INTRODUCTION
Keratoconus is characterized by bilateral asymmetrical non-inflammatory corneal ectasia that leads to central or inferotemporal stromal thinning, corneal protrusion (which may be surrounded by iron deposits in the epithelial basement membrane), and rupture of Bowman's layer. Irregular corneal astigmatism may result in significant visual loss in approximately 1 per 2000 individuals in the general population, with a diagnosis usually made in the second decade of life(1,2). Keratoconus morphology may be categorized as: nipple cones, 5-mm diameter, with the apex localized centrally or paracentrally often displaced inferonasally; oval cones, 5 to 6-mm diameter, with inferotemporally ellipsoid profile; and globus cones, more than 6-mm diameter, occupying more than 75% of the cornea(3).
The use of rigid glass contact lenses was first described in 1888 by Adolf Fick. Contact lens fitting remains the most appropriate option for correcting refractive errors induced by keratoconus, as this approach regularizes the corneal surface, thereby ensuring maximum visual acuity with decreased residual aberration. Contact lenses provide superior amount and quality of vision as compared to spectacles(4,5). In their multicenter analysis of patients with keratoconus, Lass et al. reported that 74% do not require surgery and can be managed with either contact lenses (84%) or spectacles (13%), or without correction (3%)(6). Bilgin et al. reported a success rate of 98.9% in1004 patients fitted with contact lenses over a 30-year period(7).
Rigid gas-permeable contact lenses (RGPCL) remain the most commonly used type of lens and are available in several designs, including bicurve and multicurve. The development of new lenses and designs has enabled improvements in visual acuity and either prevented or postponed the need for surgical intervention in an increased number of patients(6). However, there is currently a lack of consensus regarding the most efficacious method for fitting contact lenses in patients with keratoconus, given the various topographical patterns and evolution grades observed in affected populations.
The purpose of the present study was to evaluate the association between keratoconus evolution grade and topography pattern and the type and design of fitted contact lens.
METHODS
A retrospective analysis of 185 patients with keratoconus (325 eyes) fitted with contact lenses between 2007 and 2010 was conducted at the Contact Lens Sector, Paulista School of Medicine, Federal University of São Paulo (EPM/UNIFESP). Diagnoses were made by the Cornea Department. Age, gender, keratometry, base curve, and lens diameter were recorded. Keratoconus was classified according to keratometry (K1) as either incipient or grade I (K<45.00 D in both meridians), moderate or grade II (K between 45.00 and 52.00 D in both meridians), advanced or grade III (K between 52.00 and 62.00 D in both meridians), and severe or grade IV (K>62.00 D in both meridians) and according to cone morphology (nipple, oval, globus, or indeterminate). All patients were initially fitted with monocurve (spherical or aspherical) RGPCL with only one central base curve. In cases with unsuccessful initial lens fitting (due to contact lenses with excessive apical bearing, excessive peripheral seal-off, excessive pooling, or patient intolerance), the type and/or lens design was modified to one of the following: bicurve RGPCL (designed by Joseph Soper), with a characteristic variable central curve and a constant (45.00 D) intermediate curve; multicurve lens, a variation of the Soper design with 2 or more intermediate curves or aspherical flattening from the central till the peripheral curve; or multispherical lens, with a characteristic single spherical central area, approximately 5 mm in size, with multiple flatter spherical peripheral curves. Adaptation with soft contact lenses for keratoconus correction was attempted in patients that were intolerant to rigid contact lenses. Analyses for descriptive data were performed. Continuous variables are presented as means ± standard deviation. Categorical variables are presented as frequencies. Between-group differences were analyzed using the chi-square test. The SigmaPlot 11.0 software package was used for all statistical analyses with the significance level set to 5%.
RESULTS
A total of 325 eyes were evaluated in the present study. The average patient age was 24.7 ± 8.5 years. Topography-derived mean K1 and K2 were 47.96 ± 6.75 and 52.43 ± 8.5, respectively. The mean base curve of soft contact lenses and RGPCL was 40.66 ± 2.84 and 48.8 ± 4.5 diopters, respectively. The mean visual acuity was 0.5 ± 0.3 (logMAR) with refraction and 0.2 ± 0.1 with contact lenses (P<0.05). The mean diameter of rigid contact lenses was 9.1 ± 4.1 mm (Table 1). Bicurve contact lenses were fitted in 138 (42.4%), monocurve lenses in 126 (38.8%), and multicurve lenses in 45 (13.8%) eyes. Soft contact lenses were fitted in 7 (2.1%); keratoconus special soft contact lenses (Perfect Keratoconus, World Vision, São Paulo, Brazil) in 2 (0.6%); multispherical (Century, Optolentes, Porto Alegre, Brazil) in 6 (1.8%); and reverse curve design contact lenses (Ultraflat, Ultralentes, Porto Alegre, Brazil) in 1 eye/s (0.3%, Table 2).
