INTRODUCTION
Refractive surgery with excimer lasers is used worldwide for the treatment of myopia, hyperopia, astigmatism, corneal scar, and other diseases(1-3). Postoperative corneal hypoesthesia has been reported as a consequence of refractive surgery. The photorefractive keratectomy (PRK) technique, despite being considered a safe procedure, has been reported as associated with marked reduction in corneal sensitivity(4-8).
The cornea is one of the regions of the human body that has the highest amount of naked nerve endings and, therefore, has a high level of pain sensitivity. The sensory innervation of the cornea is essential in maintaining corneal integrity(9,10). The touch sensitivity threshold of the cornea, particularly in the center, is rather low. Loss or reduction of normal corneal sensitivity may compromise reactions to flash, delay epithelial healing, reduce tear flow, and predispose to the development of neurotrophic keratitis, sterile corneal necrosis, and infectious keratitis(11,12).
The PRK procedure consists of removing the corneal epithelial layer with its basement membrane followed by excimer laser photo-disruption of Bowman's layer and the anterior portion of the corneal stroma resulting in impairment of nerve endings in the nerve plexus of the subepithelial and anterior stromal(13,14).
The Cochet-Bonnet esthesiometer is an established tool for determining corneal sensitivity by evaluating the corneal touch threshold (CTT). This instrument contains an adjustable nylon filament with a defined diameter, which is applied in different lengths to the cornea in five prescribed regions. The length of the nylon filament estimates the applied pressure on the corneal surface. The shorter the filament, the more pressure is applied to the cornea and vice versa. The CTT is reached as soon as a blink reflex is consistently elicited with the same pressure or length of filament. Estimation of corneal sensitivity may be necessary for the diagnosis and monitoring of eye diseases or the evaluation of corneal healing following surgery(15).
The present study aimed to evaluate preoperative and postoperative corneal sensitivity following PRK surgery with and without intraoperative use of mitomycin C.
METHODS
We performed a prospective, longitudinal, interventional study. Patients were enrolled between December 2013 and January 2014, with all surgeries performed on April 3, 2014. Patients were advised to discontinue the use of contact lenses 2 weeks prior to surgery.
Individuals over 21 with stable ametropia (considered stable when no variation >0.25 D in static refraction is observed within 1 year), a spherical equivalent between -1.50 and -8.00 D, and a cylindrical component of <2.00 D with normal corneal topography were enrolled in the present study. Patients unavailable for control visits or with previous eye surgery, corneal thickness <500 µm, systemic diseases (i.e., collagenosis, uncontrolled diabetes, and immunodeficiency), or eye diseases that could affect surgical outcomes were excluded from the present study.
All tests were performed 1 week prior to surgery (Pre), on postoperative day 30 (30 post), and postoperative day 90 (90 post). Corneal sensitivity was measured in the central region using a Cochet-Bonnet esthesiometer(9). The esthesiometer filament was applied perpendicularly to the pressing surface of the cornea obtained by bending a small portion (approximately 5%) of its length. The procedure was repeated with a gradual reduction in the length of wire in 5-mm increments. Patients reported perception of the test at every touch of the filament. To confirm patient responses, the central area of the cornea was tested three times with a minimum interval of 60 s. The greatest length of the wire that elicited a response to the stimulus was recorded in millimeters and considered the CTT of the corneal central area(15). Normal values for corneal sensitivity evaluated by Cochet-Bonnet esthesiometry are >40 mm in the central region of the cornea. All tests were conducted in the same environment in a closed room.
Pattern delineation and mechanical scarification (spatula) of the cornea was performed followed by photoablation using an EC5000® excimer laser (Nidek Inc. Fremont, California) targeting a 6.5-mm ablation zone. Patients with a greater refractive error of 4 D were intraoperatively administered 0.02% mitomycin C for 20 s with subsequent washing with balanced saline solution. A bandage contact lens was maintained for 7 days in all patients. Standard prescription eye drops included tobramycin 0.3% and dexamethasone 0.1% (Tobradex®, Alcon Laboratories, Inc. Fort Worth, TX) instilled as one drop every 4 h for 7 days and ketorolac tromethamine eye drops (Acular®, Alcon Laboratories, Inc. Fort Worth, TX) instilled every 6 h for 40 days.
