INTRODUCTION
The objective of strabismus surgery is to achieve motor alignment and sensory improvement with a minimum number of procedures(1). Long-lasting favorable results depend on good control of over- and under-corrections during the immediate postoperative period(2). Tables and algorithms for the number of muscles to be included in the surgery have been formulated based on the results obtained from large patient populations; however, standardized calculations are affected by various factors that could reduce the success of surgical results(3). Moreover, the ability to modify the site of the muscle insertion in the globe and possibility of refining surgical results and controlling postoperative deviations caused Jampolsky to reintroduce an adjustable suture technique in 1975 that was based on the ideas of O'Connor, Harms, and Bielschowsky(4-6). The indications for adjustable sutures are numerous and include several circumstances of an unforeseen nature (paralysis, restrictive strabismus, and history of prior surgery). Although the adjustable suture technique has been used for over three decades and the applicability of the method has been widely reported, randomized control trials are required(7), and its indication for horizontal concomitant deviations is controversial.
To highlight these issues, we compared the surgical results of adjustable and non-adjustable suture techniques for concomitant horizontal strabismus immediately after surgery and at a later time point, using probabilistic sampling of a patient population.
METHODS
The subjects for this historical cohort study were recruited through the charts of patients undergoing horizontal strabismus surgery at a strabismus unit at a university hospital in Brazil, and from the private practice of one of the authors (HCA), for a 25 year-period, beginning in 1977. One of the authors was present during all surgeries. Subjects were selected, using probabilistic sampling based on the surgical technique employed: adjustable or non-adjustable.
Initially, a pilot study was conducted with the charts of 58 patients (29 for each surgical technique) to define the number of patients necessary to achieve sufficient statistical power. A relative risk of 0.62 was found for the two techniques. A power (β) of 90% and an alpha error (α) of 5% were adopted. These parameters defined a required minimum sample of 104 patients in each group, using the StatCalc module of Epi Info. A 15% increase in the number of patients was adopted to compensate for possible losses during the study.
The charts of patients with esotropia (ET) or exotropia (XT) of up to 55 prism diopters (PD) at distance were included. Exclusion criteria included all intermittent or vertical deviations, anisotropias >5 PD, syndromes, paresis or paralysis of eye muscles, a history of vertical muscle surgery, restrictive or paretic strabismus, reoperations, botulinum toxin injection, and patients postoperatively followed up for <3 months.
The inclusion criteria were as follows: a chart was initially selected by probabilistic sampling from the total number of charts, including 252 adjustable strabismus surgery charts (Group 1) and 1187 non-adjustable strabismus surgery charts (Group 2). Group 1 was always the first choice. A chart was selected and included in the study if it met all of the inclusion and exclusion criteria; if not, it was rejected and a new chart was selected. Therefore, 231 patients were selected: 107 had undergone operation using an adjustable suture technique, and 124 had undergone non-adjustable surgery.
The following data were extracted from the selected charts: visual acuity, preoperative deviation, age during surgery, surgical planning, adjustment information if performed, and postoperative deviation. Visual acuity considered for each eye was the one used for optical correction. In amblyopes, the most recent visual acuity measured before surgery was considered, upon failed occlusion. The most recent preoperative deviation for distance (ET/XT), obtained immediately before surgery, was recorded in PD.
Surgical planning was recorded for each patient, including the number of millimeters recessed or resected. For the adjustable surgeries, the following parameters were assessed: the surgical planning, need for adjustment, and deviation before and after the adjustable maneuver. The adjustable suture technique and adjustment postoperatively performed were in accordance with the technique previously described by Jampolsky(1,8). Adjustments were performed only on recessed muscles. Surgical success was defined as an esodeviation of up to 10 PD. For XT patients, surgical success was defined as a residual deviation ranging from orthotropia and an esodeviation of up to 10 PD. Undercorrections were not included in the success group in this study, as we have previously excluded all intermittent deviations, and reoperations with a higher risk of postoperative diplopia. Postoperative data on deviation were recorded at postoperative day 1, 1 and 3 months after surgery, and the last visit.
