INTRODUCTION
Posterior scleritis is an ocular inflammatory disorder that is predominantly idiopathic, autoimmune, or rarely, infective(1,2). Anterior and posterior scleritis due to Mycobacterium tuberculosis are rare but have been reported in the literature(3); however, to our knowledge, isolated posterior scleritis associated with tuberculosis (TB) has only been described twice(1,4).
We report a patient with posterior scleritis associated with latent TB without associated uveitis, anterior scleritis, keratitis, or any other previous ocular disease history.
CASE REPORT
A previously healthy 43-year-old woman presented with complaints of painful reduced visual acuity and periorbital edema in her left eye of 4 days' duration. Ophthalmological examination showed best corrected visual acuity (BCVA) in the right and left eyes of 6/6 and 6/60, respectively, and left eye proptosis, with no conjunctival or ciliary hyperemia and no anterior chamber reaction. Fundoscopy was unremarkable in the right eye, while the left eye showed choroidal folds, optic disc edema, and exudative inferior retinal detachment.
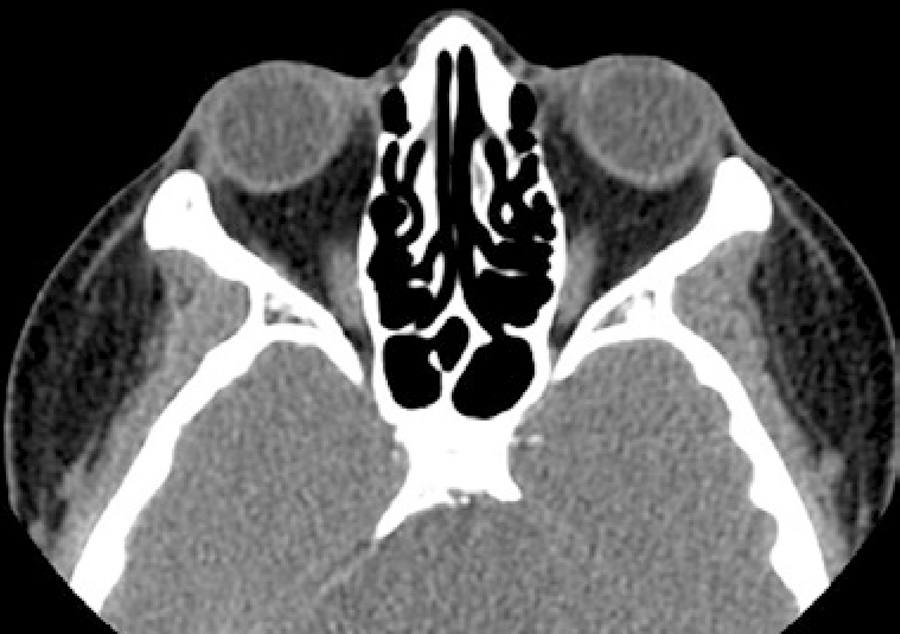
Orbital computerized tomography (CT) scan and magnetic resonance imaging revealed a left eye choroidal and transscleral mass spreading to the Tenon's space, along with thickening of the optic papilla (Figure 1).
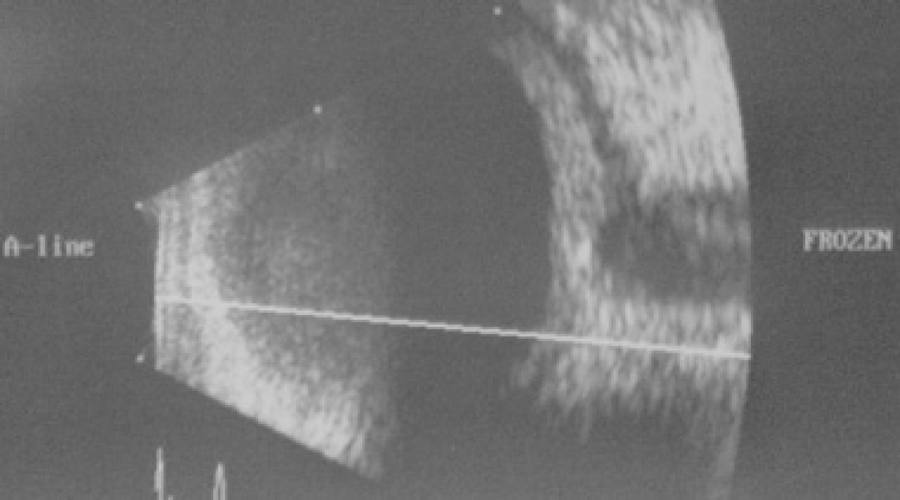
Macular optical coherence tomography (OCT) showed edema with neurosensory retinal detachment in the left eye. B-scan ultrasonography (Figure 2) revealed sclerochoroidal thickening and the presence of sub-Tenon's space fluid (T-sign).