Statistical analyses were initially performed in a descriptive manner by calculating a number of summary measures including mean, median, minimum and maximum values, standard deviation, absolute and relative frequencies (percentage), and individual graphic profiles (lines). The inferential analyses performed to confirm or refute findings of descriptive analyses were: analysis of variance in blocks with two random factors (patient and side effect) compared with central corneal sensitivity (mm) at varying study time points (preoperatively, and 30 and 90 days postoperatively) adjusted for mitomycin use and gender. Comparisons were performed using the Tukey method (Neter et al., 1996) when necessary(16). A significance level α=5% was set for all inferential analyses. Data were entered into Excel 2010 spreadsheets for Windows for proper storage of information. Statistical analyses were performed using the statistical program, R, version 2.15.2.
RESULTS
The selected sample in the present study consisted of 45 patients comprising 23 (52.2%) women and 22 (47.8%) men. The mean age was 31.8 ± 7.4 years, ranging from 21 to 46 years. Mitomycin C was administered to 24 eyes (53.3%).
The following CTT values for the sensitivity in the central region of the cornea were obtained: 51.1 ± 7.4 in the preoperative period; 26.7 ± 9.3 at 30 days postoperatively; and 43.2 ± 8.3 at 90 days postoperatively. A statistically significant difference in CTT values was observed between the three study time points (P<0.001; Table 1; Figure 1). The inferential results confirmed the results of descriptive analyses, with no significant differences in quantitatively measured sensitivity observed between the three study time points (Table 2). Sensitivity values in the central region >40 mm were considered normal, with 25 (55.6%) of 45 eyes found to have normal sensitivity on postoperative day 90.