Table 1 Descriptive analysis of eyes studied and lens fitted
| Number of eyes (n) | 325 |
| Patient age (years)* | 24.70 ± 8.50 |
| Base curve in soft contact lenses (D)* | 40.66 ± 2.84 D |
| Base curve in rigid contact lenses (D)* | 48.80 ± 4.50 D |
| K1 (D)* | 47.96 ± 6.75 D |
| K2 (D)* | 52.43 ± 8.51 D |
| Spectacle-corrected visual acuity (logMAR)* | 0.50 ± 0.30 |
| Contact lens-corrected visual acuity (logMAR)* | 0.20 ± 0.10 |
Table 2 Design of fitted lenses
| Contact lens design | % |
|---|---|
| Monocurve | 38.8% |
| Bicurve | 42.4% |
| Multicurve | 13.8% |
| Other | 5.0% |
Sixty-two eyes were classified as grade I (19.07%), 97 as grade II (29.8%), 121 as grade III (37.2%), and 45 as grade IV (13.8%). Monocurve contact lenses were successfully fitted in 66.1% of patients with grade I keratoconus, and 42.3% patients with grade II keratoconus (P<0.05; Table 3). Of the 159 eyes classified as having mild (grade I) or moderate (grade II) keratoconus, monocurve RGPCL, bicurve lenses, and other lenses were fitted in 51.5%, 30%, and 19% of cases, respectively (P<0.05). Monocurve RGPCL and bicurve lenses were fitted in 26% and 55% of patients with advanced (grade III) or severe (grade IV), respectively (P<0.05; Table 4).
Table 3 Association between the keratoconus evolution grade and type and design of contact lenses
| Grade I | Grade II | Grade III | Grade IV | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | 62 | 97 | 121 | 45 | ||||||||
| % | 19.07% | 29.80% | 37.20% | 13.80% | ||||||||
| Design | n | % | Diameter*
(mm) |
n | % | Diameter*
(mm) |
n | % | Diameter*
(mm) |
n | % | Diameter*
(mm) |
| Monocurve | 41 | 66.1% | 9.20 ± 0.20 | 41 | 42.3% | 9.0 ± 0.4 | 36 | 29.8% | 8.9 ± 0.4 | 8 | 17.8% | 8.7 ± 0.0 |
| Bicurve | 11 | 17.7% | 9.40 ± 0.30 | 36 | 37.1% | 9.3 ± 0.3 | 63 | 52.1% | 9.3 ± 0.4 | 28 | 62.2% | 9.2 ± 0.4 |
| Multicurve | 1 | 1.6% | 8.7 | 13 | 13.4% | 8.7 ± 0.1 | 22 | 18.1% | 8.7 ± 0.0 | 2 | 20.0% | 8.9 ± 0.3 |
| Multispherical | 4 | 6.5% | 10.00 ± 0.20 | 2 | 2.0% | 9.8 ± 0.0 | 0 | 0.0% | - - - | 0 | 0.0% | - - - |
| Reverse curve | 0 | 0.0% | - - - | 1 | 1.0% | 11.0 | 0 | 0.0% | - - - | 0 | 0.0% | - - - |
| Hydrophilic | 4 | 6.5% | 14.10 ± 0.30 | 3 | 3.1% | 14.3 ± 0.3 | 0 | 0.0% | - - - | 0 | 0.0% | - - - |
| Special hydrophilic for keratoconus | 1 | 1.6% | 14.2 | 1 | 1.0% | 14.2 | 0 | 0.0% | - - - | 0 | 0.0% | - - - |
*= average ± standard deviation.
Table 4 Association between grade of keratoconus and design of fitted contact lenses
| Grades I/II | Grades III/IV | |
|---|---|---|
| Monocurve | 51% | 26% |
| Bicurve | 30% | 55% |
| Other design* | 19% | 19% |
*= hydrophilic contact lenses, keratoconus special hydrophilic contact lenses, multispherical lenses, and reverse curve design contact lenses.