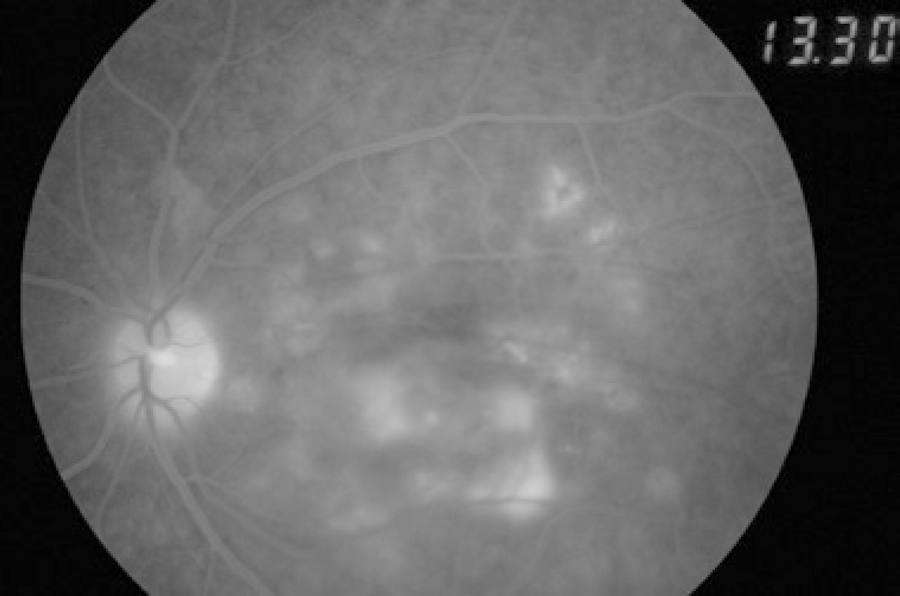
On fluorescein angiography, we found disc staining and multiple early pinpoint retinal pigment epithelial leaks (Figure 3).
The patient was treated for posterior scleritis with oral prednisolone 1 mg/kg body weight once daily. After 2 weeks of treatment, an improvement in pain was noted by the patient, along with BCVA of 6/60 in the left eye with improvement of the macular OCT edema; however, on fundoscopy, worsening of the optic disc edema was found. The orbital CT scan and B-scan ultrasonography revealed identical results. Etiological investigation showed negative anti-HIV antibody test, C-reactive protein level of 0.3 mg/dL, elevated sedimentation rate (59 mm), negative rapid plasma reagin and treponema pallidum hemagglutination test, normal angiotensin-converting enzyme (25 UI/L), negative cytoplasmic and perinuclear anti-neutrophil cytoplasmic antibodies, negative Borrelia burgdorferi and Toxoplasma gondii IgG and IgM, and negative rheumatoid factor and antinuclear antibodies. The chest radiograph was normal and the patient denied any respiratory symptoms or recent travel in TB-endemic regions. The patient had a positive result for the purified protein derivative (PPD) skin test (17 mm induration under corticotherapy 80 mg/day) and interferon-gamma release assay (IGRA), which is a more specific test. Antitubercular chemotherapy was started in combination with the oral corticosteroids, and was a combination of rifampicin 10 mg/kg, isoniazid 5 mg/kg, and pyrazinamide 25 mg/kg. The oral prednisolone treatment was given for 10 weeks, and the antitubercular therapy for 9 months. After 10 weeks of treatment, the patient recovered a visual acuity of 6/6 in the left eye, the optic disc edema and choroidal folds disappeared, and the orbital CT scan (Figure 4) and B-scan ultrasonography were normal. The patient has since remained asymptomatic for a period of 18 months.
DISCUSSION
This case report is an example of a patient with latent TB and severe posterior scleritis, with no signs of anterior segment involvement.
Some authors have suggested that infection due to TB should be considered as a possible cause of scleritis if the investigation reveals a positive PPD skin test, particularly if the scleral inflammation does not respond adequately to standard corticosteroid treatment(5). Given the worsening of the optic disc edema, no improvement of the BCVA, orbital CT scan, and B-scan ultrasonography with oral corticosteroids, and the positive results from the PPD skin and IGRA tests, we assumed that TB was the causative agent of the posterior scleritis, and started antitubercular therapy. An intraocular sample to confirm the diagnosis of Mycobacterium tuberculosis infection was not performed as the patient responded well to the combined treatment of oral corticosteroids and antitubercular therapy. In our investigation, we could not establish the presence of any connective tissue disorder in our patient, and she has had no recurrences in the 18 months of follow-up, which suggests a non-connective tissue disorder as an etiology. Some authors consider a therapeutic trial to be justified in patients with severe sight-threatening intraocular inflammation and latent TB infection(6). Furthermore, the addition of antitubercular therapy to corticosteroids in uveitis patients with latent/manifested TB has been shown to reduce the recurrences of uveitis(7).
The difficulty in optic neuropathy screening in this patient led our infectious diseases specialists to not use ethambutol as part of the antitubercular regimen.
In conclusion, posterior scleritis associated with TB can present with no signs of anterior segment involvement, and responds well to a combination treatment of antitubercular therapy and oral corticosteroids. Oral corticosteroids, given without antitubercular drugs, are likely to worsen the disease in these patients. The establishment of the diagnosis is very important for well-directed therapy, visual recovery, and no recurrences.





 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