Table 1 Summary of central corneal sensitivity measurements (mm) over time
| Central corneal sensitivity (mm) | |||||||
|---|---|---|---|---|---|---|---|
| N | Mean | Median | Minimum | Maximum | Standard deviation | P-value | |
| Preoperative | 45 | 51.1 | 50.0 | 30.0 | 60.0 | 7.4 | <0.001a |
| 30 days | 45 | 26.7 | 25.0 | 15.0 | 50.0 | 9.3 | |
| 90 days | 45 | 43.2 | 45.0 | 30.0 | 60.0 | 8.3 | |
a= analysis of variance in blocks with two random factors.
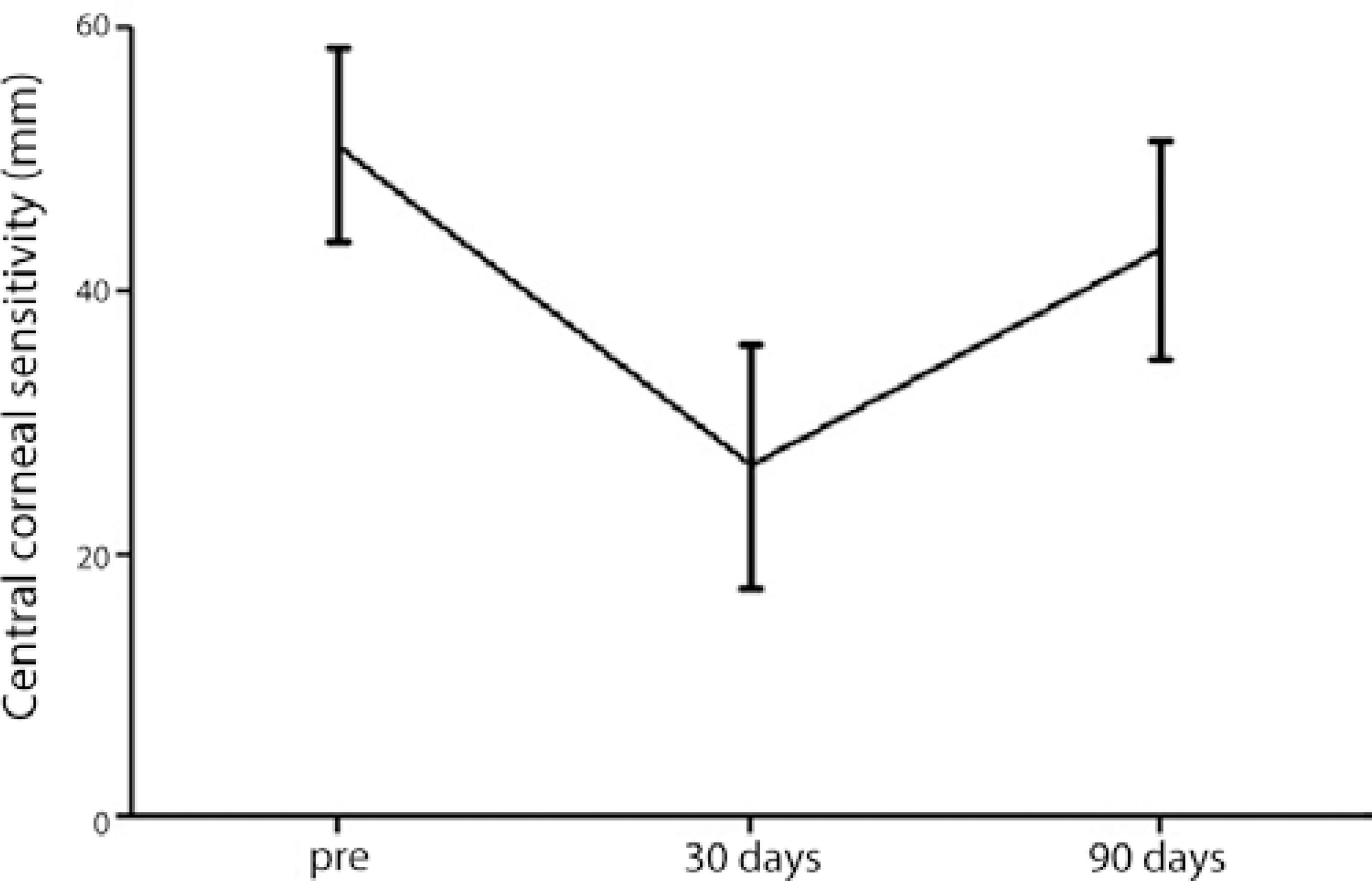
Figure 1 Mean measures of sensitivity in the central region of the cornea (mm) from the eyes of patients with standard deviations according to study time point.
Table 2 Results of multiple comparisons by the Tukey method of quantitative evaluations of central cornea region sensitivity (mm) over time
| Comparison | P-value |
|---|---|
| Preoperative vs. 30 days postoperatively | <0.001 |
| Preoperative vs. 90 days postoperatively | <0.001 |
| 30 days postoperatively vs. 90 days postoperatively | <0.001 |
Decreased sensitivity in the central region between the preoperative values and postoperative day 30 was also evaluated. The reduction was estimated using the following expression:
The average reduction in central region sensitivity observed in the 45 eyes was 45.9%, ranging from 33.3% to 75.0% with a standard deviation of 23.2%. The corneal esthesia analysis performed preoperatively and on postoperative day 90 revealed an average reduction of 14.9%, ranging from 6.7% to 41.7% with a standard deviation of 13.6%.
Mean sensitivity values in the group administered mitomycin C preoperatively and on postoperative day 90 groups were 51.3 ± 6.1 and 39.2 ± 6.7, respectively (P <0.001). In patients who did not receive intraoperative mitomycin, mean sensitivity values preoperatively and on postoperative day 90 were 51.0 ± 8.7 and 47.9 ± 7.7, respectively ( P=0.021; Table 3).
