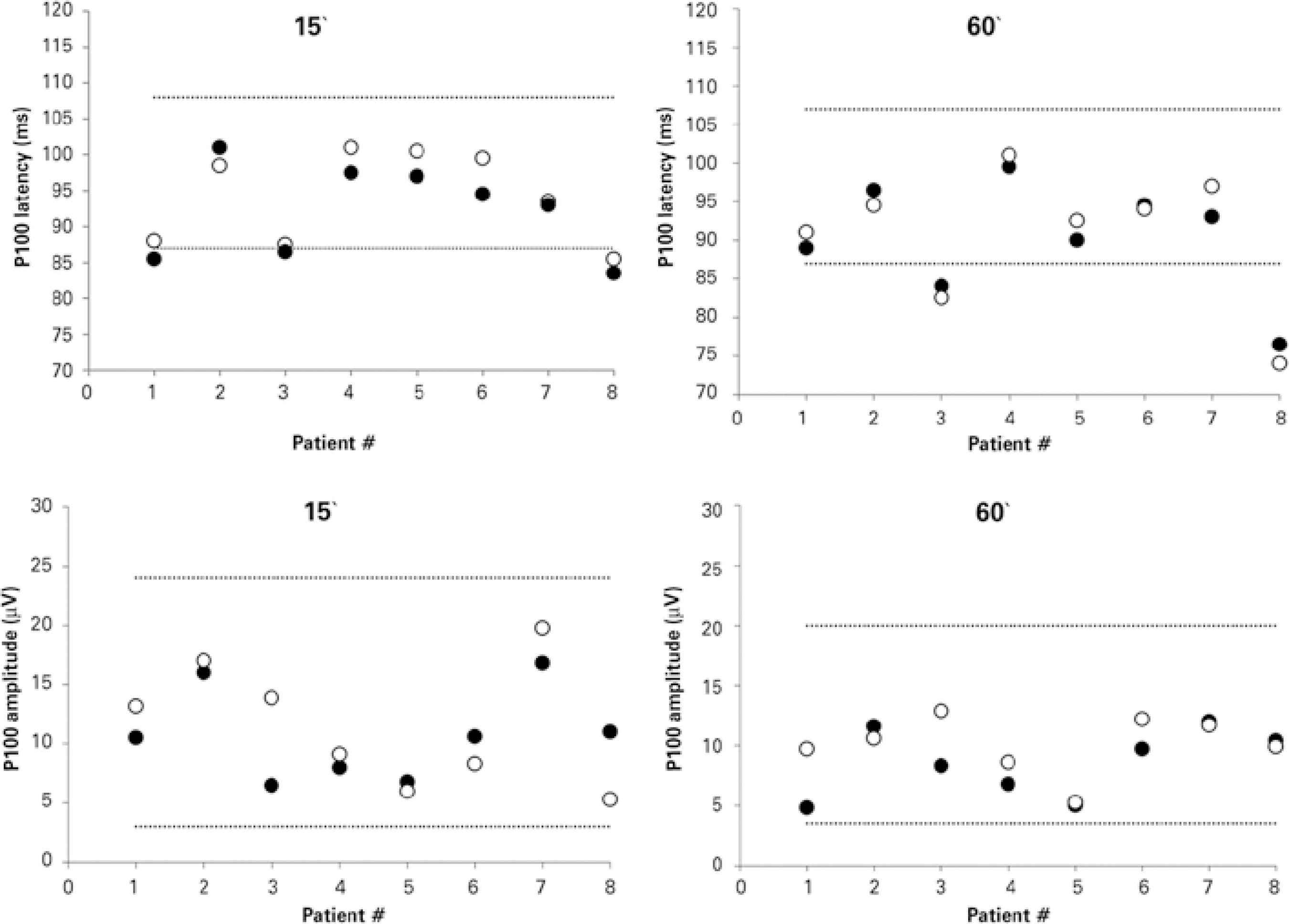
Figure 1 Transient pattern-reversal visual evoked potential parameters for check sizes of 15' and 60', demonstrating P100 latency (upper panels) and P100 amplitude (lower panels). Data were obtained from 8 patients with functional visual loss who were characterized as malingerers. Closed symbols represent right eye data; open symbols represent left eye data. Dotted lines indicate the lower and upper limits of normal as was determined in our own laboratory.
