INTRODUCTION
Cataract surgery is the most common surgical procedure performed worldwide and has become increasingly reliable and reproducible since the addition of phacoemulsification. Only in the United States, two million procedures are annually performed due to an increase in early diagnoses and demands of patients who wish to maintain productivity and daily activities(1).
Multifocal intraocular lenses (IOLs) were introduced in the early 1980s and offer the benefit of promoting both near and distance vision simultaneously(2,4). However, after 30 years, adverse phenomena remain challenging, requiring careful patient selection since some patients could experience less clarity, decrease in contrast, and photopic phenomena when two images are overlapped(1,5-7). Moreover, the same optical quality cannot be expected as with a monofocal lens(3,6).
Several types of materials and technologies have been employed in designing IOLs, with refractive, diffractive, and hybrid models being the most widely used by surgeons. Moreover, asphericity was introduced as a means to compensate positive corneal spherical aberration(2,3). The addition promoted by the lens, whether it is +2.5 diopters (D), +3.0 D, or +4.0 D, influences the best reading distance and depth of focus. These different compositions culminate in distinctly different optical aberrometric behaviors(8-10).
In this study, we compared visual parameters, optical performance, contrast sensitivity (CS), and wavefront analysis results between two different types of multifocal lenses currently available in the market: AcrySof® IQ ReSTOR® Multifocal IOL SN6AD1 (Alcon Laboratories, Inc., Irvine, CA, USA) and AMO Tecnis® ZMB00 (Abbott Medical Optics, Santa Ana, CA, USA).
The AcrySof® IQ ReSTOR® Multifocal IOL SN6AD1 is a single piece lens composed of foldable hydrophobic acrylic, aspheric, adding a negative aberration of -0.20 µm to the human eye. With a refractive-diffractive hybrid design and apodized diffractive anterior surface, it shows a better near-distance visual acuity for smaller pupils and better long-distance visual acuity for larger pupils(11,12). It has a 3.6-mm diffractive optic zone, consisting of nine concentric rings that decrease from the center to the periphery (apodization), with a central ring of 0.856 mm and provides bifocality with a addition of 3 D, thus corresponding to 2.4 D in the lens plane(3,12).
The AMO Tecnis® ZMB00 lens is an evolution of the ZM900 IOL, which is constructed of a single piece of foldable hydrophobic acrylic material, with a diffractive posterior surface and aspheric anterior surface crafted to add a negative spherical aberration of -0.27 µm. It has 32 concentric rings, with a central ring of 1 mm and promotes an addition of 4 D, thus corresponding to 3.2 D in the lens plane, regardless of pupil size(6,11).
METHODS
This study was conducted in accordance with the ethical standards of clinical and surgical research and was approved by the ethics committee for Analysis of Research Projects (CAPPesq) of the Medical Staff of the Hospital Oftalmológico de Brasília and the Hospital das Forças Armadas, Brasília, Brazil. This prospective, non-randomized, comparative study included 74 eyes of 37 patients, selected from a list of cataract outpatients of the Hospital Oftalmológico de Brasília, who underwent cataract extraction with IOL implant between January 2011 and July 2013.
All surgeries were performed by the same surgeon (W.T.H.). The main incision was made in the steepest corneal meridian in three planes to encourage self-sealing. Continuous circular capsulorhexis and hydrodissection were performed and followed by viscoelastic soft-shell technique(10). Phacoemulsification was followed by irrigation and aspiration of the lenticular cortex and was concluded with implantation of one of the following lenses into the capsular bag: AcrySof® IQ ReSTOR® Multifocal IOL SN6AD1 or AMO Tecnis® ZMB00.
The inclusion criteria were (1) presence of a senile bilateral cataract, (2) interest in multifocal lens implant, (3) corneal astigmatism of ≤1.00 cylindrical diopter in both eyes, (4) pupil diameter of >3.0 mm under mesopic conditions, and (5) none of the following exclusionary factors: (a) existence of any other eye pathology or neuropathy that could decrease visual acuity, (b) CS or visual field sensitivity, (c) high axial myopia, (d) preoperative or postoperative complications, (e) concerns regarding an IOL implant inside the capsular bag, or (f) IOL decentration of >0.5 mm, as measured with a slit lamp.
We considered working and reading habits when choosing the lens for implantation. Patients with habits that demanded better intermediate vision were included in the IOL implantation group that aimed to achieve an addition of +3 D (SN6AD1). The remaining patients were included in the IOL group that aimed to achieve an addition of +4 D (ZMB00).
All patients underwent a complete ophthalmological evaluation on all visits, before and after surgery. Data from the 180-day visit of all patients were used for comparative analysis. Acuity of short-distance vision (33 cm) with and without refraction correction was measured using the reading table model of the Early Treatment Diabetic Retinopathy Study chart (ETDRS; Precision Vision, Ltd., Aurora, CO, USA). The same procedure was performed to test long-distance vision (4 m), although the chart was backlit to 100% contrast. All values were calculated according to the logMAR rating scale(13).
IOL dioptric power was calculated according to the optical interferometry technique using the IOLMaster® 500 Optical Biometer (Carl Zeiss, Jena, Germany), which sought emmetropia or the first positive value calculated by the following three formulas: Hoffer-Q for axial lengths of <22 mm, Holladay between 22 and 24.50 mm, and Sanders-Retzlaff-Kraff/T for axial lengths of >24.50 mm(14).