Table 3 Summary of pre and 90th postoperative central cornea sensitivity (mm) measurements according mitomycin use
| Central sensitivity (mm) | ||||||||
|---|---|---|---|---|---|---|---|---|
| N | Mean | Median | Minimum | Maximum | Standard deviation | P-value | ||
| Mitomycin | Preoperative | 24 | 51.3 | 50.0 | 40.0 | 60.0 | 6.1 | <0.001a |
| 90 days post | 24 | 39.2 | 37.5 | 30.0 | 55.0 | 6.7 | ||
| Without mitomycin | Preoperative | 21 | 51.0 | 50.0 | 30.0 | 60.0 | 8.7 | 0.021a |
| 90 days post | 21 | 47.9 | 45.0 | 30.0 | 60.0 | 7.7 | ||
a= analysis of variance in blocks with two random factors.
DISCUSSION
In the present study, we observed a reduction in corneal sensitivity on postoperative day 30 and a recovery of sensitivity to normal values on postoperative day 90; however, corneal sensitivity did not fully recover to preoperative values (P<0.001). These data are consistent with previous literature demonstrating reduced central corneal sensitivity in the first month following PRK. Studies conducted in rabbits, which have a similar inervacional structure to the human cornea, have demonstrated the reappearance of peripheral neurites around the sixth week following PRK(17). Likewise, Pallikaris et al.observed recovery of central corneal sensitivity to values considered normal or near normal in the third month after PRK(18).
In the mitomycin C group of the present study, no recovery of corneal esthesia to normal values was observed ay 90 days after the procedure, with a mean value of 39.2 ( P<0.001). As mitomycin was only used in patients with ablation >4 D, the lack of sensitivity recovery during the expected period may be attributable to the greater amount of tissue removed in these patients. However, the relationship between ablation depth and decreased corneal sensitivity following photorefractive surgery remains unclear(19). Although Chucket al. reported that the measurement of the decreased corneal sensitivity induced by laser-assisted in situ keratomileusis (LASIK) appears to be independent of the depth of the ablation, other studies have shown that the depth of cut or ablation in PRK affects recovery of corneal sensitivity(20). Campos et al. reported patients with a preoperative myopia of -6.50 D recovered 95.7% of central corneal sensitivity after 3 months in a series of 14 eyes that underwent PRK, while patients with severe myopia (>-9.00 D) recovered 86.2% of the original cornea sensitivity to values within normal limits(21).
Péres-Santoja et al. and Matsui et al. investigated the sensitivity of the central cornea in similar patients groups but without the administration of 0.02% mitomycin C and observed a recovery of esthesia 90 days after the procedure to preoperative values(14,19). Thus, although patients administered mitomycin C in the present study had greater amounts of tissue removed (between -4.00 and -8.00 D), this amount was relatively small compared with previous comparable studies, and corneal sensitivity would still be expected to return to normal levels in these patients.
Farahi et al. compared CTT values between PRK alone and PRK with mitomycin C over a 12-month period postoperatively. The authors observed a reduction in CTT values in both groups postoperatively, with no statistically significant difference observed between groups(22).
Corneal sensitivity can be influenced by many variables including age, iris color, hormonal changes, type of eyelid closure, and psychological state. The determination of any single factor responsible for reduced sensitivity corneal in individual patients is questionable, particularly in patients undergoing refractive surgery(9).
Further studies are required to evaluate late recovery of corneal sensitivity in patients administered mitomycin C and compare outcomes with patients undergoing other refractive procedures. Recovery following LASIK typically occurs at approximately 6 months postoperatively(14,23).
CONCLUSION
The results of the present study demonstrate corneal sensitivity following PRK recovered to normal levels at 90 days after surgery in patients who did not receive mitomycin C; however, a 6.08% reduction in corneal sensitivity was observed at this time point compared with preoperative levels.
In patients administered mitomycin C, a 23.59% reduction in CTT compared with preoperative levels was observed who did not recover to normal levels by postoperative day 90.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

