INTRODUCTION
Eyes are the third most frequently affected organ by trauma, after hands and feet(1). The incidence of traumatic globe dehiscence after penetrating keratoplasty (PK) has been reported to be 0.6%-5.8%(2). Any globe is susceptible to rupture and will do so at its weakest point if subjected to enough force(3-5). Keratoplasty exposes patients to a higher risk of globe rupture because the surgical wound may never regain the strength and stability of an intact cornea.
In this study, the authors present their experience with 11 cases of traumatic graft dehiscence after PK or deep anterior lamellar keratoplasty (DALK) as seen at the Brasilia Ophthalmologic Hospital (HOB), Brasilia, Brazil, from January 2004 to December 2012.
METHODS
This study is a retrospective, noncomparative, and interventional case series. All cases of traumatic wound dehiscence (WD) treated in the HOB were identified from the records of the only surgeon performing regular PK and DALK in this hospital from 2005 through 2013. PK was performed in 5 eyes (45.5%), and DALK was performed using the big-bubble technique in 6 eyes (54.5%). All eyes were phakic before the trauma. No intraoperative microperforation had occurred previously in the DALK patients. Cases of WD caused by infection or suture manipulation, such as adjustment or removal of sutures, were excluded. All patients received immediate surgical intervention within several hours after admission. Subsequent secondary surgeries, if any, were noted.
The study was performed according to established ethical standards for clinical research and was approved by the Institutional Review Board (IRB) of the Brasilia Ophthalmologic Hospital, Brazil. Demographic and surgical details were recorded, including the indication for keratoplasty, time from keratoplasty to WD, extent of the WD, associated ocular complications, and the visual outcome after surgical repair.
All data analyses were performed using SPSS statistical software (version 17.0, SPSS, Inc, Chicago, Illinois, USA). Quantitative data are presented as the mean ± standard deviation (range). The Mann-Whitney test was employed to compare the preoperative and postoperative visual acuities. Differences were considered statistically significant when the p value was <0.05.
RESULTS
Our hospital surgeons performed 471 keratoplasties during the 8-year study period, and eleven eyes (2.33%) in this group subsequently presented with globe rupture. Table 1 shows the demographic data for the 11 patients with globe rupture. The study included 11 eyes of 11 patients, of which 8 (72.7%) were men. The mean patient age at the time of rupture was 31.1 ± 8.81 years (range, 17-44 years). The median interval between keratoplasty and globe rupture was 12.82 months (range, 3-33 months). The mean follow-up time after the repair surgery was 4.36 ± 2.5 years (range, 1-8 years). The most common indication for the original graft was keratoconus.
Table 1 Demographic and clinical data for eleven patients with traumatic wound dehiscence after corneal keratoplasty
| Case | Age (years) | Gender | Indication for keratoplasty | Type of keratoplasty | Interval between keratoplasty and wound dehiscence | Nature of trauma | Extent of wound disruption (quadrants) and other damage | BCVA before trauma | BCVA after rehabilitation | Follow-up (years) |
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 26 | M | KCN | DALK | 6 m | Deliberate blunt trauma (punched) | 2, lens and vitreous loss | 20/60 | 20/60 | 2 |
| 2 | 41 | M | KCN | DALK | 7 m | Hit with tennis ball | 2 | 20/80 | 20/100 | 3 |
| 3 | 33 | M | KCN | PK | 6 m | Finger poked into eye | 2 | 20/70 | 20/60 | 2 |
| 4 | 33 | F | KCN | PK | 23 m | Fall | 2 lens and vitreous loss | 20/20 | 20/200 | 4 |
| 5 | 44 | M | Corneal scar | PK | 17 m | Deliberate blunt trauma | 3 lens and vitreous loss and RD | 20/25 | 20/2000 | 8 |
| 6 | 39 | F | Corneal scar | PK | 10 m | Fall | 2 lens and vitreous loss | 20/50 | 20/50 | 6 |
| 7 | 28 | F | KCN | PK | 5 m | Accidental blunt trauma | 3 endophthalmitis, vitreous hemorrhage, and RD | 20/100 | NPL | 1 |
| 8 | 37 | M | HSK | DALK | 19 m | Accidental blunt trauma | 2 | 20/50 | 20/80 | 7 |
| 9 | 20 | M | KCN | DALK | 33 m | Fall | 1 | 20/30 | 20/50 | 8 |
| 10 | 24 | M | KCN | DALK | 12 m | Accidental blunt trauma | 1 | 20/80 | 20/60 | 4 |
| 11 | 17 | M | KCN | DALK | 3 m | Accidental blunt trauma | 1 | 20/300 | 20/50 | 3 |
M= male; F= female; KCN= keratoconus; HSK= herpes simplex keratitis; PK= penetrating keratoplasty; DALK= deep anterior lamellar keratoplasty; NPL= no light perception; RD= retinal detachment.