The postoperative scheme of medication (eye drops) was similar for all patients. The evaluation included the testing of monocular CS under photopic (with and without glare) and mesopic conditions using the Optec® 6500P Vision Screener (Stereo Optical Company, Inc., Chicago, IL USA) with spatial frequencies ranging between 1.5 and 18 cycles/degree and using the Functional Acuity Contrast Test chart provided by the manufacturer, which consists of columns that grow at different rates of 0.15 log units, which are then converted into base 10 logarithmic units for statistical analysis(2,15-20).
The same assessment was analyzed across the wavefront function, and the monocular optical aberrations were gathered using an OPD-Scan III aberrometer (Nidek Co., Ltd., Gamagori, Japan). Unlike other studies, we sought to evaluate aberrometry under conditions of mesopic pupil in an attempt to detect the manifestation of wavefront function under physiological conditions without the use of pharmacological mydriasis(13). The following variables were collected: (1) total aberration, (2) high-order spherical aberration, (3) tilt, (4) coma, and (5) Strehl ratio(8,9). Finally, the visual monocular defocus curve was evaluated in long-distance visual acuity, corrected using the same ETDRS chart at a distance of 4 m, at intervals of 0.50 spherical diopters from -5.00 to +2.50 D(21).
Significance was tested using the Tukey, Wilcoxon, Kruskal-Wallis, ANOVA, and chi-square tests by adjusting to a level of significance of 5% (p<0.05) and using SPSS for Windows statistical analysis software (IBM-SPSS, Inc., Chicago, IL, USA).
RESULTS
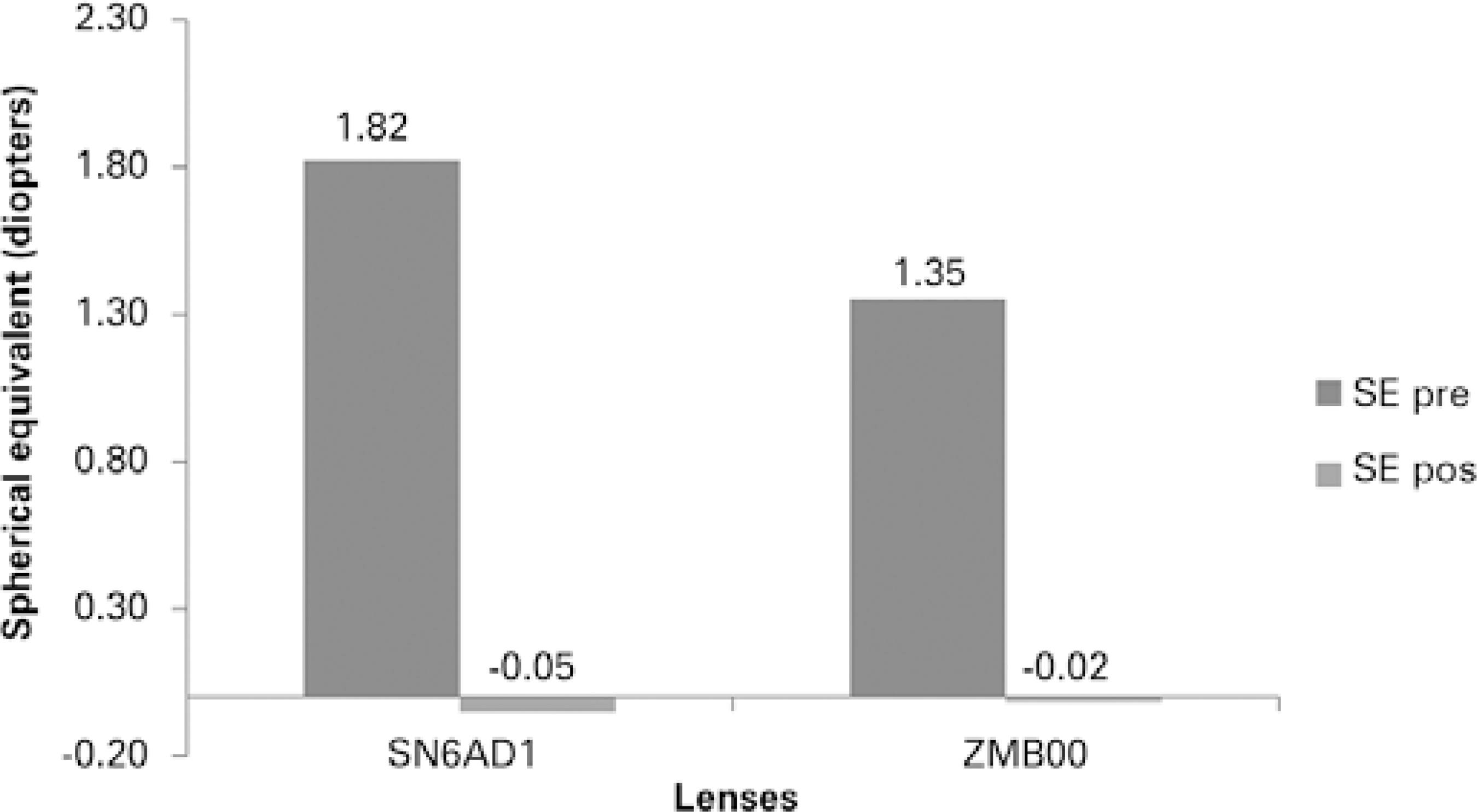
The study involved the participation of 37 subjects, 22 women (59.5%) and 15 men (40.5%), and a total of 74 eyes. There was homogeneity in the group distribution of lenses regarding to gender, age, axial length of the eye, and chosen diopter, as shown in table 1. The average preoperative spherical equivalence (SE) of all subjects was 1.58 D, and there was no relevant statistical difference between the groups (Table 1).
