INTRODUCTION
Anomalous posterior vitreous detachment (PVD) is a pathological variant of the aging gel liquefaction process(1,2). In this variant, the vitreous gel adheres in an abnormally strong manner to the retina. Combining the current knowledge regarding PVD with advances in optical coherence tomography (OCT), a panel of specialists convened to develop a consensus classification of vitreomacular interface (VMI) disorders(3), such as vitreomacular adhesion (VMA), vitreomacular traction (VMT), and partial or full thickness macular hole (FTMH)(3,4-6).
VMA occurs during initial and partial PVD, when a portion of the posterior vitreous remains attached to the macula without alterating the underlying retinal contour(4). VMA may develop into VMT, with subsequent symptom development and anatomical distortion observed on OCT. This continuous traction may progress to FTMH or other potentially sight-threatening conditions(4-6).
In general, observation and pars plana vitrectomy have been the only treatment options for vitreomacular interface disorders. The Microplasmin for Intravitreous Injection-Traction Release without Surgical Treatment (MIVI TRUST) program, comprising two randomized clinical trials, demonstrated the benefits of a single 0.125-mg intravitreal ocriplasmin injection (JETREA; ThromboGenics, USA). Good tolerability and higher nonsurgical resolution of VMA were observed in 464 patients who were administered ocriplasmin (26.8%) than in 188 control patients who were administered the placebo (10.1%)(4,6). Supported by this data, in 2012, the US Food and Drug Administration approved pharmacological vitreolysis as a valid therapeutic alternative for symptomatic VMA(5). Ocriplasmin is a recombinant, truncated form of the human plasmin with autolytic and proteolytic activity. It mainly targets fibronectin and laminin that are abundant in vitreous gel and provides in a normal condition, a suitable attachment to the retina(6-8). The resolution of VMA has been typically observed within 28 days of ocriplasmin injection(4,6). The treatment also induced higher rates of FMTH closure (40.6%) compared with the sham group (10.6%)(4). The MIVI TRUST study group results demonstrated major benefits in patients younger than 65 years, with focal adhesions (diameter ≤1500 µm), absence of epiretinal membrane, and phakic lens status(4). In this case series, we report the initial experience of intravitreal ocriplasmin in the treatment of symptomatic VMA in Brazil.
METHODS
This study was a retrospective analysis of a small case series of seven patients who were diagnosed with VMT according to the International Vitreomacular Traction study group and who were treated with ocriplasmin at the Centro Brasileiro de Cirurgia de Olhos (Goiânia, GO) and Centro Brasileiro da Visão (Brasília, DF) in 2013 and 2014(3). Spectral domain OCT (SD-OCT) was performed using Spectralis (Heidelberg Engineering; Heidelberg, Germany). Following informed consent, a single 0.125-mg ocriplasmin injection was administered under sterile conditions. Snellen best-corrected visual acuity (BCVA) values were converted to logMAR units(9).
RESULTS
Patient data are shown in table 1. The subjects had a median age of 66.14 years. Six patients (85.71%) were females. Initial and final BCVA measurements ranged from 0.19 to 0.17, respectively, after a median follow-up of 70.57 days. Overall, 4 patients (57.14%) achieved anatomical resolution (Figures 1 and 2). Three patients (42.8%) were older than 65 years. One of these three patients achieved VMT release during follow-up. All members included in this study were diagnosed with VMA or VMT, and none of them presented with epiretinal membrane or FTMH. Studying the 3 patients who failed to achieve anatomical resolution, one patient exhibited a decrease in BCVA (Figure 3), 3 presented brief metamorphopsia, and one demonstrated transient conjunctival hemorrhage, flashes, and diplopia. No post-injection endophthalmitis or retinal tears were identified.
Table 1 Demographical and clinical characteristics of the study population
| Patient | Sex | Age | Eye | Lens status |
ERM | MH | Focal VMT |
Broad VMT |
Initial BCVA (logMAR) |
Final BCVA (logMAR) |
Initial BCVA (Snellen) |
Final BCVA (Snellen) |
Follow up in days |
VMT resolution (SD-OCT) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 49 | OS | Phakic | – | – | + | – | 0.30 | 0.18 | 20/40 | 20/30 | 28 | + |
| 2 | F | 74 | OD | PCIOL | – | – | + | – | 0.10 | 0.00 | 20/25 | 20/20 | 4 | + |
| 3 | F | 62 | OD | PCIOL | – | – | + | – | 0.18 | 0.00 | 20/30 | 20/20 | 40 | + |
| 4 | F | 79 | OS | PCIOL | – | – | + | – | 0.30 | 0.30 | 20/40 | 20/40 | 61 | – |
| 5 | F | 63 | OS | PCIOL | – | – | + | – | 0.00 | 0.40 | 20/20 | 20/50 | 28 | – |
| 6 | M | 72 | OD | PCIOL | – | – | – | + | 0.30 | 0.18 | 20/40 | 20/30 | 319 | – |
| 7 | F | 64 | OS | PCIOL | – | – | + | – | 0.18 | 0.18 | 20/30 | 20/30 | 14 | + |
PCIOL: posterior chamber intra ocular lens; logMAR: logarithm of minimum angle of resolution; OD: right eye; OS: left eye; ERM: epiretinal membrane; MH: macular hole; VMA: vitreomacular adhesion; VMT: vitreomacular traction; SD-OCT: spectral domain optical coherence tomography.