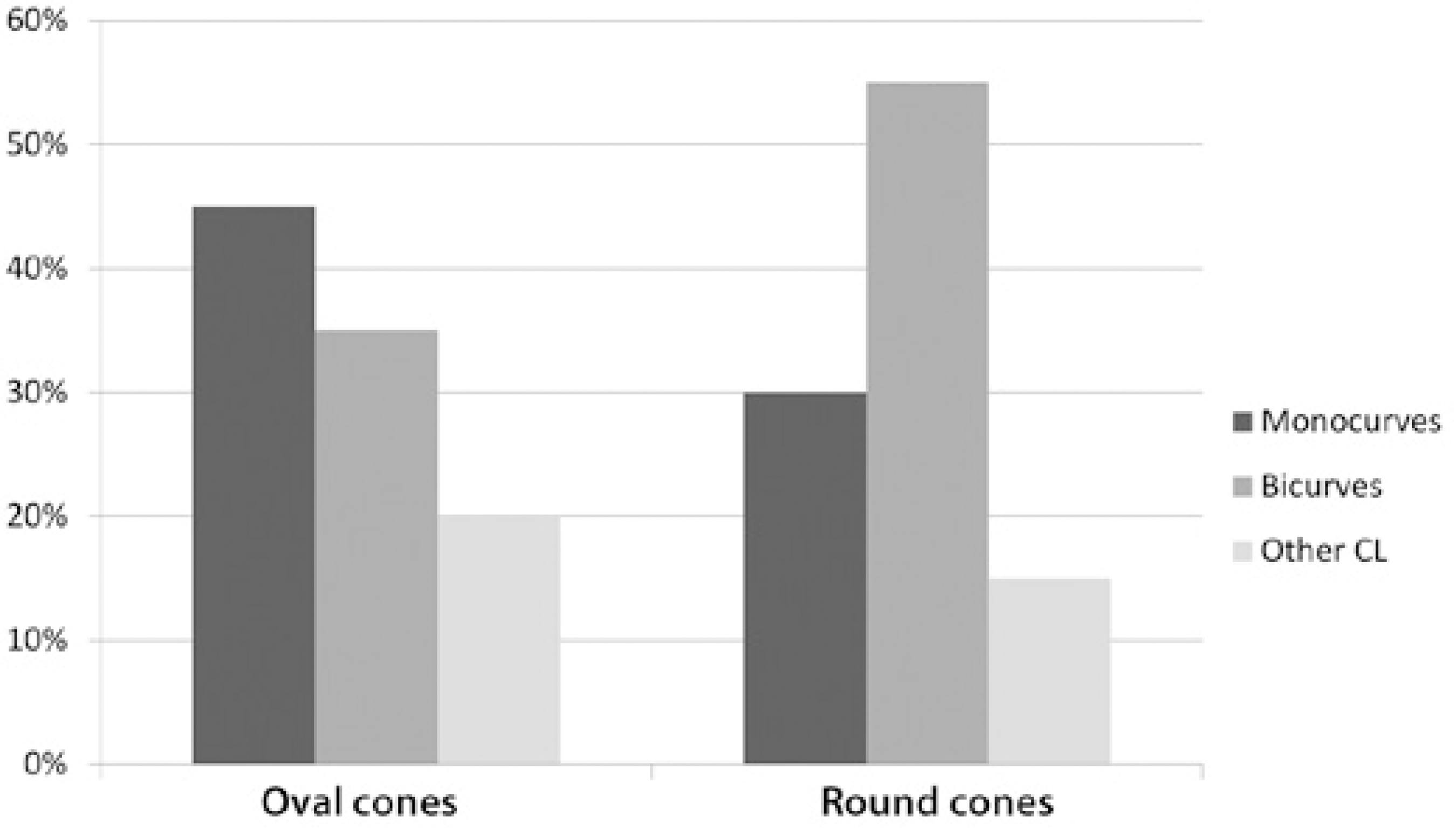
In patients with oval cones, 45% were fitted with monocurve lenses, 35% with bicurve lenses, and 20% with other lens types. In patients with round cones (nipple morphology), 55% were fitted with bicurve lenses, 30% with monocurve lenses, and 15% with other lens types (P<0.05; Figure 1).
DISCUSSION
RGPCL remain an excellent option for visual rehabilitation of patients with keratoconus. In the present study, the corrected visual acuity of patients fitted with contact lenses was higher than those fitted with spectacles (0.2 vs. 0.5 logMAR). No statistically significant difference in the number of eyes classified as mild, moderate, advanced, or severe was observed in the present study.
Monocurve RGPCL were more frequently fitted in patients with grades I or II (51%) than in those with grades III or IV (26%; P<0.05), while bicurve lenses were fitted in the most advanced cases of keratoconus (30% in grades I or II and 55% in grades III or IV; P<0.05). In a retrospective study, Ghanem et al. analyzed 881 eyes with keratoconus and concluded that the majority could be fitted with rigid monocurve contact lenses. However, the results of the present study indicate that other designs may be more appropriate in patients with more advanced and severe keratoconus. Toric contact lenses and the "piggyback" system were reported to be more suited to central cones, while monocurve and bicurve rigid contact lenses were more suited to inferior peripheral cones(8). In addition, a separate study by the same group demonstrated that the design of contact lens used in the initial evaluation does not provide the best fit between the lens and cornea, due to variations in corneal topography over time. The Soper-McGuire lenses have been shown to be more effective than monocurve RGPCL in patients with advanced and central keratoconus(9).
Cone morphology may influence the fitting of different lens designs. In the present study, monocurve lenses fitted oval cones better (45%). However, a significant portion of eyes required bicurve lenses (35%). Round cones mostly required bicurve lenses in order to achieve a better standard of adaptation (55%).
CONCLUSION
Monocurve RGPCL were more frequently fitted in patients with mild to moderate keratoconus or with oval cone morphology, while bicurve lenses were more frequently fitted in patients with severe or advanced keratoconus, most likely as these lenses are considered the best option for patients with round cones due to increased corneal asphericity.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