Table 1 Descriptive measures for age, implanted IOL refractive power (Diopters), axial length, preoperative spherical equivalent, preoperative and postoperative visual acuities for SN6AD1 and ZMB00 lenses
| 95% Confidence interval for mean | p-value between groups | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | Std. dev | Std. error | Lower bound | Upper bound | Max | Min | Student’s t-test | Mann-Whitney U test | ||
| Age | SN6AD1 | 34 | 62.12 | 5.48 | 0.94 | 60.21 | 64.03 | 51.00 | 72.00 | 0.184 | 0.170 |
| ZMB00 | 40 | 63.85 | 5.59 | 0.88 | 62.06 | 65.64 | 53.00 | 76.00 | |||
| Diopters | SN6AD1 | 34 | 22.26 | 3.20 | 0.55 | 21.15 | 23.38 | 17.50 | 31.00 | 0.969 | 0.521 |
| ZMB00 | 40 | 22.24 | 2.82 | 0.45 | 21.34 | 23.14 | 14.00 | 27.00 | |||
| AL | SN6AD1 | 34 | 23.16 | 1.00 | 0.17 | 22.81 | 23.51 | 20.60 | 24.75 | 0.197 | 0.533 |
| ZMB00 | 40 | 23.47 | 1.06 | 0.17 | 23.13 | 23.81 | 22.08 | 25.94 | |||
| preSE | SN6AD1 | 34 | 1.82 | 1.66 | 0.28 | 1.24 | 2.40 | -1.00 | 7.00 | 0.262 | 0.929 |
| ZMB00 | 40 | 1.35 | 1.90 | 0.30 | 0.74 | 1.96 | -4.00 | 4.00 | |||
| preUDVA | SN6AD1 | 34 | 0.26 | 0.45 | 0.08 | 0.11 | 0.42 | 0.00 | 1.00 | 0.058 | 0.081 |
| ZMB00 | 40 | 0.50 | 0.60 | 0.09 | 0.31 | 0.69 | 0.00 | 2.00 | |||
| postSE | SN6AD1 | 34 | -0.05 | 0.37 | 0,06 | -0.18 | 0.08 | -1.00 | 1.00 | 0.640 | 0.525 |
| ZMB00 | 40 | -0.02 | 0.28 | 0,04 | -0.11 | 0.07 | -0.50 | 0.75 | |||
| postUDVA | SN6AD1 | 34 | 0.09 | 0.09 | 0.02 | 0.06 | 0.13 | 0.00 | 0.40 | 0.601 | 0.677 |
| ZMB00 | 40 | 0.08 | 0.09 | 0.01 | 0.05 | 0.11 | 0.00 | 0.30 | |||
| postCDVA | SN6AD1 | 34 | 0.04 | 0.05 | 0.01 | 0.02 | 0.06 | 0.00 | 0.18 | 0.056 | 0.076 |
| ZMB00 | 40 | 0.02 | 0.04 | 0.01 | 0.01 | 0.03 | 0.00 | 0.10 | |||
| postDCNVA | SN6AD1 | 34 | 0.04 | 0.07 | 0.01 | 0.01 | 0.06 | 0.00 | 0.18 | 0.009 | 0.000 |
| ZMB00 | 40 | 0.09 | 0.09 | 0.01 | 0.06 | 0.11 | 0.00 | 0.30 | |||
| postDCIVA | SN6AD1 | 34 | 0.17 | 0.13 | 0.02 | 0.12 | 0.20 | 0.00 | 0.40 | 0.000 | 0.006 |
| ZMB00 | 40 | 0.54 | 0.13 | 0.02 | 0.50 | 0.60 | 0.20 | 0.80 | |||
AL= axial length; preSE= preoperative spherical equivalent; preUDVA= preoperative uncorrected distance visual acuity; postSE= postoperative spherical equivalent; postUDVA= postoperative uncorrected distance visual acuity; postCDVA= postoperative corrected distance visual acuity; postDCNVA= postoperative distance-corrected near visual acuity postoperative; postDCIVA= postoperative distance-corrected intermediate visual acuity.
Preoperative uncorrected distance visual acuity (UDVA) was better in the SN6AD1 group than in the ZMB00 group (0.62 vs. 0.50 logMAR, p=0.058), although this difference was not statistically significant (Table 1). There were no statistically significant differences in postoperative data of SE, UDVA, or corrected long-distance visual acuity (CDVA) between the groups (Table 1).
There was a statistically significant difference in pre- and postoperative SE and in pre- and postoperative UDVA between groups (Table 1).
Considering short-distance vision, there was a significant difference in the average short-distance visual acuity, as analyzed with correction for long-distance (DCNVA) between the SN6AD1 and ZMB00 groups (0.04 vs. 0.09 logMAR, p=0.009), and in intermediate vision (0.17 vs. 0.54 logMAR, p=0.000) (Table 1 and Figure 1). Preoperative and postoperative spherical equivalent (SE) results are demonstrated in figure 2.