For statistical analysis, data were stratified according to the type of surgery and strabismus, and the chi-square and Fisher's tests were used. An α error of 0.05 was specified. The comparability between subgroups ET and XT was verified based on variants, such as the presence of amblyopia, angle of deviation, preoperative follow-up, and age during surgery.
RESULTS
The study involved 107 and 124 patients in the adjustable and non-adjustable surgery groups, respectively. The adjustable surgery group comprised 84 patients with ET (78.5%) and 23 with XT (21.5%), and the non-adjustable surgery group comprised 93 cases with ET (75.0%) and 31 with XT (25.0%).
In the ET subgroup, the frequency of amblyopia was 58.3% (49 patients) in the adjustable group and 55.9% (52 patients) in the non-adjustable group; in the XT subgroup, the frequency of amblyopia was 60.9% (14 patients) in the adjustable group and 54.1% (17 cases) in the non-adjustable group. With regard to the distribution of ametropia, the majority of patients in both subgroups undergoing either technique presented with spherical equivalents of <5 diopters (between 83% and 90%). Mean angles of deviation were similar: adjustable ET, 37° ± 11° PD; non-adjustable ET, 38° ± 10° PD; adjustable XT, 31° ± 7° PD; and non-adjustable XT 37° ± 10° PD. Mean preoperative follow-up was similar between subgroups and techniques: adjustable ET, 2.4 ± 3.8 years; non-adjustable ET, 2.4 ± 4.0 years; adjustable XT, 1.3 ± 2.6 years; and non-adjustable XT, 2.0 ± 3.4 years. The mean age of patients in the adjustable suture subgroups was higher than that of patients in the non-adjustable suture subgroups: 19.1 ± 7.0 years and 9.9 ± 7.4 years in the ET subgroups and 24.2 ± 7.5 years and 15.9 ± 10.4 years in the XT subgroups.
The highest rate of monocular surgery was observed in the adjustable groups: 91.7% (77 patients) for ET and 100% (23 patients) for XT; monocular surgery was performed in 77.4% (24 patients) of patients undergoing non-adjustable XT. Binocular surgery (bilateral recession) was predominant in the non-adjustable ET group, 36 patients (61.3%). After initial postoperative evaluation, adjustment was required in 60% of all patients in Group 1; 64.3% of those with ET, and 56.5% of those with XT. Muscle adjustment failed in 9 patients (16.7%) from the ET group and 2 (15.4%) from the XT group. Surgical results of adjustable and conventional techniques were compared at postoperative day 1, 1 and 3 months after surgery, and the last visit. On postoperative day 1, the overall success rates for adjustable and non-adjustable sutures were 90.3% and 57.2%, respectively. The success rates for each group were as follows: on postoperative day 1 ET adjustable, 89.3%; ET non-adjustable, 61.2%; XT adjustable, 91.3%; and XT non-adjustable, 53.1%. The chi-square test revealed significant differences on postoperative day 1 (p=0.00 for ET, and p=0.01 for XT), which could not be detected at 1 and 3 months after surgery and the last visit for the ET group (p>0.05; Figures 1 and 2).