Table 1 Clinical characteristics of patients with malingering and normal VEP parameters in both eyes
| ID | Sex | Age (years) | Complaint of visual loss | Cause | VA RE | VA LE | Motivation |
|---|---|---|---|---|---|---|---|
| 1 | F | 33 | Binocular | None | HM | 20/160 | Psychogenic |
| 2 | M | 58 | Binocular | Corneal burn RE | 20/160 | 20/50 | Financial |
| 3 | F | 57 | Binocular | Bilateral diabetic retinopathy | HM | 20/125 | Financial |
| 4 | F | 36 | Binocular | None | 20/200 | NLP | Psychogenic |
| 5 | F | 56 | Right eye | Acute myocardial infarct | 20/160 | 20/125 | Financial |
| 6 | M | 32 | Left eye | Blunt trauma LE | 20/250 | CF | Financial |
| 7 | F | 60 | Binocular | None | 20/160 | 20/125 | Financial |
| 8 | F | 49 | Binocular | Head trauma with retinal detachment LE | 20/125 | 20/200 | Financial |
ID= identification; VA= visual acuity; F= female; M= male; RE=right eye; LE= left eye; HM= hand motion; NLP= no light perception; CF= counting fingers.
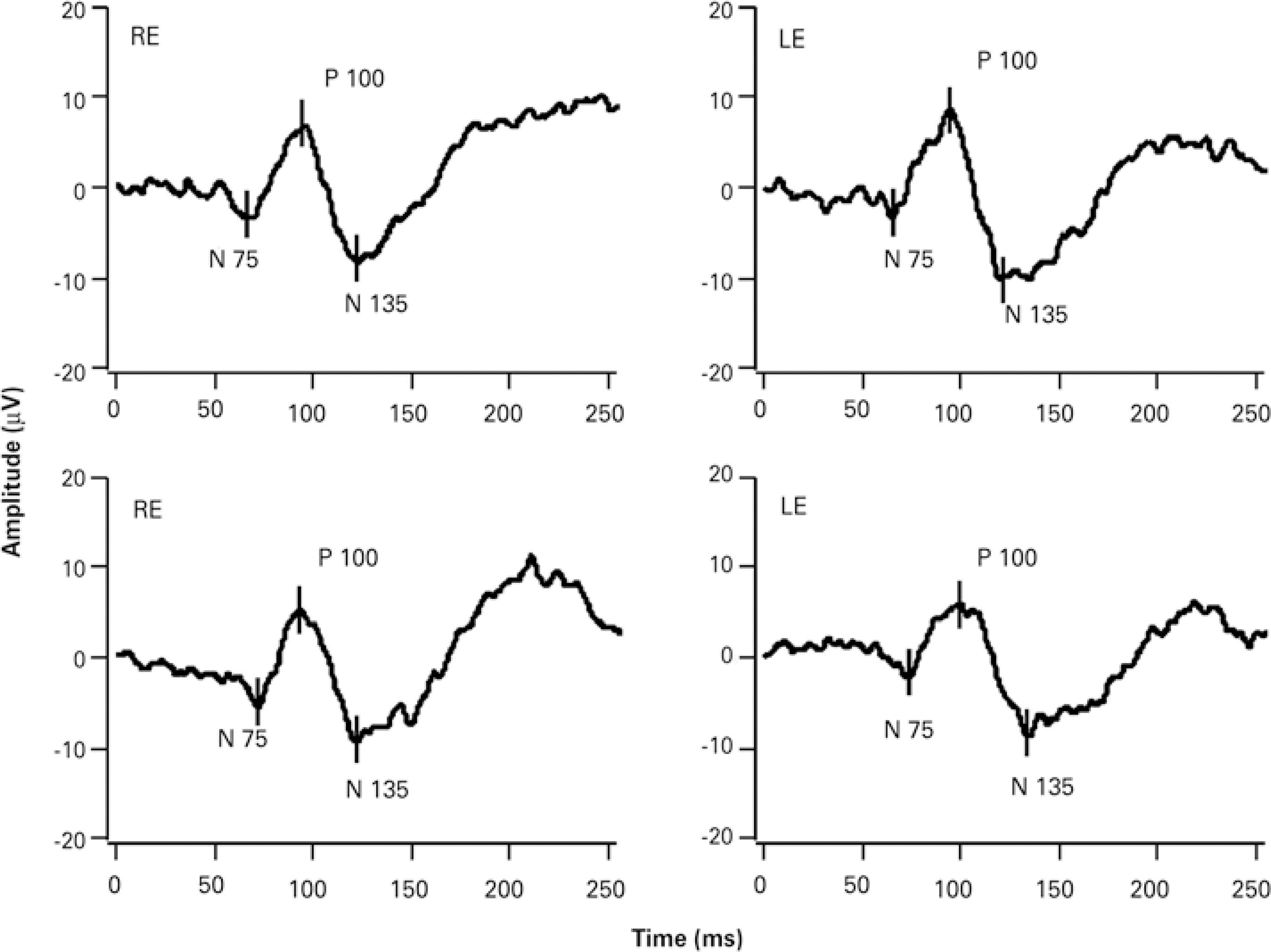
Twelve patients had an organic background for visual loss in 1 eye and complained of visual loss in the contralateral eye; accordingly, they were classified as exaggerators. Table 2 presents the demographics, visual loss complaints, informed optotype acuities, and motivations of this particular group. For these 12 patients, the individual parameters (P100 latency and amplitude) of the eye without an organic background for visual loss are shown in figure 2. All patients in this group had a financial motivation for their visual loss. Visual acuity in the malingering eye ranged from 20/63 to NLP. In 5 cases, ocular trauma was the organic cause that led to malingering of the contralateral eye in an attempt to achieve personal gains from social security agencies. Representative PR-VEP data from both eyes of a 32-y ear-old man with a subjective VA of 20/250 in the right eye and ability to count fingers with the left eye are presented in figure 3. The subject had experienced blunt trauma to his left eye and was suing his former employer for compensation benefits regarding his workplace injury.