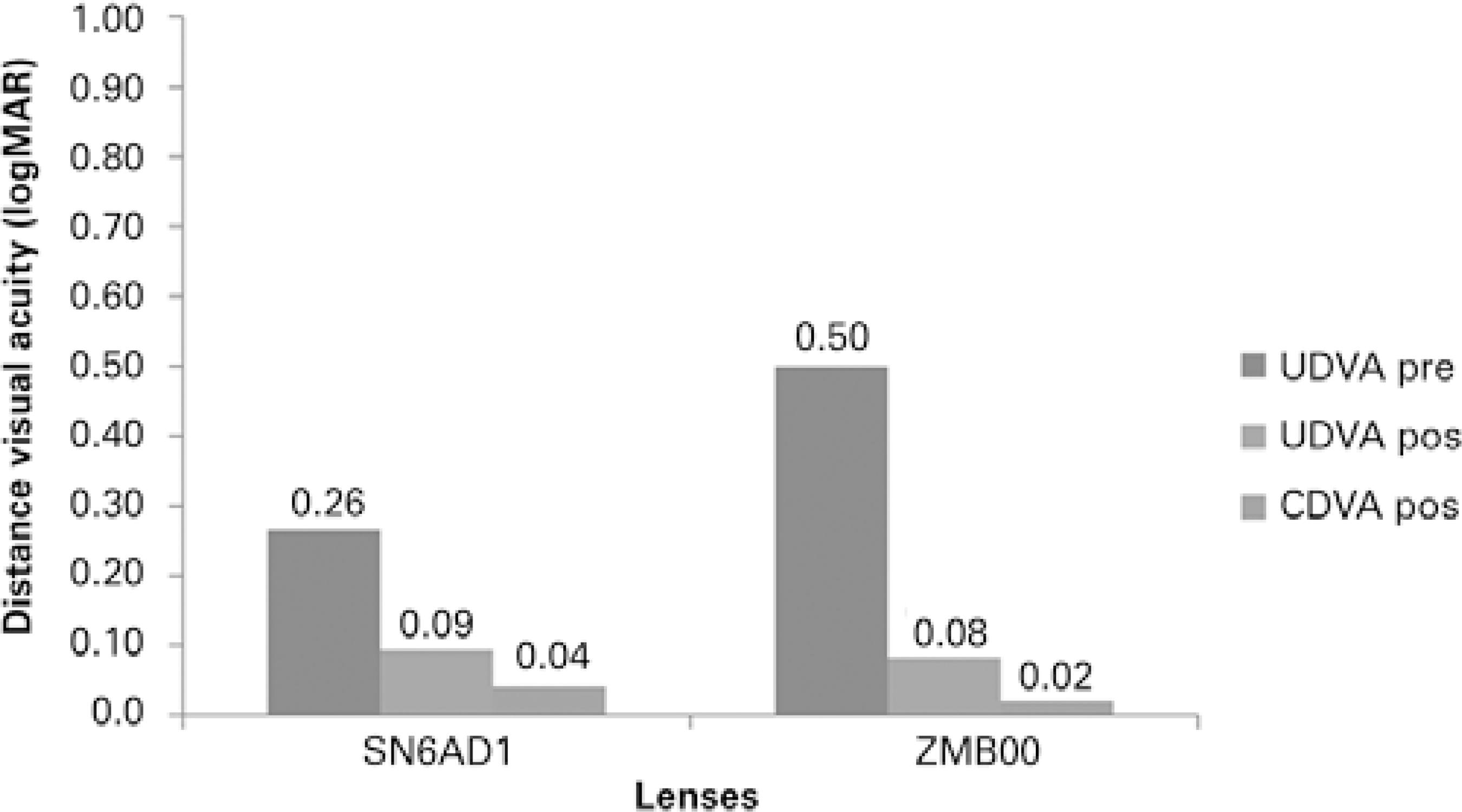
Figure 1 Preoperative long-distance visual acuity without (UDVA) correction, versus post-operative UDVA versus postoperative visual acuity for long-distance with (CDVA) correction for SN6AD1 and ZMB00 lenses.
None of the patients required any type of short- or long-distance correction in their everyday life following surgery.
CS under photopic conditions without glare was better at a low frequency (1.5 cpd) for the SN6AD1 lens (p=0.039) and at a high frequency (18 cpd) for the ZMB00 lens (p=0.62). Under photopic conditions with glare, the ZMB00 lens performed better at high frequencies (18 cpd) with p = 0.003. Under mesopic conditions, the lenses exhibited similar behavior (p>0.05) (Figures 3, 4, and 5).