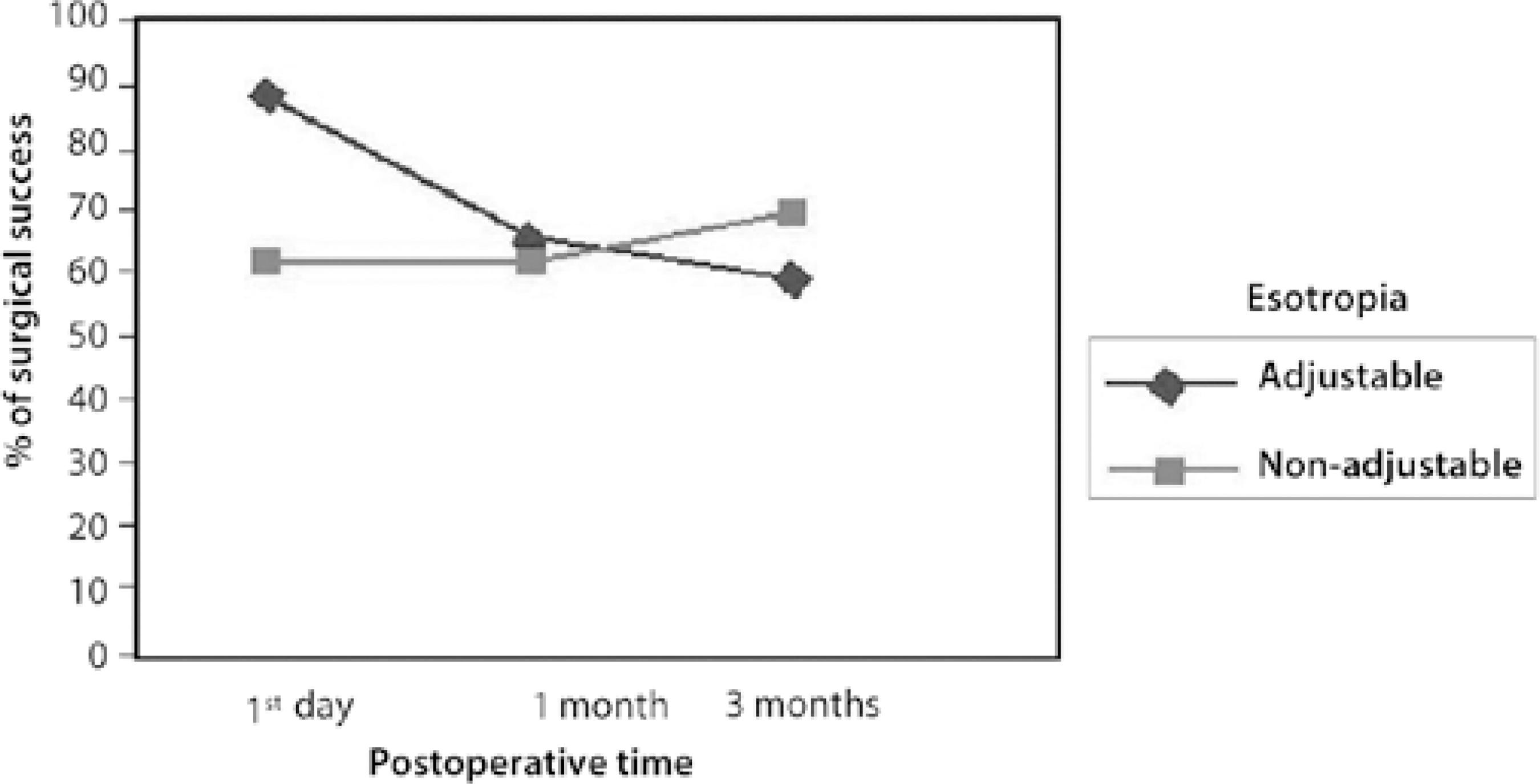
Figure 1 Surgical success at day 1st, 1 month and 3 months for patients with Esotropia, according to surgical technique.