In all except 1 eye, globe rupture involved the graft-host junction. Three patients (27.3%) had dehiscence involving 1 quadrant, 6 patients (54.5%) had dehiscence involving 2 quadrants, and 2 patients (18.2) had dehiscence involving 3 or more quadrants. Descemet membrane perforation after DALK was observed in 4 eyes (66.6%).
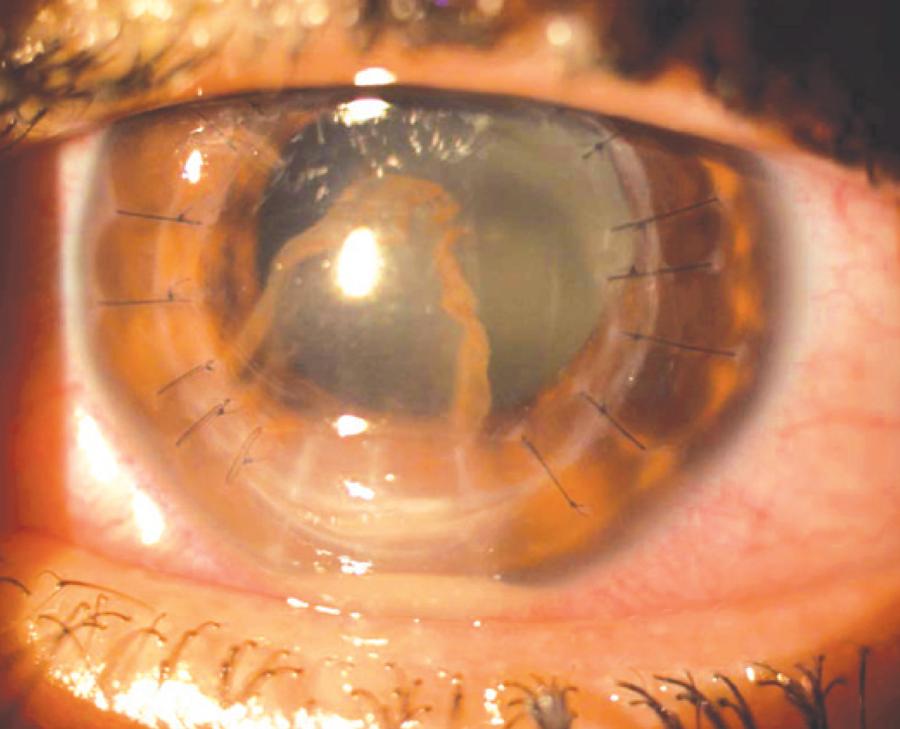
None of the patients were wearing protective eyewear at the time of trauma. Seven patients (63.6%) were using topical steroids at the time of WD. In all except 2 eyes, some or all of the sutures were present at the time of the trauma. In 4 eyes (36.4%), 3 of which underwent PK and 1 underwent DALK, the crystalline lens was expelled during trauma. Two patients (18.2%) experienced retinal detachment after WD. Three eyes (27.3%) were noted to have elevated intraocular pressure (defined as intraocular pressure >22 mmHg), requiring medical therapy. Only 1 patient developed endophthalmitis after WD (Figure 1).
The best-corrected visual acuity (BCVA) at the last visit before trauma ranged between 0.00 logMAR to 1.18 logMAR (mean, 0.48 logMAR). At the final visit after the surgery, the mean BCVA was 0.90 logMAR (range, 0.40 logMAR to no light perception). The difference between the mean BCVA at the last visit before trauma and the last visit after the repair surgery was not found to be statistically significant (p=0.15). At the last visit, 8 grafts (72.7%) were clear, 4 underwent secondary intraocular lens implantation for aphakia after the first surgical intervention, 2 (18.2%) experienced graft failure and the eye underwent repeat PK, and 1 eye (9.1%) developed phthisis bulbi.