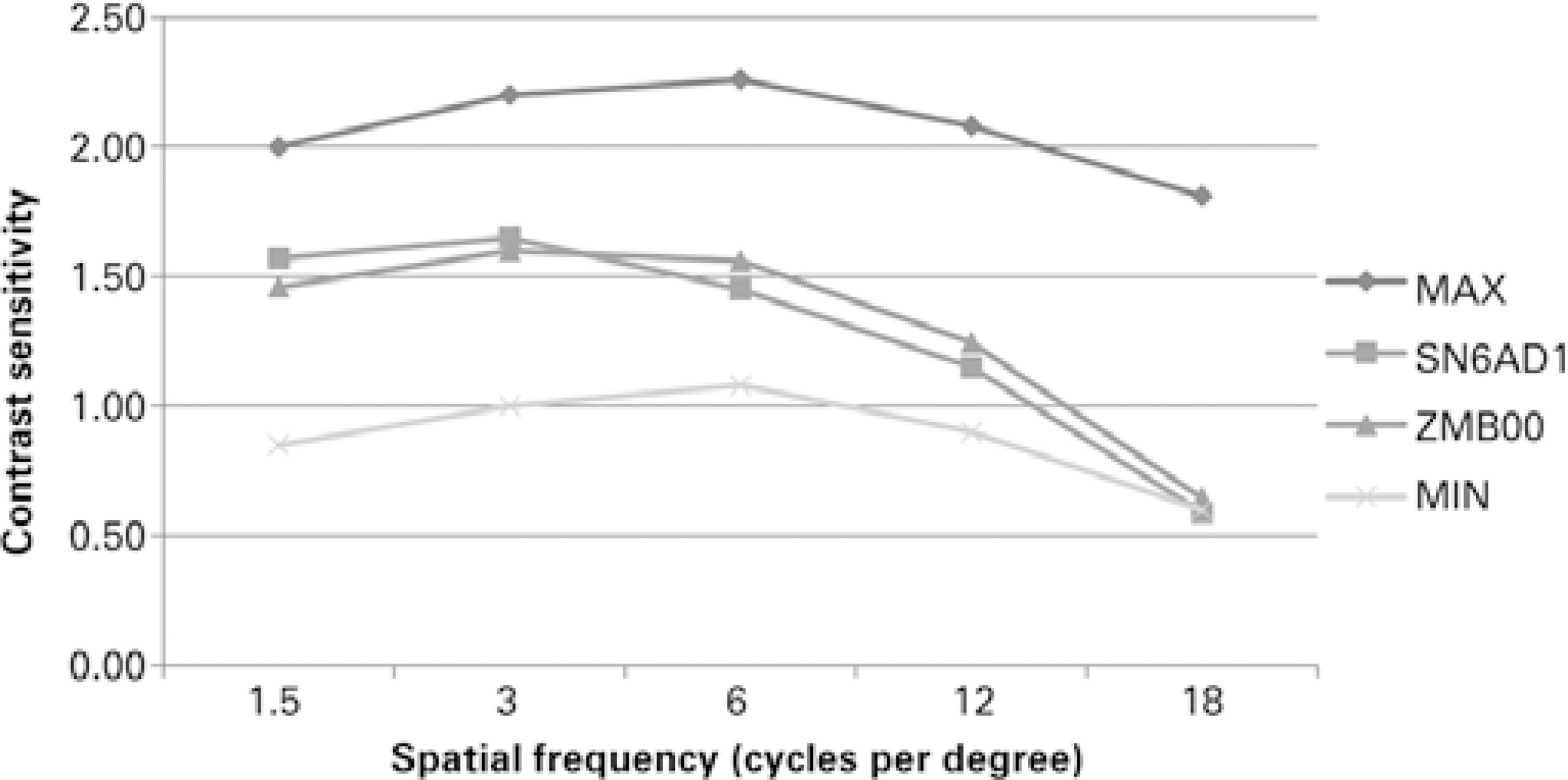
Figure 3 Comparison for the SN6AD1 and ZMB00 lenses with respect to the photopic situation without glare.
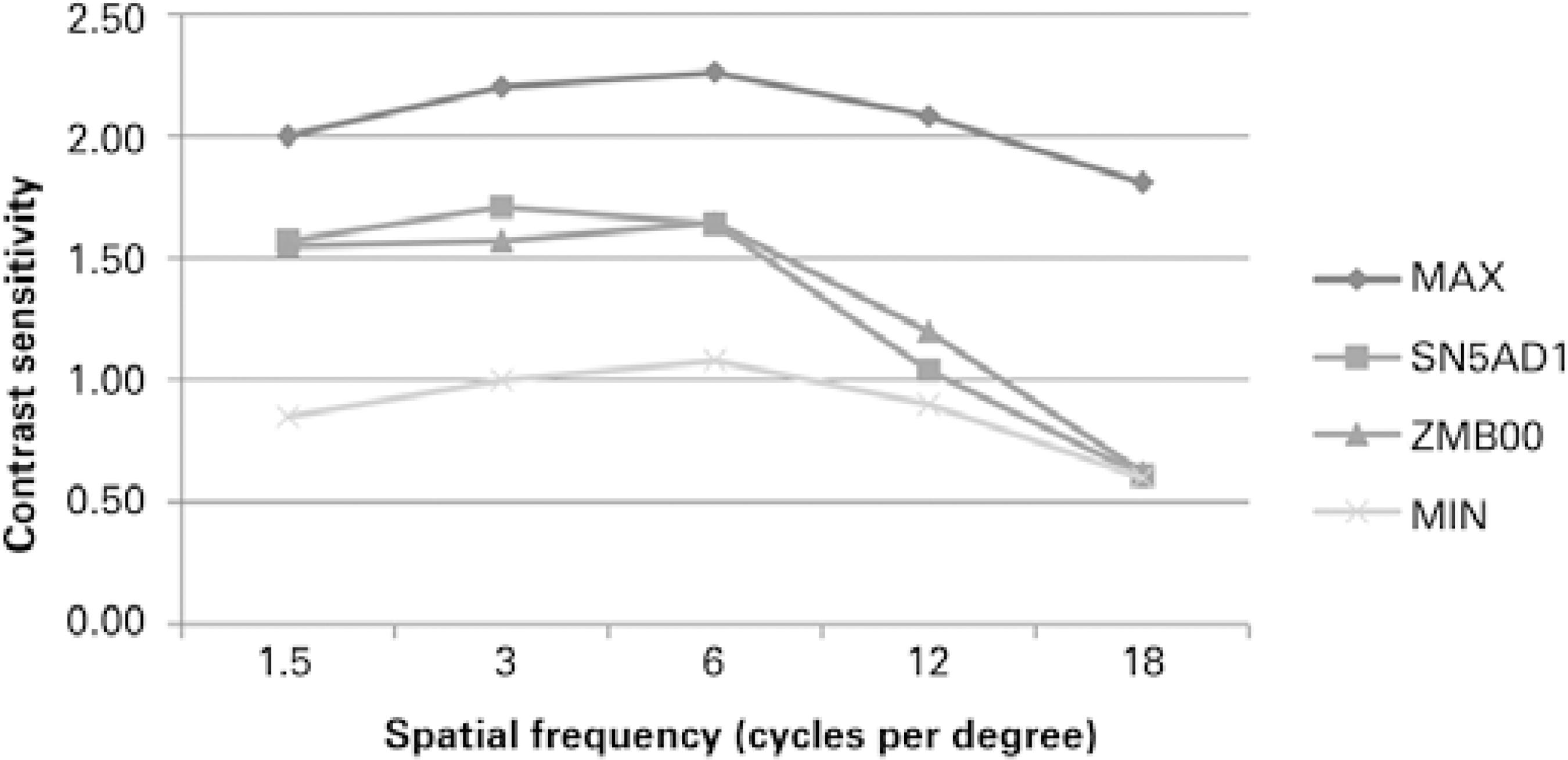
Figure 4 Comparison for the SN6AD1 lenses and the ZMB00, with respect to the photopic with glare situation.