Table 2 Clinical characteristics of 12 patients classified as exaggerators, with unilateral organic lesion: 9 malingering of the contralateral eye and 3 exaggerators of ipisilateral eye (patients 3, 7 and 9)
| ID | Sex | Age | VA RE | VA LE | Complaint | VEP RE | VEP LE | Motivation | Ocular findings |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 34 | NLP | 20/630 | Binocular | Non- detactable | Normal | Financial | Retinal atrophy post uveitis in RE |
| 2 | F | 34 | 20/320 | NLP | Binocular | Normal | Non-detectable | Financial | Infantile cataract in LE |
| 3 | F | 30 | 20/400 | 20/32 | Monocular | Normal | Normal | Financial | Penetrating ocular trauma in RE |
| 4 | F | 51 | Prosthesis | 20/63 | Monocular | N/A | Normal | Financial | Ocular prosthesis in RE |
| 5 | M | 37 | HM | LP | Binocular | Normal | Non-detectable | Financial | Macular scar post-chorioretinitis in LE |
| 6 | M | 52 | NLP | CF | Monocular | Non-detectable | Normal | Financial | RCVO in RE |
| 7 | M | 21 | NLP | 20/20 | Binocular | Normal | Normal | Financial | Penetrating ocular trauma in RE |
| 8 | M | 52 | NLP | 20/100 | Binocular | Non-detectable | Normal | Financial | Phthisis bulbi in RE |
| 9 | M | 48 | HM | 20/160 | Binocular | Non-detectable | Normal | Financial | Retinal detachment in LE |
| 10 | F | 61 | NLP | 20/400 | Binocular | Non-detectable | Normal | Financial | Penetrating ocular trauma in RE |
| 11 | M | 51 | NLP | 20/125 | Binocular | Non-detectable | Normal | Financial | Blunt ocular trauma in RE |
| 12 | M | 49 | NLP | 20/80 | Binocular | Non-detectable | Normal | Financial | Penetrating ocular trauma in RE |
ID= identification; VA= visual acuity; F= female; M= male; RE= right eye; LE= left eye; NLP= no light perception; HM= hand motion; LP= light perception; CF= counting fingers; VEP= visual evoked potential; N/A= non-applicable; RCVO= retinal central vein occlusion.