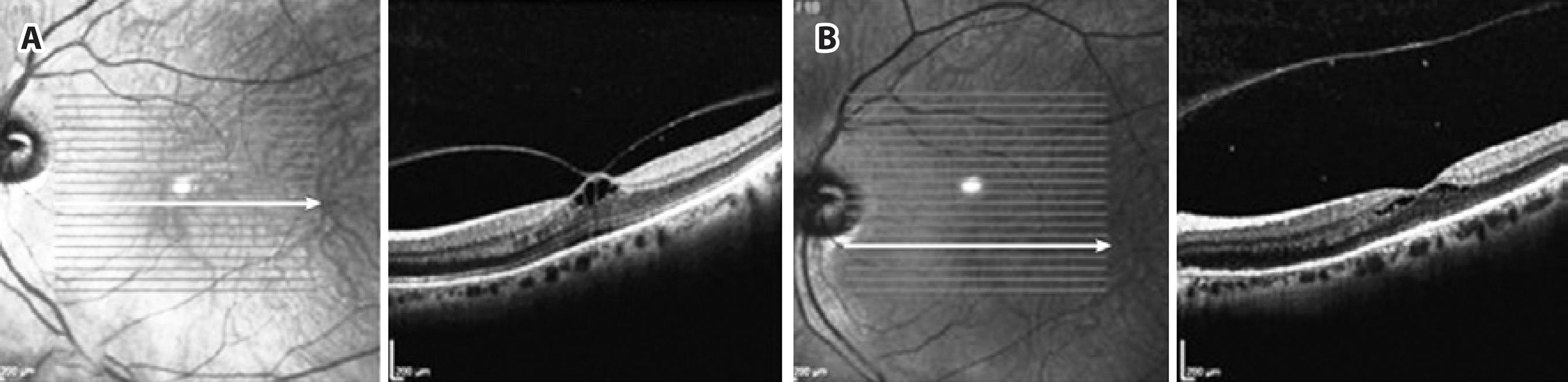
Figure 1 Initial Spectral Domain Optical Coherence Tomography (SD-OCT) of a 49-year-old phakic patient showing focal vitreo-macular traction (VMT) (A), with complete separation of the posterior hyaloid 4 days after ocriplasmin injection, accompanied by re-establishment of macular contours (B).
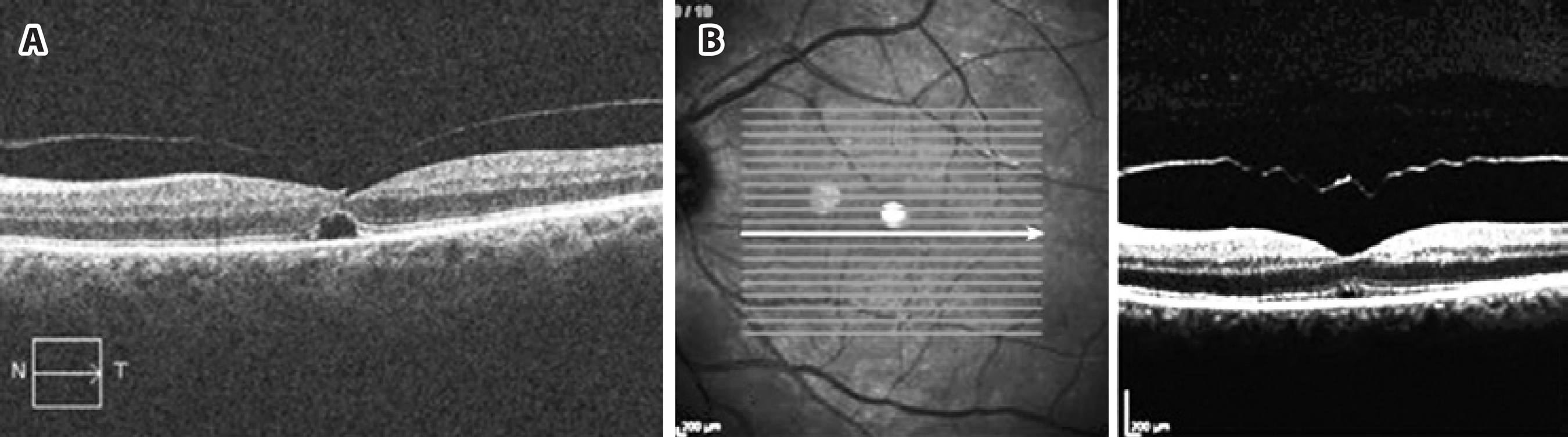
Figure 2 A 64-year-old patient having focal vitreo-macular traction (VMT) with subretinal fluid as observed on Cirrus Spectral Domain Optical Coherence Tomography (SD-OCT) (Carl Zeiss Meditec, USA), which was clinically managed over 58 days (A); 14 days after ocriplasmin injection, retinal anatomy was re-established (B).