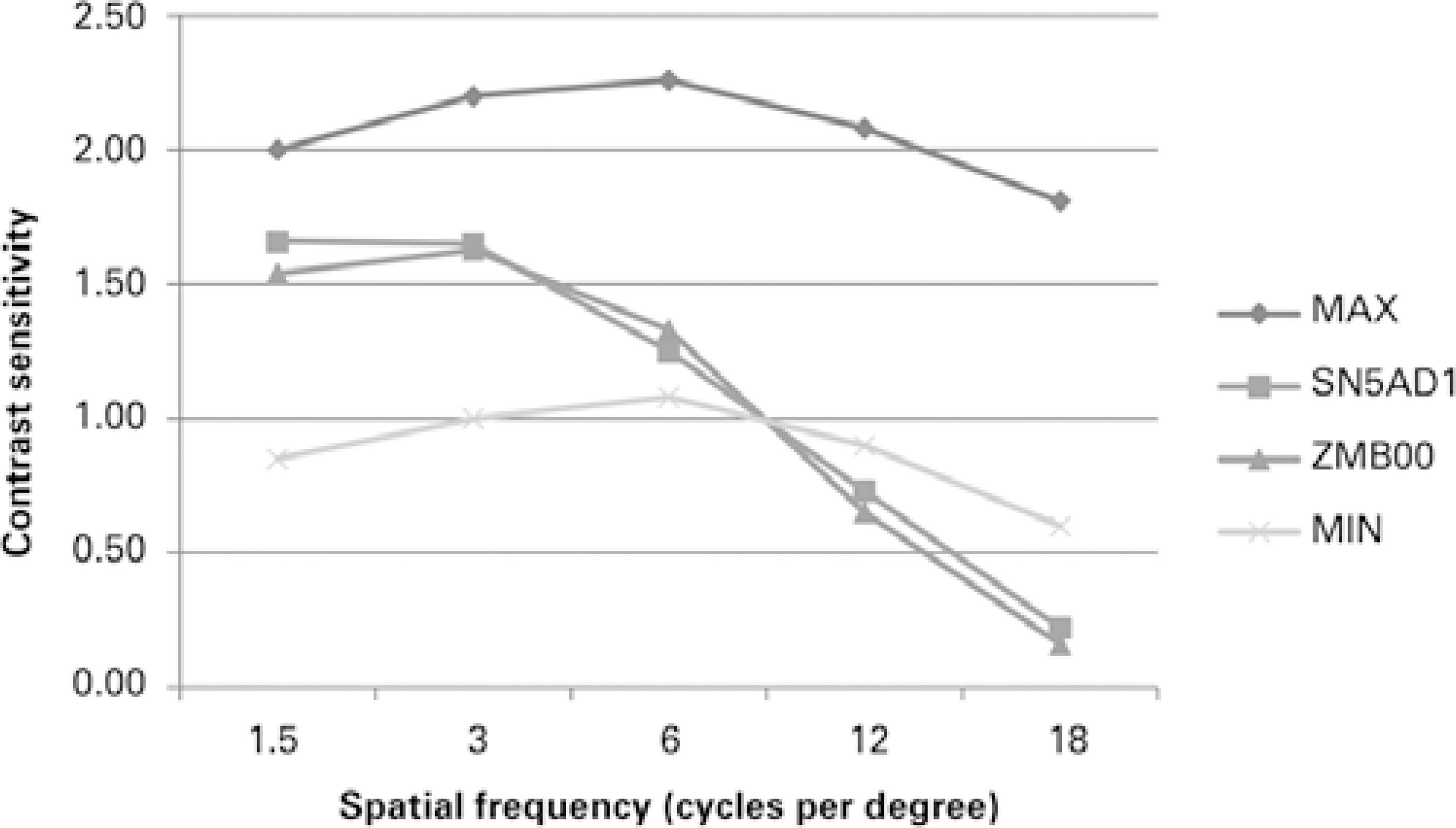
Figure 5 Comparison for the SN6AD1 lenses and the ZMB00 lenses with respect to the mesopic with glare situation.