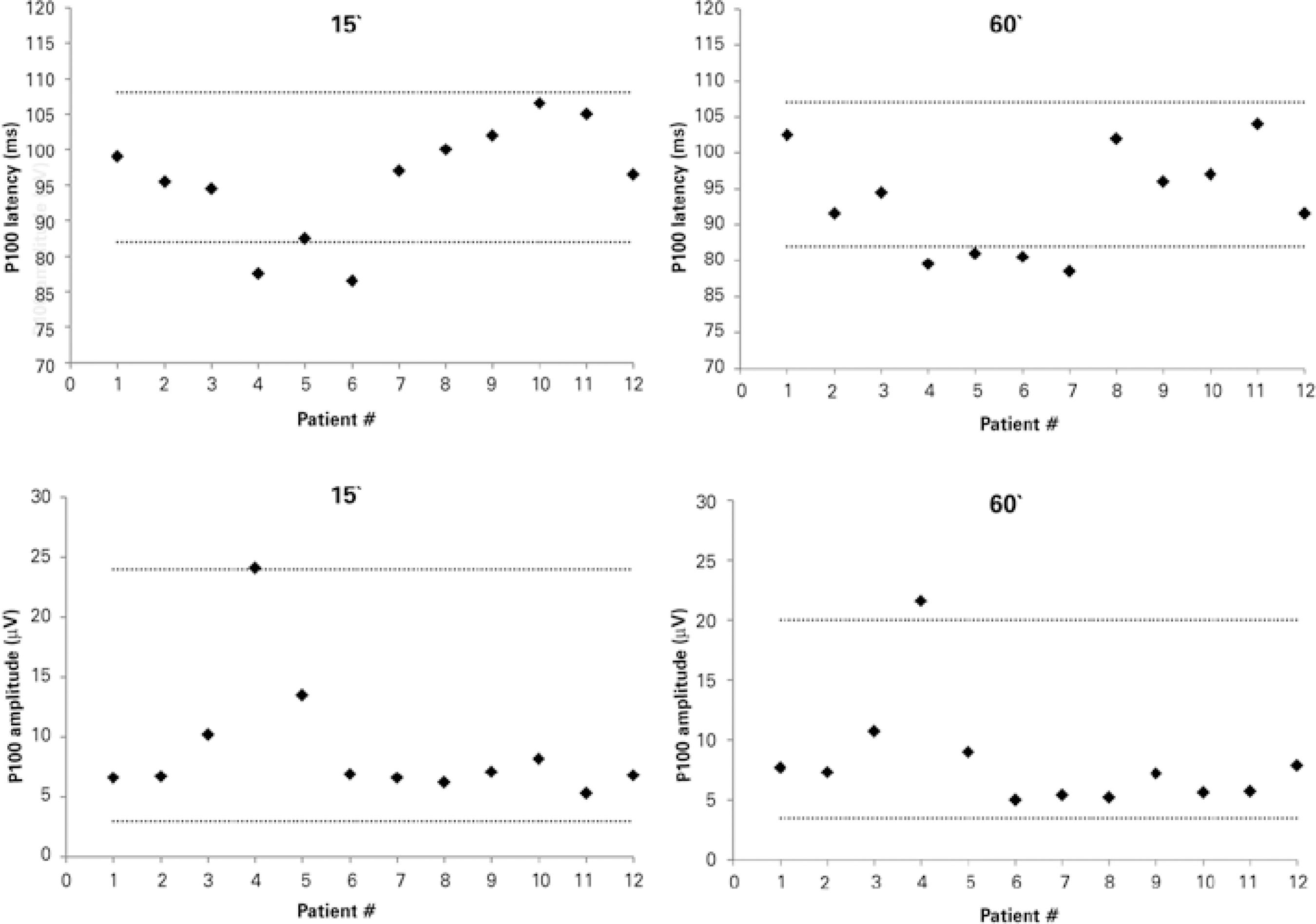
Figure 2 Transient pattern-reversal visual evoked potential parameters for check sizes of 15' and 60', demonstrating P100 latency (upper panels) and P100 amplitude (lower panels). Data obtained from 12 patients with functional visual loss who were characterized as malingerers and had one eye with an organic background. Data were obtained from the exaggerator eyes. Dotted lines indicate the lower and upper limits of normal as was determined in our own laboratory.