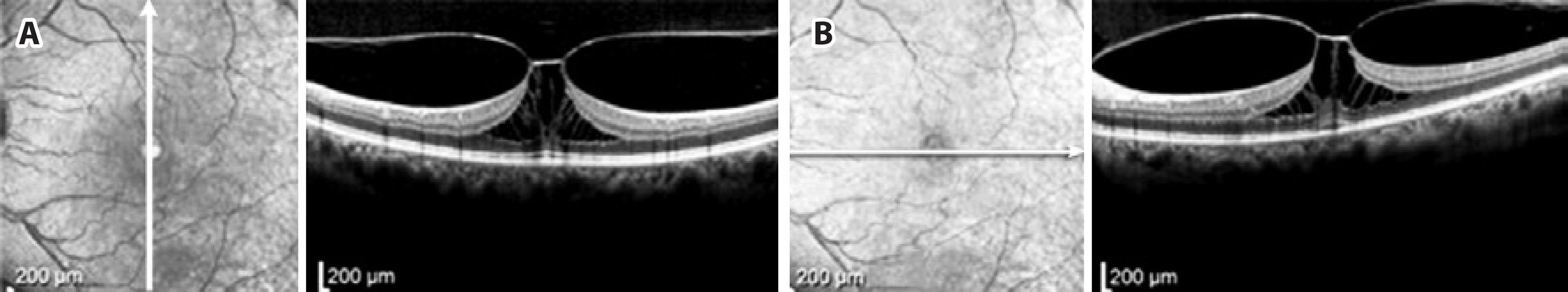
Figure 3 A 63-year-old patient complained about significant metamorphopsia (A). Spectral Domain Optical Coherence Tomography (SD-OCT) showed persistent focal vitreo-macuolar traction (VMT), with no reported fracture in the ellipsoid segment (IS/OS) of the outer retina during the follow-up period (B); the patient experienced loss of vision from 20/20 to 20/50.
DISCUSSION
Pharmacological vitreolysis has been studied as an alternative to vitrectomy and has become a promising medical agent because of its ability to induce PVD, for its stable structure, and as a supplement to observation and vitrectomy in managing selected disorders(5-8,10). Previous studies have demonstrated that appropriate patient selection is critical for improving outcomes using ocriplasmin(5-8,10).
The overall frequency of successful release (4 eyes, 57.1%) was higher in this study than in phase III clinical trials (26.5%). Three patients (42.8%) from our series were older than 65 years, which has been related to a worse prognosis following pharmacological vitreolysis(4). Kim et al.(5), after studying a carefully selected group of 19 patients, demonstrated a separation of VMT in 42% of the patients. In a sample size of 17 patients, Singh et al.(7) reported a 47.1% resolution rate within 28 days after the injection; although this group reported predictive factors and patient enrollment similar to those reported by the MIVI TRUST group(4), they used SD-OCT instead of time domain OCT, which has an inferior resolution.
According to Singh et al.(7), almost all patients who responded to therapy had outer retinal fracture in the ellipsoid zone (IS/OS junction) as observed on SD-OCT, which was probably because of the potential toxicity of the drug. Nevertheless, this did not alter the study outcomes regarding the spontaneous resolution of the symptoms or SD-OCT findings, with treatment response occurring in most patients within the first 7 days after the procedure, with further improvement during follow-up. In our group, four patients initially complained of blurred vision or reduced BCVA in the initial observation after the injection; however, no evident outer retina abnormalities could be observed on SD-OCT.
The limitations of our study include the small sample and its retrospective design. A retrospective study, which was performed with eight patients, revealed complete resolution in 62.5% after a minimum period of 1 month of observation, corroborating our results(8). It is important to highlight that this study included only a small case series, and these results cannot be directly compared with randomized clinical trials. To the best of our knowledge, this is the first study reporting the initial data on pharmacological therapy of VMI-related diseases in Brazil.
In conclusion, in our study, 4 of 7 seven eyes achieved anatomical resolution of VMT after a single 0.125-mg ocriplasmin injection. This corroborates with phase III clinical trials that have proved the benefits of ocriplasmin, leading to a shift in treatment paradigm with respect to achieving optimal outcomes in symptomatic patients. Future and larger reports, particularly with SD-OCT, should help us understand and better explain the drug's mechanism of action.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