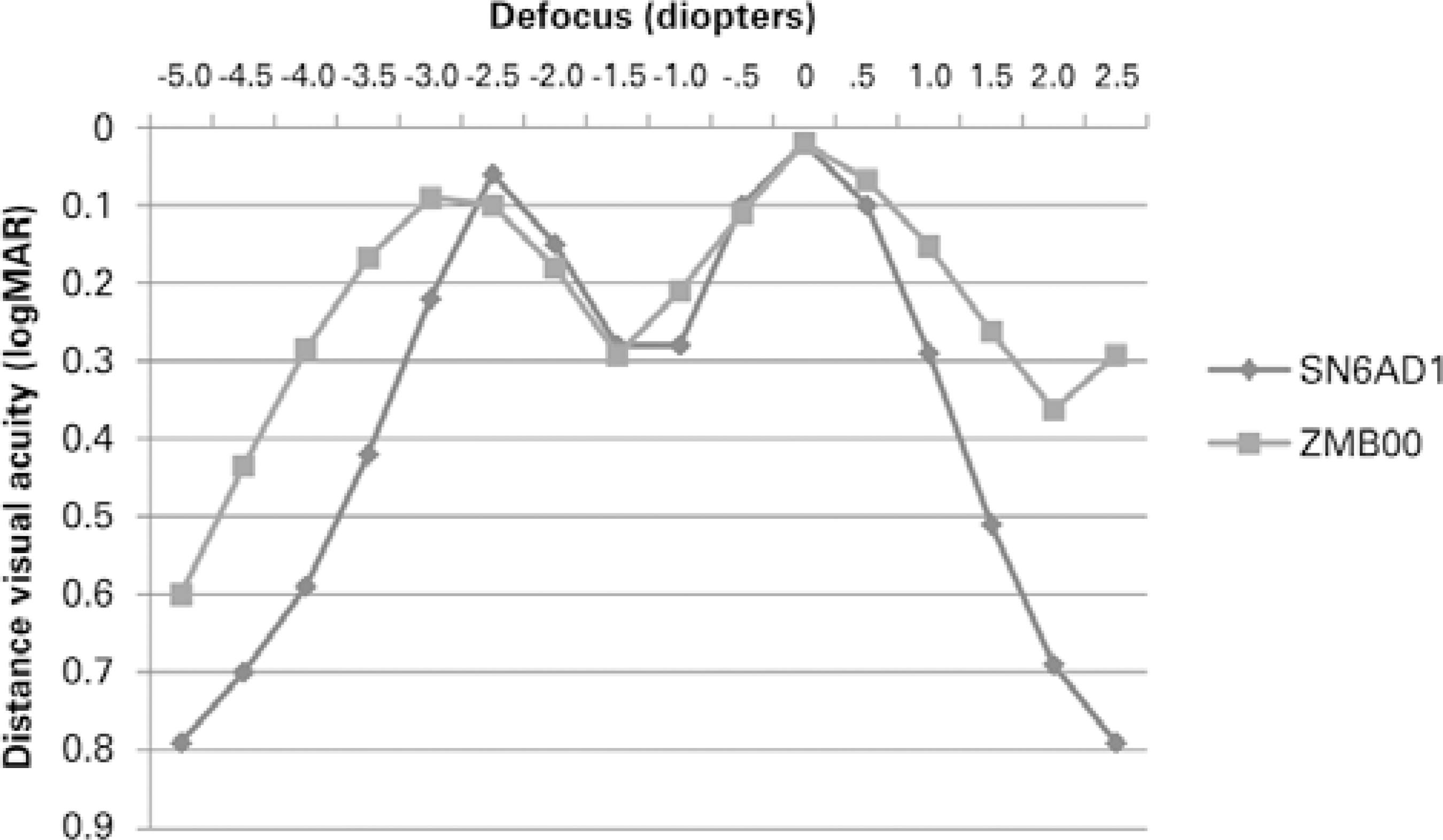
Regarding defocus curve, there was a difference in almost all of the distances assessed between lenses (converted into diopters, p<0.001). The ZMB00 lens showed peaks close to -3.0 D (33 cm) and 0.0 D, with an average visual acuity of 0.09 and 0.02 logMAR, respectively. The line corresponds to the SN6AD1 lens and showed peaks at -2.5 D (40 cm) and 0.0 D, with visual acuity of 0.06 and 0.02 logMAR, respectively. Regarding intermediate deflection vision, both occurred at -1.5 D (66 cm), with a visual acuity of 0.28 and 0.29 logMAR, respectively, but with no statistically significant difference from this point (p=0.68) to -2.5 D (40 cm) (p=0.12) (Figure 6).
Wavefront analysis demonstrated that, in absolute values, the ZMB00 lens showed better results in the decomposition of the wavefront function; however, there was no statistically significant difference between groups (p>0.05) (Table 2).
Table 2 Comparison of wavefront function analysis between SN6AD1 and ZMB00
| SN6AD1 | ZMB00 | p-value | ||
|---|---|---|---|---|
| Mean | Mean | Student’s t test | Mann-Whitney U test | |
| Total | 0.775 | 0.742 | 0.784 | 0.793 |
| Tilt | 0.338 | 0.288 | 0.554 | 0.734 |
| HOA | 0.408 | 0.328 | 0.231 | 0.156 |
| Coma | 0.161 | 0.149 | 0.785 | 0.422 |
| Sph | 0.105 | 0.077 | 0.400 | 0.107 |
| Strehl ratio | 0.048 | 0.052 | 0.663 | 0.459 |
HOA= high order aberrations; Sph= spherical aberration.
DISCUSSION
The analysis of groups distribution demonstrates homogeneity and enables comparisons between groups, indicating its suitability for comparison to other publications(7,10,21-24).