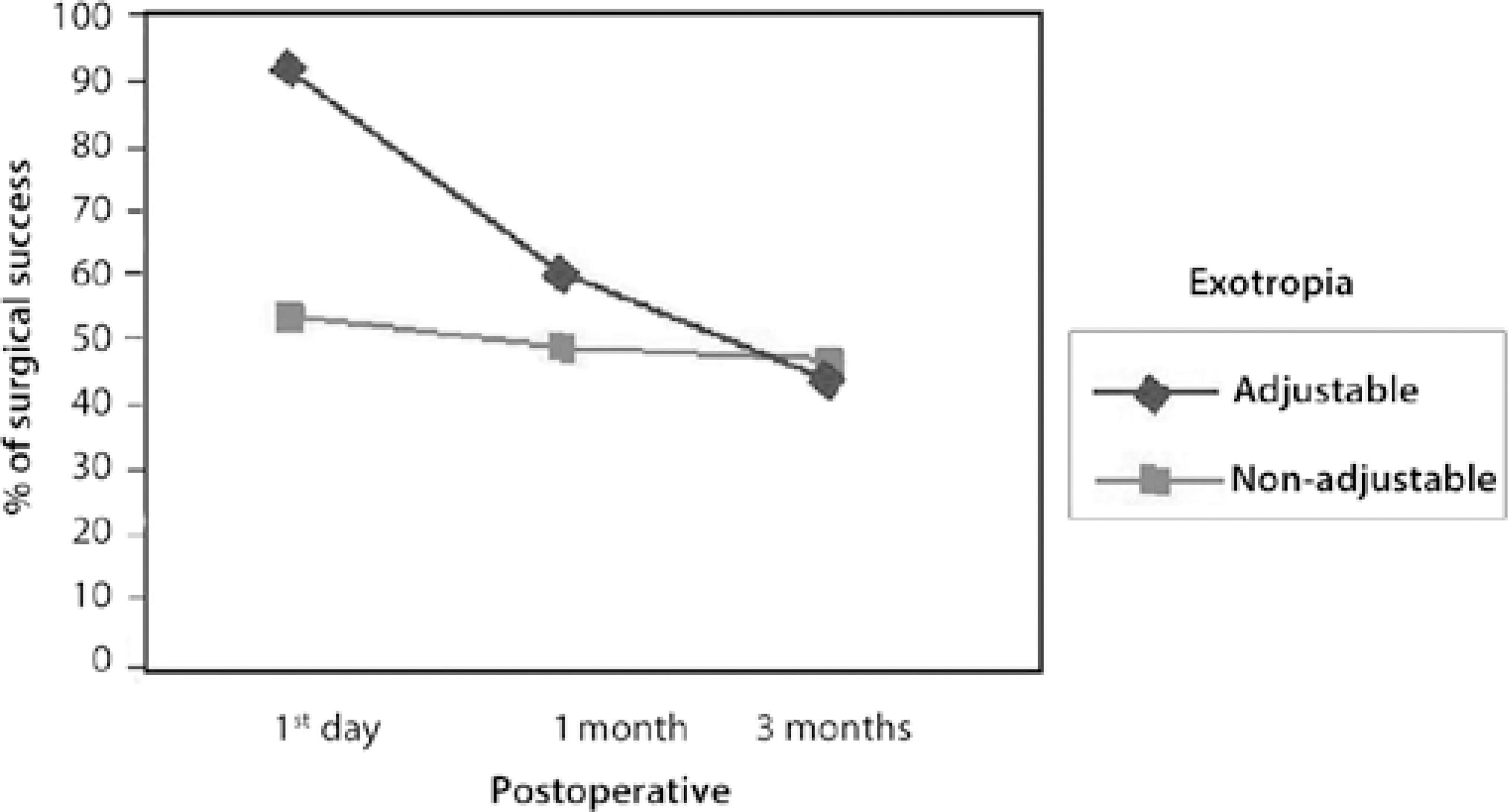
Figure 2 Surgical success at day 1st, 1 month and 3 months for patients with Exotropia, according to surgical technique.
For the XT group with a follow-up of at least 1 year, there were significant differences between patients undergoing adjustable and non-adjustable strabismus surgery: surgery was successful in 9/18 patients (50.0%) from the XT adjustable subgroup and in 5/23 (21.7%) from the XT non-adjustable subgroup (p=0.05); The chi-square test failed to show any correlation (p>0.05) between the presence of amblyopia and ametropia and surgical success at the last visit. No significant differences were found for ET patients with a follow-up of at least 1 year.
The relative risk of success at the last visit (non-adjustable/adjustable) was 0.96 for ET and 0.60 for XT. The pre-established parameter of 0.62 obtained during the pilot study correlates with the XT group results, although it indicates the need a larger sample of patients than that used for the ET group.