DISCUSSION
WD is an unusual but serious complication of corneal keratoplasty. The wound healing occurs mainly at the endothelial and epithelial junctures. At the level of the stroma, the lamellar cut ends reconnect through a tangle of new collagen fibers, rather than through anastomosis(4). Various laboratory simulations and clinical and histopathological reports have shown that the cornea never regains its preoperative strength(5,6). The finding of a 2.33% incidence of WD after keratoplasty is approximately the same as that reported in other studies, in which the incidence has been reported to be 1.3-2.6%(6,7). Generally, WD after keratoplasty occurs early in the postoperative course(2,6-8). Our study supports this finding, with an average time between keratoplasty and ocular trauma reported as 12.8 months.
Most of the patients in our study were relatively young males with the mean age of 31 years, which was lower than that of patients in earlier investigations. The mean ages in studies by Williams et al.(7), Das et al.(9) and Renucci et al.(8) were 65, 55, and 69.5 years, respectively. Most of the young patients were males, similarly to what has been reported(7). Tseng et al.(10) also found a predominance of men in their series of traumatic WD cases and attributed their findings to the more physically active lifestyle of men.
Keratoconus was the most common indication for keratoplasty among the patients that experienced traumatic WD in this study. Other graft indications included corneal scar and herpes simplex keratitis. This is consistent with the most common indications for corneal transplantation performed in Brazil, in which keratoconus is the most common indication, followed by pseudophakic bullous keratopathy and corneal scar(11). In a study by Nagra et al.(12), the most common indication for PK among patients who developed WD was also keratoconus, followed by Fuch's endothelial dystrophy and pseudophakic bullous keratopathy. This is in contrast to the most common indication for corneal transplantation performed in the United States and United Kingdom, which is graft failure(13,14). Other indications include pseudophakic or aphakic bullous keratopathy, Fuch's endothelial dystrophy, keratoconus, and viral keratitis(13,14). In another retrospective case series of 19 traumatic dehiscence with corneal grafts that underwent repair In Australia, the most common indication for the original graft was keratoconus(9). The indication for the original keratoplasty is not considered to influence the risk of subsequent dehiscence. However, grafts for keratoconus are less likely to vascularize, a process that would probably strengthen the wound.
The most prevalent cause of trauma in our series was accidental blunt trauma (4 eyes, 36.4%). This reflects the younger ages of our patients who engaged in more social activities and were, therefore, more prone to ocular injury. Three patients sustained a fall from their own height, two received a deliberate blunt trauma (they were punched), and one was hit with a tennis ball. The force of the trauma was great enough to expel the lens through the WD in four eyes (36.4%), given that three had undergone PK and only one had undergone DALK.
In each of these cases the patient received primary resuturing of his corneal graft within several hours after the trauma. With follow-up varying from 1 to 8 years, the grafts remained clear in 8 eyes (72.7%). Other reports have found that WD after keratoplasty can be associated with a good visual outcome, depending upon the nature and severity of the wound disruption and the type of keratoplasty performed. Our series supports this finding. The difference between the mean BCVA at the last visit before trauma and the last visit after the repair surgery was not found to be statistically significant (p=0.15). Among patients with worsening of vision, the major cause of vision loss was posterior segment damage at the time of trauma. In 5 of 11 cases with posterior segment involvement, only one had undergone DALK, whereas the other 4 had undergone PK.
Although DALK offers advantages over PK, including less damage to the endothelium and fewer immunologic reactions, it has complications similar to that of PK. It is reasonable to assume that the intact Descemet's membrane provides reinforcement against dehiscing traumas after DALK surgery. However, a weakness at the graft-host junction seems to persist, and a severe deforming force can result in WD with lens and vitreous loss.
In summary, this study found that the risk of traumatic corneal graft rupture after keratoplasty is significant, even years after the surgery, and may cause a bad visual outcome depending upon the severity of WD. This should be clearly emphasized during preoperative counseling, particularly for young male patients. To minimize the risk of WD after keratoplasty, a thorough education of transplant candidates encouraging the use of protective eyewear and a low-risk lifestyle is warranted.




 English PDF
English PDF
 Print
Print
 Send this article by email
Send this article by email
 How to cite this article
How to cite this article
 Submit a comment
Submit a comment
 Mendeley
Mendeley
 Scielo
Scielo
 Pocket
Pocket
 Share on Linkedin
Share on Linkedin