As demonstrated in other studies, the good quality of distance and near vision was attested through both types of lenses, regardless of which addition had been used. The improvement in UDVA, in addition to the excellent individual results, for both long and short distance confirmed the efficacy of the treatment and provided independence from glasses(1-3,6,12,13,17,21-23,25). Such inference is particularly evident when considering postoperative SE.
Analysis of DCNVA highlighted advantages of the SN6AD1 lens (p<0.05). However, when converting the Jaeger table visual scale to logMAR, values that transcend the understanding of the different visual levels for short distances may appear. Given that J1 corresponds to 0.00 logMAR and at the level immediately below, J2 corresponds to 0.1 logMAR, both groups presented average DCNVA level at J1 and better than J2(11).
Considering CS under photopic conditions, the ZMB00 lens showed better results at high spatial frequencies (p<0.05). Low spatial frequencies are associated with the perception of motion (magnocellular pathway), whereas high frequencies are associated with the perception of detail (parvocellular pathway)(26). Hida et al. compared the SN60D3 IOL to the ZM900 IOL and found similar results applicable to this study since SN6AD1 and ZMB00 lenses are the evolution of the SN60D3 and ZM900 IOLs(13). Cillino et al. compared the visual CSs of SN6AD1, SN6AD3, and ZMA00 lenses and found no statistical difference among the three groups. However, the study was performed using the Pelli-Robson method to evaluate CS, which has a greater chance of being influenced by the environment, unlike the automated method(11). Afonso et al. found similar values for the SN6AD1 lens, as did de Vries et al. for average values at high frequencies (1.13 at 12 cpd and 0.65 at 18 cpd)(2,12).
The differences in Mesopic CS were not significant when comparing the two groups at any spatial frequency. This finding was consistent with those in other publications(2,12,13,22).
It must be considered that under photopic and mesopic conditions, the two groups showed averages below their corresponding monofocal IOLs peers, as described in other studies. Considering CS, ZA9003 IOL has been considered better than the ZMA00 IOL(10,22,23). Nakano et al. and Vingolo et al. concluded the same by comparing SN60WF and SA60AT IOLs with SN60D3 and ZM900 IOLs(27,28). This phenomenon could be explained through the analysis of the concept of multifocality promoted by these kind of lenses by splitting light energy into two foci and overlapping near and far images.
Afonso et al. correlated greater pupil diameters to better CS at all frequencies under photopic and mesopic conditions(20). This idea seems plausible because a larger amount of light enters the optical system, which is proportional to the increase in pupil diameter. In our study, we did not perform analysis of any such correlation.
Considering visual defocus curve, it was clear that both groups reached two peaks of improved visual acuity corresponding to near and far distances. Considering near vision, significantly better vision was found close to 33 cm with the ZMB00 lens than with the SN6AD1 at this point, although the SN6AD1 lens demonstrated greater near vision at a 40-cm reading distance, but with no statistical significance when compared with the ZMB00 lens at this focus point. This is a different result from what was found at the near visual acuity test and may be related to pupillary function that improves the near visual acuity for refractive-diffractive hybrid design lenses.
When assessing intermediate vision of 66 cm, the two groups showed similar low performances when compared with the peak curve points of better vision. Schmickler et al. reached similar values when individually assessing the ZMB00 lens(6). Similarly, Afonso et al., de Vries et al., and Petermeier et al. depicted the same defocus curve pattern for the SN6AD1 lens(2,12,21).
Nevertheless, analysis of the two IOL defocus patterns suggests that there should be a relative permanence of the curve near the better vision peaks, which indicates a reasonable depth of focus around these two top focal points. To be more specific, the reading distance might not be confined only to certain near distance, and it would have an amplitude of approximately 12 cm in diameter around the best near focal point. Although it seems little, it may make a difference for better adaptation of patients with more intermediate visual habits.
Regarding the results of aberrometry, both lenses were successful in decreasing corneal positive spherical aberration. However, self-criticism is necessary to evaluate the method employed. Because a multifocal lens simultaneously generates two distinct wavefronts, it may be difficult to achieve separate and accurate measurements with a particular device. Nevertheless, it is understood that the same difficulty in measurement was imposed upon both groups, making comparisons reasonable. Hida et al. compared the ZM900 and SN60D3 lenses and found similar aberrometric results, as did Nakano et al.(10,27). Moreno et al. evaluated a system for analyzing the wavefront of a double-passage Optical Quality Analysis System (Visiometrics, S.L., Cerdanyola, BCN, Spain) that could differentiate the two wavefronts and thereby assess the optical quality more accurately for better differentiation(29).
It is important to emphasize the Strehl ratio variable. This value corresponds to the ratio between the peak of the measured point spread function (PSF) and a PSF peak in an aberration-free optical system. Values range from 0 to 1, where 1 represents an ideal optical system. The value usually decreases as the pupil increases, expanding the influence of optical aberrations that compromise quality. Larger or smaller values for similar pupil conditions correspond to better or worse visual quality(9). Our results suggested equivalence between the two lenses. Artigas et al., compared the SN60D3 and ZM900 lenses and suggested better results for the SN60D3 lens, using an artificial eye as model(30).
In conclusion, the two lenses were effective in enabling better vision for both long and short distances, although neither exhibited excellent visual acuity on intermediate vision, despite this equivalence. Both groups had a reasonable range of focus around the two best focus points (near and far). The ZMB00 lens recorded better results in CS under photopic conditions at high frequencies, although both lenses demonstrated inferior results when compared to their monofocal peers described in past publications. The ZMB00 and SN6AD1 lenses are equivalent with regards to wavefront function, although more studies are needed to better assess aberrometry.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