DISCUSSION
A historical or retrospective cohort was adopted for the present study to highlight the need of a reliable sample of patients whose selection followed strict inclusion and exclusion criteria(9). According to Weston et al.(10) and Wisnicki et al.(11), the success rate among adjustable suture surgeries is lower in patients previously operated on to correct ET and XT. Therefore, patients who had undergone previous surgeries were excluded from the present study to avoid the possibility of bias. In our study, the samples were uniformly distributed according to the frequency of amblyopia, angle of deviation, and preoperative follow-up. Consistent with the distribution of horizontal deviation in the general population, the ratio of ET cases to XT cases was 3:1 in the two groups.
An amblyopia rate >50% was present in all subgroups, indicating that the majority of the patients had little or no fusion capacity, unlike the patients presented by Pratt-Johnson in 1985(12), who included vertical deviations, paralysis, and reoperations, finding fusion ability in 40% of the patients. This is a potential reason for the lack of postoperative diplopia in XT patients who present with a slight overcorrection.
Deviations of up to 55 PD were included to compare between monocular and binocular two-muscle surgeries and to avoid large undercorrections and exaggerated adjustments, which could have distorted the results.
The mean age of patients undergoing operation with adjustable suture (22 years) was lower than that previously reported by Pratt-Johnson (33 years)(12). Mean age during surgery of the adjustable suture group was higher than that of the conventional group, which is consistent with previous studies and can be explained by the selection of cooperative patients(13). In our sample, 16 children (4-12 years old) underwent surgery with adjustable sutures under general anesthesia and were adjusted when necessary, without sedation. Chan et al. reported adjustable suture surgery in younger children(14). We found a higher rate of adjustments: 65.9% for ET and 56.5% for XT, compared with previous studies (around 40%)(10,12,15). The success rate for the adjustable surgery technique was 90.3%, which is similar to the rates described in the literature, which range from 67% to 90%(9,14-16).
The adjustable suture technique produced better surgical results than non-adjustable strabismus surgery for both the ET and XT groups on postoperative day one. At the last visit, the adjustable technique produced significantly better surgical results than the non-adjustable surgery for the XT subgroup. Mohan et al.(17) studied 38 patients with alternant exotropia equally allocated to adjustable and non-adjustable surgery and they found no statistically significant difference between the techniques at postoperative day 1 or at the last visit. The authors emphasized the need for a larger number of patients in each group. In 2009, Park et al.(18) could not show any significant differences between the results when comparing adjustable and non-adjustable surgery in the treatment of 54 patients with sensory exotropia. In a larger group comprising 370 patients with horizontal strabismus (primary and re-operation cases), Kraft et al.(19), found that XT patients who underwent adjustable surgery had a significant 15% in success rate compared to patients undergoing non-adjustable surgery.
The predominance of monocular surgery in both the adjustable and non-adjustable XT subgroups allowed for an equal distribution of characteristics such as hypercorrection, thereby avoiding biased information, which can occur in retrospective studies. The predominance of binocular surgery for the non-adjustable ET group and the presence of a high frequency of amblyopia, may have interfered negatively in the comparison with the ET adjustable group, predominantly representing of monocular surgery.
The results of the adjustable suture technique appear to be more effective when the recess-resection technique is employed. This technique places the recessed muscle under tension, which allows it to slide backwards when released during the adjustment.
We believe, based on our findings, that if a surgeon's goal is to obtain 5 to 10 PD hypercorrection postoperatively in XT patients, this could possibly be more easily obtained with adjustable sutures. The high amblyopia rate in our sample (>50%) could explain the need for minor hypercorrection during the immediate postoperative period for XT patients in order to minimize the risk of poor long-term surgical results in patients with no fusion ability.
Considering the lack of randomized control trials(7), we think that the present study will contribute significantly to the field, presenting a comparison of adjustable with non-adjustable sutures for horizontal strabismus using probabilistic sampling, rigid exclusion criteria, and homogeneous distribution of bias.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