DISCUSSION
In this cohort of patients from a public hospital in Brazil, transient PR-VEP testing was found to be highly sensitive for the identification and diagnosis of pure malingering(5), as all eyes tested under the suspicion of malingering yielded normal PR-VEP amplitudes and latencies. A normal VEP result indicates a normal visual pathway with no organic cause of vision loss, and consequently, suggests malingering because of a specific motivation. It is important, however, to note that normal subjects might have employed changes in accommodation, a lack of attention, or meditation to consciously alter their VEPs to mimic significant visual or neurological lesions(5,15-18). For example, a patient might not focus on the center of the screen or might close his/her eyes too frequently. However, these artifacts were controlled through a careful observation of patient behavior during testing, as described in another report(19). In some cases, mainly those of patients who reported a lack of light perception, the use of flash VEPs might be considered to avoid the requirement for constant and steady eye fixation. However, flash VEPs are not sensitive to image blurring.
The majority of subjects in this study reported financial motivations for their reported ocular malingering (90%). As in previous studies, reliable PR-VEP data could be recorded in all patients with no observable physical damage to the anterior visual system who were included in the present study(9,20,21). An earlier study of 4 children with functional visual losses and normal PR-VEP results reported psychological and social motivations as the major reasons for malingering(22). PR-VEP testing assesses the integrity of visual stimulus conduction through the visual pathway, and a normal PR-VEP is thought to indicate pathway integrity; in addition, it is possible to infer whether the informed acuity is or is not reliable. However, mild losses in visual acuity should be interpreted in light of clinical findings from an ophthalmic exam that includes careful anamnesis and detailed semiology. Furthermore, patients with a true reduction in visual acuity might exhibit normal VEP responses and could therefore be considered false dissemblers.
If the results of conventional tests are equivocal or an objective assessment of the visual system functional integrity is required, VEP testing can offer a more direct assessment of visual pathway integrity, particularly in the context of a simulated severe visual acuity loss such as that of light perception. Although the current study was not designed to measure objective visual acuity using ISCEV transient VEPs, such measurements could be reliably achieved using the previously described sweep-VEP technique(23). This type of electrophysiological assessment allows patients with complaints of unexplained reduced visual acuity to verify their complaints, assess the degree of an underlying disorder, and attempt to localize the site of the defect within the visual system(24). PR-VEP might thus facilitate the detection or suspicion of malingering.
The major limitations of the present study were its retrospective design and its basis on a medical chart review; accordingly, the study lacked follow-up data that could confirm the subjects' malingering statuses. Furthermore, subject cooperation during the examination might have affected the PR-VEP outcomes. In this case series, many of the contributing factors associated with malingering, such as pre-existing trauma, physical illness, and pursuit of social benefits, were observed.
In conclusion, transient PR-VEP testing was found to be highly sensitive for the identification and diagnosis of pure malingering in a cohort of patients suspected of ocular malingering in a Brazilian hospital.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

